
Lupus Erythematosus Panniculitis: Clinical and Histopathological
Diagnostic Challenge
Vashty Amanda Hosfiar
1*
, Agung M. Rheza
1
, Sondang P. Sirait
1
, Eyleny Meisyah Fitri
1
,
Rahadi Rihatmadja
1
, Endi Novianto
1
1
Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia/
Dr. Cipto Mangunkusumo National Central General Hospital Jakarta
*
Corresponding auhtor
Keywords: Histopathology, Lupus Erythematous, Morphea, Panniculitis
Abstract: Panniculitis is the inflammation of subcutaneous fatthat sometimesassociated with connective tissue
diseases.One of the well-described forms of connective tissue panniculitis is lupus erythematosus
panniculitis (LEP). We report a 35-year-old female patient with skin atrophic lesions on the lateral aspect of
the upper arms and cheeks for at least 8-year duration. The atrophic lesions were followed by recurrent
multiple small nodules on the right jaw and neck, on which excisional biopsy was performed.
Histopathologyexamination revealed lobular panniculitis consistent with LEP. However, slight hyalinosis
and thickened collagen bundles were also observed that deep morphea could not be ruled out. The patient
was treated with hydroxychloroquine 200 mg/day and methotrexate 7.5 mg a week, showing improvement
by decreased ANA titer. No new nodules and enlargement of atrophic areas were found after the one-month
course of therapy.
1 INTRODUCTION
Inflammation of the subcutaneous fatknown as
panniculitis can be seen in many disorders, including
connective tissue diseases. Panniculitis occurring in
connective tissue diseases are lupus erythematosus
panniculitis (LEP), panniculitis associated with
dermatomyositis, morphea, and scleroderma, which
were also known as connective tissue panniculitides
and associated with autoimmune phenomena.(Gupta
P et al., 2016; Braunstein I et al., 2012)
LEP, or also
known as Kaposi-Irgang disease, is a rare form of
chronic cutaneous lupus erythematosus
characterized by inflammatory lesions in the lower
dermis and subcutaneous tissue,(Costner et al., 2012;
Aronson IK et al 2012).The most important
differential diagnosis of LEP is deep morphea.
Morphea or localized scleroderma is a chronic
autoimmune disease characterized by sclerosis of the
skin.(Costner et al., 2012; Saxton-Daniels et al.,
2012).Diagnosing panniculitis is often difficult due
toinadequate clinical details, overlapping clinical
and histopathological features, inadequate biopsy
specimens, and evolving morphology of different
types of panniculitides at different
stages.
1
Panniculitis associated with connective tissue
diseases resolves with depressed atrophic scar
leading to cosmetic disfigurement and decrease in
quality of life. (Braunstein I et al., 2012;Hansen CB
et al., 2010). report a case of connective tissue
panniculitis featuring atrophic lesions on upper arms
and cheeks for at least 8-year duration. Despite
previous histopathology evaluation, it was not
correctly diagnosed that definitive treatment had
been delayed leading to permanent atrophy. This
case report aimed to raise the awareness of the
entity, the importance of skin biopsy for diagnosis,
and prompt treatment to improve quality of life.
2 CASE
A 35-year-old female presented with skin atrophy on
the lateral aspect of the upper arms for 12 years and
cheeks for eight years. The lesions started as bluish-
red bumpswithout pain or itch. Over six months,
lesions progressed to atrophic scar with healthy
skinappearance. She also had suffered from a similar
process on her cheeks for eight years, followed by
272
Hosfiar, V., Rheza, A., Sirait, S., Fitri, E., Rihatmadja, R. and Novianto, E.
Lupus Erythematosus Panniculitis: Clinical and Histopathological Diagnostic Challenge.
DOI: 10.5220/0009986402720276
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 272-276
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
multiple small nodules on the right jaw and neck.She
underwent surgical excision and was diagnosed with
tuberculosis lymphadenopathy by an internist. She
was treated with a fixed-dose combination of anti-
tuberculosis drugs for six months, and the nodules
were improved.Over the past ten months, multiple
recurrent nodules had developed on the right neck.
