
Diagnosing Leprosy in Infants:
A Histopathological Challenge using Several Staining Technique
Joanne Natasha
1*
, Rizky L. Prayogo
1
, Michael H. Angriawan
1
, Rinadewi Astriningrum
1
, Melani
Marissa
1
, Sri Linuwih Menaldi
1
, Sondang P. Sirait
1
Department of Dermatology and Venereology, Faculty of Medicine Universitas Indonesia/
Dr. Cipto Mangunkusumo Central National General Hospital
*Corresponding author
Keywords: Leprosy, Histopathology, Infants, Stains
Abstract: Leprosy in infants is a rare case compared to adults. There is an excellent variety of the clinical cutaneous
finding in leprosy. Leprosy diagnostic is based on the classical cardinal signs, the presence of acid-fast
bacilli which is obtained by slit skin smear and skin biopsy. The gold standard to diagnose leprosy is the
identification of Mycobacterium leprae (M. leprae) bacilli using Hematoxylin and Eosin (H&E) and Fite
Faraco (FF) stains. Periodic acid-Schiff (PAS) and Gomori (Grocott) methenamine-silver (GMS), known to
give the positive result for fungal staining, revealed the other function is becoming the alternative staining
for M. leprae. Hereby, we report a case of a six-month-old male patient who presented unusual clinical
findings that were never considered as leprosy initially. Histopathological examination with several stains
was performed, and a diagnosis of lepromatous leprosy was obtained.
1 INTRODUCTION
The occurrence of leprosy during infancy is
uncommon. Infants are believed to be the most
vulnerable group to infection with M. leprae due to
their immature immunity and exposure to the
member of the family who has leprosy.(Narang T et
al., 2018) WHO data showed 210.671 newly
diagnosed leprosy cases during 2017, 16.979 were
children, represented almost 7,5% of all new cases
(5-14 years old).(Narang T et al., 2018) During
2002, based on the data, Indonesia has 21,2% (95%
CI: 12,5–29,9%) newly detected leprosy cases in
children 6-16 years old.(Bakker et al., 2002) Our
data showed 25 new cases leprosy in children (5-14
years old) from 150 patient’s visit in the
Dermatology Department of Dr. Cipto
Mangunkusumo Central National General Hospital
from 2017 to 2018, but none of them were infants.
The spectrum of leprosy in children or infants
has reported mostly to be tuberculoid (TT),
borderline tuberculoid (BT), mid-borderline (BB),
and indeterminate (I) forms. Lepromatous leprosy
(LL) type is rare in children or infants. The great
variety of presentations made the diagnosis of
leprosy a problematic challenge. The most likely
portal of entry is considered to be the upper
respiratory tract, but other possibilities through
direct contact. (Girdhar et al., 1989) Hematogenous
dissemination occurs in LL.(Sabin et al., 2005).
Leprosy diagnostic is based on the clinical
characteristics, finding acid-fast bacilli (AFB) in slit
skin smear, and histopathology. .(Narang T et al.,
2018). Hematoxylin and Eosin (H&E) and FF stains
are the chosen method for AFB staining. The other
study reported PAS and GMS stains could stain
Mycobacteria besides the previously known main
staining for fungal. Nevertheless, there is still
limited literature concerning the results of these
stains when applied to other Mycobacteria
species(Csillag, 1960;Wright et al., 2017;Schinietz
et al., 2018). We have recently highlighted the AFB
positive result by using PAS and GMS stains in the
case of an infant's LL. Hence, the use of these stains
may be considered to diagnose leprosy.
2 CASE
A six-month-old baby boy was consulted from the
Pediatric Department, on October 2018, with
290
Natasha, J., Prayogo, R., Angriawan, M., Astriningrum, R., Marissa, M., Menaldi, S. and Sirait, S.
Diagnosing Leprosy in Infants: A Histopathological Challenge using Several Staining Technique.
DOI: 10.5220/0009987002900294
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 290-294
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
complaints of erythematous collarette fine-scale
papules, plaque, and slightly nodules on the face,
chest, abdomen, arms, legs, buttocks and soles since
three months ago. The lesion was not accompanied
by pain. He was not seen scratching the lesion.
Alloanamnesis with the patient's mother, he had a
recurrent fever before the lesion appeared on the
skin. Pityriasis lichenoides chronica, atypical
pityriasis rosea, and psoriasis Vulgaris were initially
chosen to become the differential diagnosis based on
alloanamnesis and physical examination.