She underwent fine-needle aspiration biopsy,
resulted as a benign submandibular lesion, and she
was referred to oncology surgeon in our hospital. An
excisional biopsy was performed, histopathology
and immunohistochemistry examination confirmed a
reactive polyclonal lymphoproliferativeprocess
(lymphocytes positive for CD30, CD20, CD138,
CD4, CD8, and Ki67 20% of a nucleus).She was
consulted to the hemato-oncology division and
dermato-allergo-immunology division.No history of
skin trauma, fever, malaise, weight loss, stomatitis,
joints, pain, or hair loss was found. There was no
history of malignancy or similar symptoms in the
family.
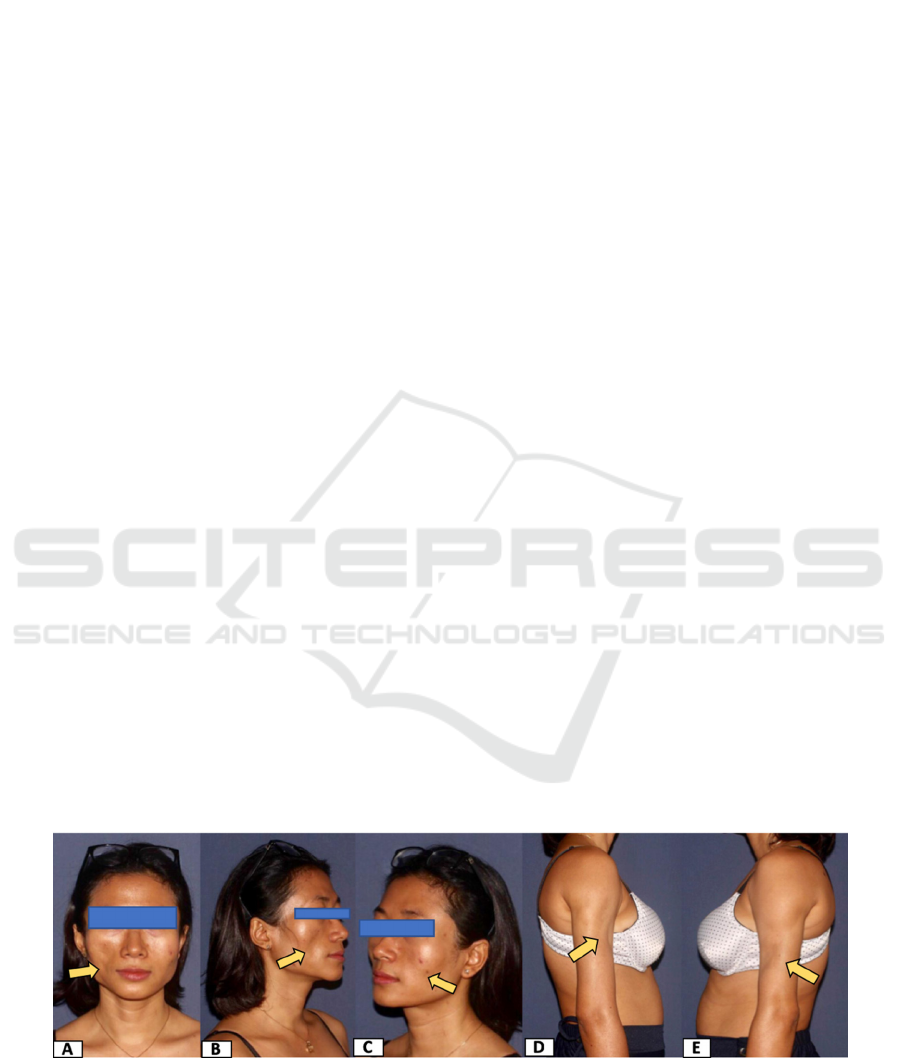
Physical examinations revealedmultiple atrophic
lesions on the cheeks and lateral aspect of the upper
arms with the normal skin surface. There were
twoimmobile and painless lymph node enlargement
in the neck and submandibular region, 1x1x0,5 cm
in size. Chest x-ray examination result was within
normal limits. Ultrasonography of neck showed right
mandible isoechoic lesion and partially bilateral
multiple conglomerated right intraparticle lymph
nodes.Level II right neck lymphadenopathy was
found in CT scan of the neck with contrast.
Laboratory test results showed normal levels of
complete blood count, renal and liver function tests,
but a decrease in vitamin D 25-OH level (21ng/dl).
HIV screening assays, HBsAg, anti-HCV, C3,
C4levels, and anti-dsDNA test were
negative.ANA1/1000, coarse speckled pattern,
possible antibodies on hnRNP, U1RNP, Sm, RNA
Polymerase III. Ro-52 recombinant borderline and
SS-B positive in ANA profile.
In the dermato-allergo-immunology clinic, patients
were suspected of LEP, different from the earlier
histopathologic result. So, we asked for a
reevaluation of the biopsy specimens to
dermatopathology division. Histopathology reading
revealed epidermal atrophy, vacuolaralteration, and
flattening of rete ridges; perivascular and
periadnexal lymphohistiocytic infiltrates forming
lymphoid follicles; and lymphohistiocytic infiltrates
among fat lobules which showed partial necrosis
with corresponding Touton giant cells, and
lipophage, supporting a diagnosis of LEP. Ziehl-
Neelsen, Periodic Acid-Schiff (PAS), and Gram
staining did not demonstrate acid-fast bacilli,
thickened basement membrane, and bacteria
respectively. However, as there was suspicion for
morphea, another reading was done that found what
was considered as hyalinized and thickened collagen
bundles. The diagnosis of LEP with deep morphea
as a differential diagnosis was made.
After confirming a normal glucose-6-phosphate
dehydrogenase (G6PD) level and no ophthalmic
contraindication to an antimalarial drug, the patient
began treatment with hydroxychloroquine 200 mg a
day and topical sunscreens. Later atone month
follow uplesions were stable without new nodules,
andANA titer decreased to 1/320. Methotrexate was
given in initial dose 5 mg a week, escalated to 7.5
mg a week accompanied with folic acid 5 mg a week
orally in addition to hydroxychloroquine.During the
last threemonths,the atrophic lesions were stable, no
new nodules were found, and multiple nodules on
the right neck decreased in size.
Figure 1. AE. Multiple atrophic lesions with normal skin surface (arrow).
Lupus Erythematosus Panniculitis: Clinical and Histopathological Diagnostic Challenge
273
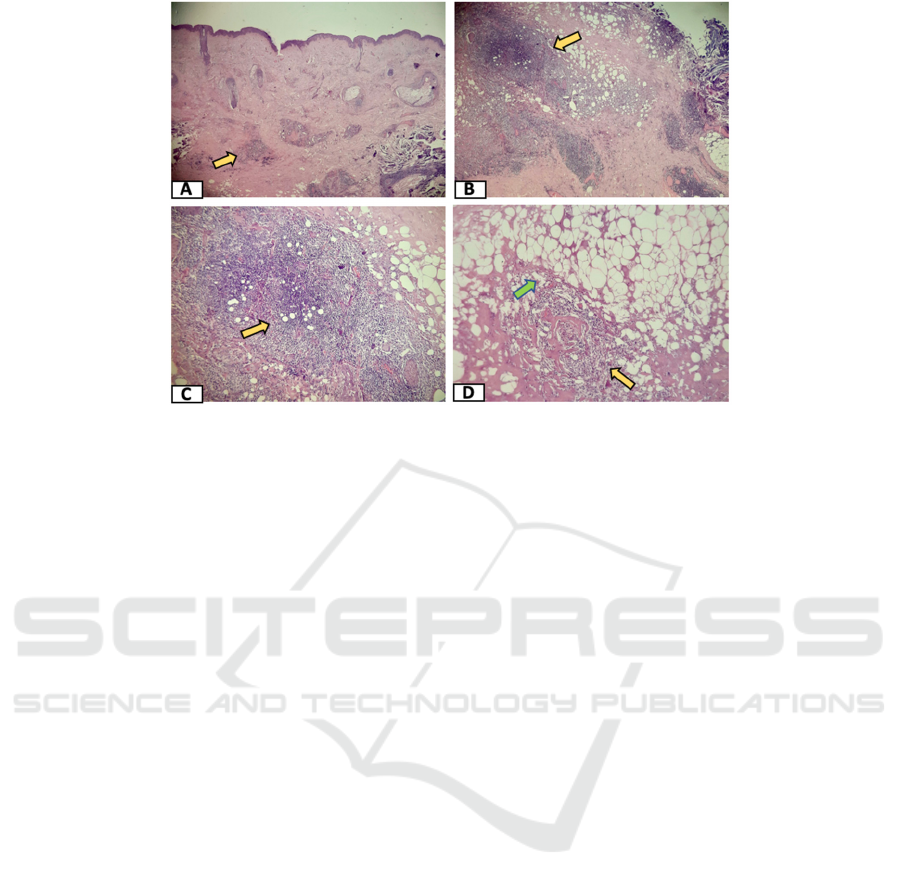
Figure 2. Histopathology with Hematoxylin-eosin (HE) staining A. HE,50x, perivascular and perifollicular
lymphohistiocytic infiltrates extending to the subcutis (arrow). B. HE, 100x, lymphoid follicles (arrow). C. HE, 400x,
lymphoid follicles (arrow). D. HE, 1000x, lymphohistiocytic infiltrates (yellow arrow) and fat lobules necrosis (green
arrow).