Skin biopsy was performed on November 2018
with a histopathological picture of granulomas with
numerous foamy cells in the lower dermis. There
were many vacuoles containing slightly grey-
basophilic colored material, including
polymorphonuclear (PMN), extravasation of red
blood cells, thickened vessel walls, and visible
granulomas surrounded nerves structures, suggesting
the diagnosis of lepromatous leprosy. Additional
staining using the FF, showed numerous AFB,
mostly in the solid forms. Periodic acid-Schiff and
GMS were also performed, gave a positive result for
bacilli inside the cytoplasm of foamy cells. Acid-fast
bacilli finding in histopathology was followed by slit
skin smears examination. This was obtained positive
on both ears, with 4/6 bacterial index and 0%
morphological index.
The patient was diagnosed with Severe
Combined Immune Deficiency (SCID) and
malnourished by the Pediatric Department since he
was five months old. He was the second child of two
siblings, with full-term delivery. He obtained
incomplete immunization. He lives in one house
together with his father, mother, mother's sibling,
and grandmother.
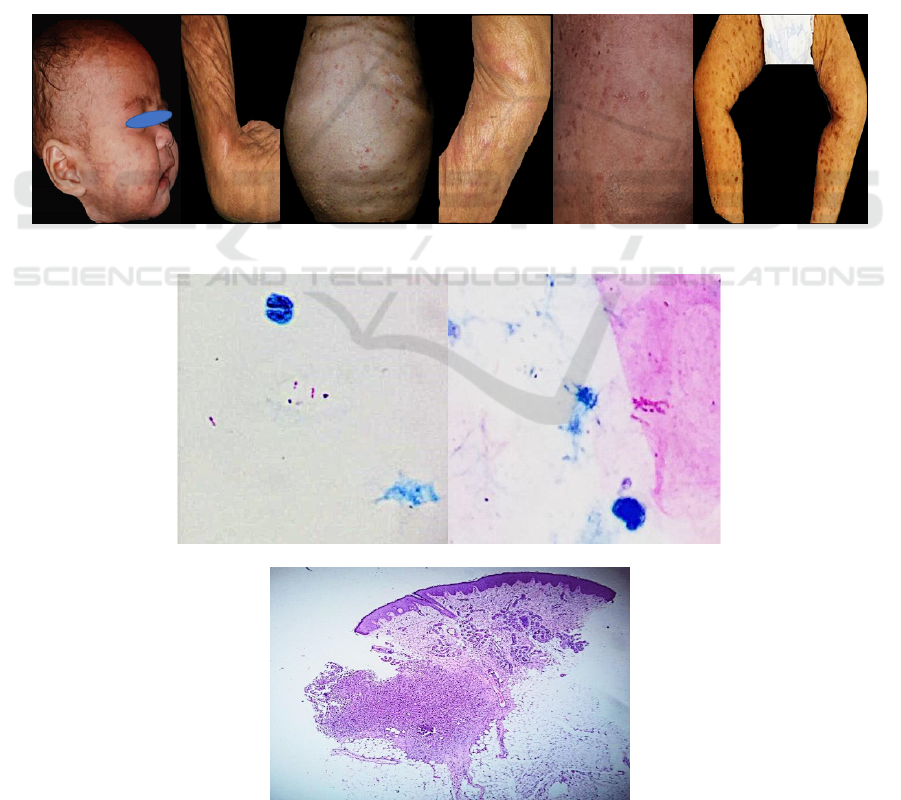
Figure 1. Erythematous to hyperpigmented papule-plaque-nodule with collarette scale in November 2018
Figure 2. Positive AFB on both ear lobes was revealed from slit skin smear
Figure 3. Histopathology, H&E staining, 100x, granuloma in the lower dermis
Diagnosing Leprosy in Infants: A Histopathological Challenge using Several Staining Technique
291

Figure 4. Histopathology, H&E staining, 400x (A), FF staining, 400x (B), PAS staining, 400x (C), GMS staining, 400x
(D). All shows numerous foamy macrophage containing globi of AFB. GMS and PAS show more bacilli than FF
3 DISCUSSION
Children or infants have a four-fold risk of
developing leprosy in the presence of leprosy close
contact in the neighborhood, and this risk increases
to nine-fold if there is a contact with leprosy patient
within the household. (Jain et al., 2014) The
occurrence of leprosy and its complication are
related to changes in the host’s immune response.
Individuals who are immunosuppressed could be
more at risk of developing leprosy.(Massone, 2012)
Individuals with sufficient exposure to M. leprae
may develop a broad range of clinical
manifestations. The bacillary proliferation and
hematogenous dissemination occur in LL. .(Sabin et
al., 2005).
Initially, the cutaneous lesion was confusing with
the other dermatological ailments. Several
differential diagnoses were chosen, but a primary
diagnosis was not established yet. The clinical
findings were never considered as leprosy, hence the
skin biopsy was done to obtain a definite diagnosis.
Papules, plaque, nodules skin lesions did not appear
as a typical lesion of leprosy, therefore slit skin
smear examination was done considering this infant
was not able having the nerve examination. The
result did not show globi as in the histopathology.
The number of AFB should be in the same quantity
as in the smear according to the bacterial index of
granuloma, such as +6 shows many clumps globi
(>1000 bacilli). (Massone, 2012). Possibly because
of the incision was not deep enough, since the
granuloma is in the deep dermis.
Leprosy diagnostic has generally been performed
based on a cardinal sign of clinical criteria
(anesthetic skin lesions, enlarged or thickened
peripheral nerves) and the presence of AFB from
tissue smears stained by modified Ziehl-Neelsen
staining. These great varieties of presentations in
infants made the diagnosis of leprosy as a challenge.
Histopathology is the gold standard to diagnose
leprosy, particularly in an early stage of leprosy. The
infant’s histopathology determined LL, in
accordance with nodular granuloma in the dermis,
macrophage cytoplasm were loaded with bacilli or
globi with large quantities of lipids, which on
staining give the appearance of foamy cells
(Virchow cells), and the infiltrate was separated
from the epidermis by collagenous fiber bands
(Unna band) giving the appearance of subepidermal
clear zone(Narang T et al., 2018;Weedon, 2012). In
a systematic review examined 24 children
histopathologically, the majority showed
characteristic features of BT leprosy (19/24), three
were BL leprosy, and two were indeterminate
leprosy. (Jain et al., 2014). Histological confirmation
is mandatory in all cases of leprosy because the gold
standard to diagnose leprosy is the identification of
M. leprae bacilli using H&E and FF stains. The gold
standard to diagnose leprosy is strictly related to
three significant points such as well done and deep,
6 mm punch biopsy performed at the right site of the
lesion, well-cut, stained H&E and FF slides, also
detailed clinical information. (.(Massone,
2012;Xavier Jnior JCC et al., 2016)
Job-Chacko modified FF staining for M. leprae
enables the better chance of detecting the bacteria in
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
292

the early leprosy granuloma. Histopathology, carried
out by FF staining, displays the sensitivity of 74,6%
and positive predictive value of 85,9% and negative
predictive value of 56,7%. This study shows that
diagnosis was revealed with FF staining, better than
other stain.(Reja AHH et al., 2013) Based on authors
experience and other literature, FF staining is often
negative even in multibacillary leprosy.(Adiga et al.,
2013;Joshi,2014)
Mycobacteria is challenging to demonstrate by
the Gram technique as they possess a capsule
containing a long-chain fatty acid (mycolic acid)
which makes them hydrophobic. Mycobacteria are
PAS-positive due to the carbohydrate content of
their cell walls. However, this positivity is evident
only when the large concentration of the
microorganisms are present. When these organisms
die, they lose their fatty capsule and consequently
their carbol fuchsin positivity. The carbohydrate can
still be stained by GMS reaction, which may prove
useful when acid-fast procedures fail, particularly if
the patient is already receiving therapy. These
organisms are acid- and alcohol-fast but are usually
easily identified as contaminants by their appearance
as clumps, or floaters.(
Morris GB et al., 2015)
Although GMS and PAS often used to identify
fungal infection, it is important to recognize their
other function of non-fungal staining in order to
obtain the correct diagnosis and guide appropriate
clinical management. Identified non-fungal
organisms, which are stained with GMS, include
parasitic worms, virally infected cells, acid-fast
bacilli, partially acid-fast bacilli, and non-acid-fast
bacteria. Gomori methenamine-silver and PAS
stains have also been reported to stain M.
leprae.(Xavier Junior JCC et al.,2013) In this case
report, GMS and PAS were useful to stain the bacilli
inside the foamy cells. Wright reported three of the
nine cases, which also revealed as non-fungal using
GMS and PAS stains. Organisms were not clinically
suspected as non-fungal. The non-fungal organisms
had silver deposition in varying locations including
the cell walls acid-fast Mycobacteria.(Wright et al.,
2017). In this case, histopathology showed more
numerous AFB in the cytoplasm of macrophage
foamy cells which were stained by GMS and PAS
compared to H&E and FF.
Gomori methenamine-silver is a chromic acid,
sodium bisulfate stain which precipitates silver ions
in fungal polysaccharide walls, producing the
characteristic black stain on light microscopy. This
is helpful to recognize aberrant GMS staining to
avoid misdiagnose of fungal elements. GMS stains
several non-fungal human pathogens which may be
useful diagnostic aid if the infectious condition is
not clinically suspected or the number of organisms
is sparse and having any difficulty to visualize with
routine staining methods.(Csillag, 1960). The other
study also reported the prominent PAS and GMS
positivity in a case of cutaneous Mycobacterium
avium complex (MAC) infection, and organisms
show the higher intensity of staining with GMS
compared to routine AFB staining. Strong staining
of M. tuberculosis and M. leprae has been reported
with GMS with a modified silver stain.