3 DISCUSSION
Panniculitisassociated with connective tissue disease
begins with active inflammation and develops into
atrophy, scar, and calcification.(Gupta P et al., 2016;
Braunstein I et al., 2012;Hansen CB et al., 2010)
.
Diagnosis of LEP and deep morphea as a differential
diagnosis were established based on clinical,
laboratory, and histological findings. LEP is
characterized by inflammatory of the lower dermis
and subcutaneous tissue, estimatedto comprise
13% of cutaneous LE cases. (Costner et al.,
2012;Aronson IK et al., 2012)
.
LEP lesions begin
with subcutaneous nodules without or with any
surface changes including erythema and discoid
lupus erythematosus (DLE) features. The most
common sites are on the lateral aspect of upper
arms, shoulders, face, scalp, hips, breasts, and
buttocks. The mean duration of the disease is
sixyears and resolves with depressed lipoatrophic
areas. (Aronson IK et al., 2012). Clinically, the
disease’s course and location in our patient matched
with those of LEP. Fifty percent of LEP patients
could develop systemic lupus erythematosus (SLE)
with mild manifestations. (Fett N et al.,
2011;Castrillon MA et al., 2017). On the other hand,
Deep morphea is a chronic autoimmune disease
characterized by skin sclerosis that involves the deep
dermis, subcutaneous tissue, fascia, and muscle.
5
Both diseases are more common in females aged
3060 years old and resolve with depressed atrophic
scar. (Costner et al., 2012; Saxton-Daniels et al.,
2012; (Fett N et al., 2011)
.
Serologic analysis for LEP are often normal, and
sometimes variable positive ANA titer demonstrated
ranging from 2795,4% of cases. Less frequently,
anti-ds-DNA antibodies are present. (Aronson IK et
al., 2012; Castrillon MA et al., 2017;Zhao YK et al.,
2016)
In our patient, the laboratory showed ANA
titer 1/1000. However, anti-dsDNA is not present.
Positive ANA could also be found in 3980%
morpheawith speckled pattern (81%) andtiter
>1/1280. (Saxton-Daniels et al., 2012;Teke MN et
al., 2017)
The gold standard of LEP diagnosis is the
histopathology examination result from a deep skin
biopsy of the lesional area.(Castrillon MA et al.,
2017;Bednarek A et al., 2015).The histopathological
finding of LEP shows mostly lobular or mixed
panniculitis with a variable lymphocytic infiltrate.
Meanwhile, panniculitis on deep morphea is
predominantly septal. (Gupta P et al., 2016;
Bednarek A et al., 2015)
.
In our patient, the
important findings included lymphoid follicles (that
lead to the previous diagnosis of lymphoproliferative
disorder), necrosis of fat lobules, and what was
thought later to be hyalinized and thickened collagen
bundles. With these overlapping clinical and
histopathological features, diagnosis in our case was
made with a degree of uncertainty. Lipoatrophic
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
274
panniculitis is a diagnosis of exclusion that requires
evaluating for other causes of panniculitis. (Aronson
IK et al., 2012; Hansen CB et al., 2010). In our
patient, laboratory findings within normal limits and
staining for Ziehl-Neelsen, Periodic Acid-Schiff
(PAS), and Gram examination were used to
eliminate infection, all returned negative. The
differences between LEP and deep morphea are
depicted in Table 1.