7
Periodic
acid-Schiff method selectively stains some
carbohydrates and carbohydrate compounds such as
glycogen, starch, mucin, and chitin. Csillag also
reported PAS-positive material, in all strain of
Mycobacteria. PAS-positive smears often contain
clearly distinguishable vacuolated cells, though
these might only be present in small numbers. The
reaction was strong and the material colored
intensely red, although the study did not include M.
leprae. In the challenging cases, as in this case,
clinical manifestation showed some variety of
unusual cutaneous lesion in an infant with
immunocompromised. Leprosy was initially
unexpected as the differential diagnosis. (Csillag,
1960).
4 CONCLUSION
In children, leprosy is dominated by borderline type
to tuberculoid type leprosy. Unusual case leprosy in
infant showed atypical cutaneous lesion. Hence
leprosy was not an unexpected differential diagnosis.
As seen in this case, the diagnosis of lepromatous
leprosy was established by histopathological
examination. Leprosy could be diagnosed by slit
skin smear and histopathology due to the difficulty
in conducting the sensitivity test, primarily in
children under ten years of age, and the need for
knowing other dermatoses commonly found in
childhood as the differential diagnosis. This case
was solved through the histological analyses using
leprosy routine stains and also alternative stains.
This case report showed that GMS and PAS were
also considered choices to stain AFB in leprosy
besides H&E and FF. Although GMS and PAS are
not specific for AFB, it can stain bacteria inside the
cytoplasm of foamy cells in leprosy.
REFERENCES
Adiga DSA, Hippargi SB, Rao G, Saha D, Yelikar BR,
Karigoudar M. 2016.Evaluation of fluorescent staining
for diagnosis of leprosy and its impact on grading of
Diagnosing Leprosy in Infants: A Histopathological Challenge using Several Staining Technique
293

the disease: comparison with conventional staining. J
Clin Diagn Res.10:23-6
Bakker MI, Hatta M, Kwenang A, Klatser PR, Oskam
L2002. Epidemiology of leprosy on five isolated
islands in the Flores sea, Indonesia. Trop Med Int
Health.;7:780-7.
Csillag A. 1960.Periodic acid-Schiff (PAS) staining of
“atypical” mycobacteria and tubercle bacilli. In:
Tubercle. vol 41. London: Elsevier. p.63-7.
Girdhar A, Mishra B, Lavania RK, Bagga AK, Malaviya
GN, Girdhar BK. 1989. Leprosy in infants report of
two cases. Int J Lepr Other Mycobact Dis.;57:472-5.
Jain M, Nayak CS, Chokkar R, Aderao R.2014.Clinical,
bacteriological, and histopathological characteristics
of children with leprosy: A retrospective, analytical
study in dermatology outpatient department of tertiary
care centre. Indian Journal of Paediatr
Dermatol;15:16-9.
Joshi R.2014. Limitations of histopathology in diagnosis
and management of patients with leprosy. Indian J
Dermatol Venereol Leprol;80:389-391.
Massone C. 2012. Histopathology of the skin. In: Nunzi
M, Massone C. Leprosy a practical guide. Austria:
Springer .p.115-36
Reja AHH, Biswas S, Dasgupta S, Chowdhury IH,
Banerjee S, et al.2013. Fite-Faraco staining in combination
with multiplex polymerase chain reaction: A new
approach to leprosy diagnosis. Indian J Dermatol Venereol
Leprol;79:693-700.
Sabin TD, Swift TR, Jacobson RR.2005. Leprosy. In:
Dyck PJ, Thomas PK. Peripheral neuropathy.4th ed.
vol 2. USA: Elsevier. p.2081-2108.
Schnietz R, Wilson ML.2018. Grocott methenamine silver
and periodic acid-Schiff positivity in cutaneous
Mycobacterium avium complex infection. J Cutan
Pathol.;45:551-3.
Wright AM, Mody DR, Anton RC, Schwartz MR. 2017.
Aberrant staining with Grocott’s methenamine silver:
utility beyond fungal organisms. JASC;1-14
Weedon D. 2010.Bacterial and rickettsial infections. In:
Weedon D. Skin's pathology. 3rd ed. China: Elsevier;.
p.562-6.
Xavier junior JCC, Ocanha JP, Marques MEA, Marques
SA.2016.Mycobacterium leprae is usually favorable to
periodic acid–Schiff and Grocott stains. Am J
Dermatopathol;38:322-4.
.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
294