As immunohistochemistry examination confirmed a
reactive polyclonal lymphoproliferative disease,
another important differential diagnosis is
subcutaneous panniculitis-like T-cell lymphoma
(SPTCL), a lymphoma whose origin is from mature
cytotoxic T cells.(Sugeeth et al., 2017;Lerma IL.,
2018;Arps DP et al., 2013).
As lymphocytes were
positive for CD3, CD4, CD8, and CD20 (B cells
marker) in our patient, SPTCL were excluded.
Antimalarial drugs such as hydroxychloroquine or
chloroquine are usually the first-line treatment for
LEP. Antimalarials interfere with inflammatory
cytokinesas well as TLRs, requiring at least three
months to show effectiveness. (Costner et al.,
2012;Aronson IK et al., 2012).
The patient has
treated with hydroxychloroquine 200 mg a day with
good response, shown by decreased ANA titer from
1/1000 to 1/320, no new nodules or enlargement of
atrophic lesion found after a month. Since
methotrexatewas recommended as a first-line
treatment for morphea with dermal and
subcutaneous involvement,
five
we also added
methotrexate to previous hydroxychloroquine
treatment.
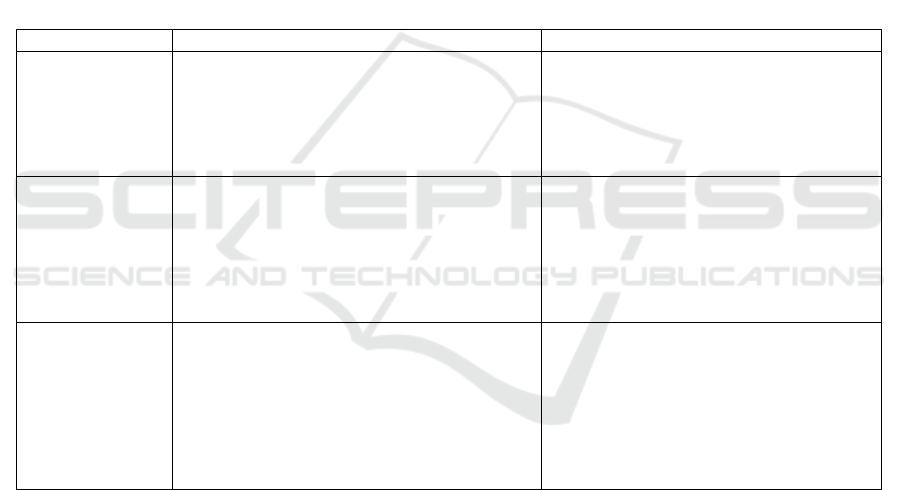
Table 1.Summary of clinical features, laboratory findings, and histopathology in LEP and deep morphea. Bold words are
found in our patient
Characteristics LEP Deep morphea
Clinical features - Subcutaneous nodules without or with any
surface changes.
- Location: lateral aspect of upper arms,
shoulders, face, scalp, hips, breasts, and
buttocks.
- Resolve with atrophic scarring.
- Sclerotic plaque with hyperpigmented,
ill-defined, or mildly inflamed.
- The skin feels bound down to the
underlying fascia and muscle.
- Resolve with atrophy,
hyperpigmentation, or discoloration.
Laboratory
findings
- The serologic analysis is often normal.
- Positive ANA titer ranging from 2795,4%.
- Anti-ds-DNA antibodies are less frequently
present.
- Serologic analysis: peripheral
eosinophilia, hypergammaglobulinemia,
and raised ESR.
- Positive ANAcan be found.
- Other autoantibodies: Anti ds-DNA, anti-
histone, anti-Scl-70, and rheumatoid
factor.
Histopathology - Predominantly lobular panniculitis or mixed
panniculitis.
- Variable lymphocytic infiltrate, lymphoid
follicles, and hyaline fat necrosis.
- Other characteristics: DLE-like changes in
epidermis, dermo-epidermal changes,
mucin deposition, granuloma formation,
plasmacytic infiltration, and calcifications.
- Predominantly septal panniculitis.
- Lymphocyte and plasma cell infiltration
and collagen tissue thickening and
hyalinization in the subcutis.
- Occasionally, lymphoid follicles devoid
of germinal centers.
- Lipophagic granuloma also may be
present in the fat lobules.
4 CONCLUSION
Diagnostic of panniculitis poses achallenge due to
various factors. Many conditions that could cause
panniculitis to need to be excluded. Histopathology
examination from a deep skin biopsy is still
remained to be the gold standard. Clinical and
serologic characteristics should always be weighed
in for a final diagnosis.Particularly in LEP,early
diagnosis and appropriate therapy should be
considered to prevent disfigurement and progression
to systemic involvement.
REFERENCES
Arps DP, Patel RM. 2013. Lupus profundus (panniculitis):
a potential mimic of subcutaneous panniculitis like T
cell lymphoma. Archives of pathology and laboratory
medicine.;137:1211-15.
Aronson IK, Fishman PM, Worobec SM. Panniculitis. In:
Goldsmith LA, Katz SI, Gilchrest BA, Paller AS,
Leffell DJ, Wolff K, eds. 2012.Fitzpatrick's
Dermatology in General Medicine. 8th ed. New York:
McGraw Hill;. p.732-54.
Lupus Erythematosus Panniculitis: Clinical and Histopathological Diagnostic Challenge
275

Bednarek A, Bartoszak L, Samborski W. 2015.Case report
on a patient with lupus panniculitis. Postep Derm
Alergol.;32(1):59-62.
Braunstein I, Werth VP. 2012.Update on management of
connective tissue panniculitides. Dermatol
Ther.;25(2):173-82.
Castrillon MA, Murrell D.2017. Lupus profundus limited
to a site of trauma: case report and review of the
literature. International Journal
Costner MI, Sontheimer RD. Lupus erythematosus. In:
Wolf K, Goldsmith LA, Kath SI, Gilchrest BA, Paller
AS, Leffel DJ, eds. 2012.Fitzpatrick’s Dermatology in
General Medicine. 8th ed. New York: Mc Graw Hill;.
p.1909-26.
Fett N, Werth VP.2011.Update on morphea: part I.
Epidemiology, clinical presentation, and
pathogenesis.J Am Acad Dermatol;64(2):217-28
of Women’s Dermatology. 2017;3(2):117-20.
Hansen CB, Callen JP. 2010. Connective tissue
panniculitis: Lupus panniculitis, dermatomyositis,
morphea/scleroderma. Dermatol ther.;23:341-349.
Gupta P, Saikia UN, Arora S, De D, Radotra BD.2016.
Panniculitis: a dermatopathologist’s perspective and
approach to diagnosis. Indian Journal of
Dermatopathology and Diagnostic Dermatology.;3:29-
41.
Bednarek A, Bartoszak L, Samborski W. 2015. Case
report on a patient with lupus panniculitis. Postep
Derm Alergol.;32(1):59-62.
Saxton-Daniels S, Jacobe HT. Morphea. In: Wolf K,
Goldsmith LA, Katz SI, Gilchrest BA, Paller AS,
Leffel JD, editor. 2012. Fitzpatrick’s dermatology in
general medicine. 8th ed. New York: McGraw-Hill;.
p.692-701.
Sugeeth MT, Narayanan G, Jayashuda AV, Nair RA).
2017.Subcutaneous panniculitis-like T-cell lymphoma.
Proc (Bayl Univ Med Cent;30(1):76-77.
Teske MN, Jacobe HT. Morphea (Localized Scleroderma).
In: Varga J, Denton CP, Wigley FM, Allanore Y,
Kuwana M, 2017 editor. Scleroderma from
Pathogenesis to Comprehensive Management. 2nd ed.
Switzerland: Springer;. p. 91-113.
Zhao YK, Wang F, Chen WN, Xu R, Wang Z, Jiang YW,
et al. 2016. Lupus panniculitis as an initial
manifestation of systemic lupus erythematosus: a case
report. Md Journal.;95(16):1-5.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
276
