
Generalized Pustular Psoriasis in Childhood
with Exogenous Cushing’s Syndrome
Fitri Azizah
1*
, Yusnita Rahman
1
, Rahadi Rihatmadja
1
,Triana Agustin
1
,
Rinadewi Astriningrum
1
, Githa Rahmayunita
1
1
Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia/
Dr.CiptoMangunkusumo National General Hospital, Indonesia
Keywords: Pustular Psoriasis, Childhood, Cushing’s Syndrome, Steroid Misuse
Abstract: Pustular psoriasis is characterized clinically by yellowish sterile pustules surrounded by erythema. Pustular
psoriasis in children is very rare and could be appear following steroid withdrawal in psoriasis vulgaris.
Psoriasis in children usualy mild and can be managed with topical treatment, which is considered as the first-
line therapy. Misuse of topical and systemic steroid in children could lead to Cushing’s syndrome. It is a
multisystem disorder resulting from prolonged exposure to excess glucocorticoids, both systemic or topical.
Children could easily develop systemic reactions to topical steroids due to their higher ratio of total body
surface area to body weight. Here we reported a case of generalized pustular psoriasis (GPP) in a 14-year-old
girl who had suffered from Cushing’s syndrome due to misuse of oral and topical steroid.
1 INTRODUCTION
Since the introduction in 1950s, topical steroids have
become the most commonly prescribed drugs by
dermatologists in outpatient setting. Used properly,
they are safe and effective, with minimal side effects.
Easy access to the drugs and practice of self-
medication has resulted in widespread misuse of
topical corticosteroids.(Meena S et al., 2015) In case
of childhood psoriasis, topical corticosteroids
remained the first line therapy and majority of
children can be managed only with topical treatment.
(Bronckers et al., 2015) Excess intake of
glucocorticoids, either systemic or topical could lead
to Cushing’s syndrome, which characterized
clinically by moon face, appearance of dorsocervical
and supraclavicular fat pads (buffalo hump), and
stretch marks. Cushing’s syndrome in children could
also manifests as growth deceleration.(Stratakis
CA,2018)
Over the last 35 years, there are 43 cases reported
of iatrogenic Cushing’s syndrome due to misuse of
very potent topical steroid usage in children and adult,
particularly in developing countries. The most
common purpose of steroid use in the children group
is infants with diaper dermatitis and in adult group is
psoriasis.(Sahana PK et al., 2015). Pustular psoriasis
is a rare disease, especially in children. Patients with
the generalized type of von Zumbuschs and
erythroderma have higher risk of mortality due to
systemic involvement. Few complications of
generalized pustular psoriasis (GPP) are septicemia,
hyperthermia, liver damage, and acute renal failure.
(Al Aboud DM et al., 2019) Psoriasis vulgaris can
either progressed into generalized pustular psoriasis
or appear after pustular psoriasis. Various
precipitating factors have been reported to trigger or
flare acute generalized pustular psoriasis, including
corticosteroid use and withdrawal. (Al Aboud DM et
al., 2019) Here we reported a case of exogenous
Cushing’s syndrome resulting from years of topical
and oral corticosteroids misuse in a pustular psoriasis
patient.
2 CASE
A 14-year-old girl came to our outpatient clinic 5
months agowith generalized erythematous plaques
worsening3 months prior to admission. Her lesions
first appeared when she was 4-year-old and was then
self-treated with various ointments. The plaques
never fully subsided until approximately 5 years later.
Inthe age of 11, she had her first menstrual period and
the lesions flared up all over her body and scalp.Her
262
Azizah, F., Rahman, Y., Rihatmadja, R., Agustin, T., Astriningrum, R. and Rahmayunita, G.
Generalized Pustular Psoriasis in Childhood with Exogenous Cushing’s Syndrome.
DOI: 10.5220/0009986002620266
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 262-266
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
mother usually bought so-called bitter antipruritic
pills from pharmacy to relieved her of the
symptoms.She continously took the medication
everyday for almost a year. The plaques recurred
temporarily and she had never had her period again
since 4 years ago.A year ago, the lesions flared up
again and she bought very potent topical steroidto
apply all over the body twice daily for about 7
months. Her lesions were not improving so she went
to a dermatologist 8 months ago and was sent for
biopsy. The histopathologyresult was psoriasis. She
was then given 8 mg methylprednisolone twice daily
along with 10 mg cetirizine and mometasonefuroate
cream. In 2018, she had topical steroids for almost 10
months and oral steroids for around 3 months.
At the time she went to our outpatient clinic, she
had moon face, her body weight was 46 kgs andher
height was only 137 cm which was short for her age
(BMI 24.5). Her skin was thin along with multiple
red-purple striae all over her body. She also had an
ulcer from a previous motorcycle accident which did
not heal completely. Multiple erythematous scaly
plaques were found on her scalp, neck, back, and
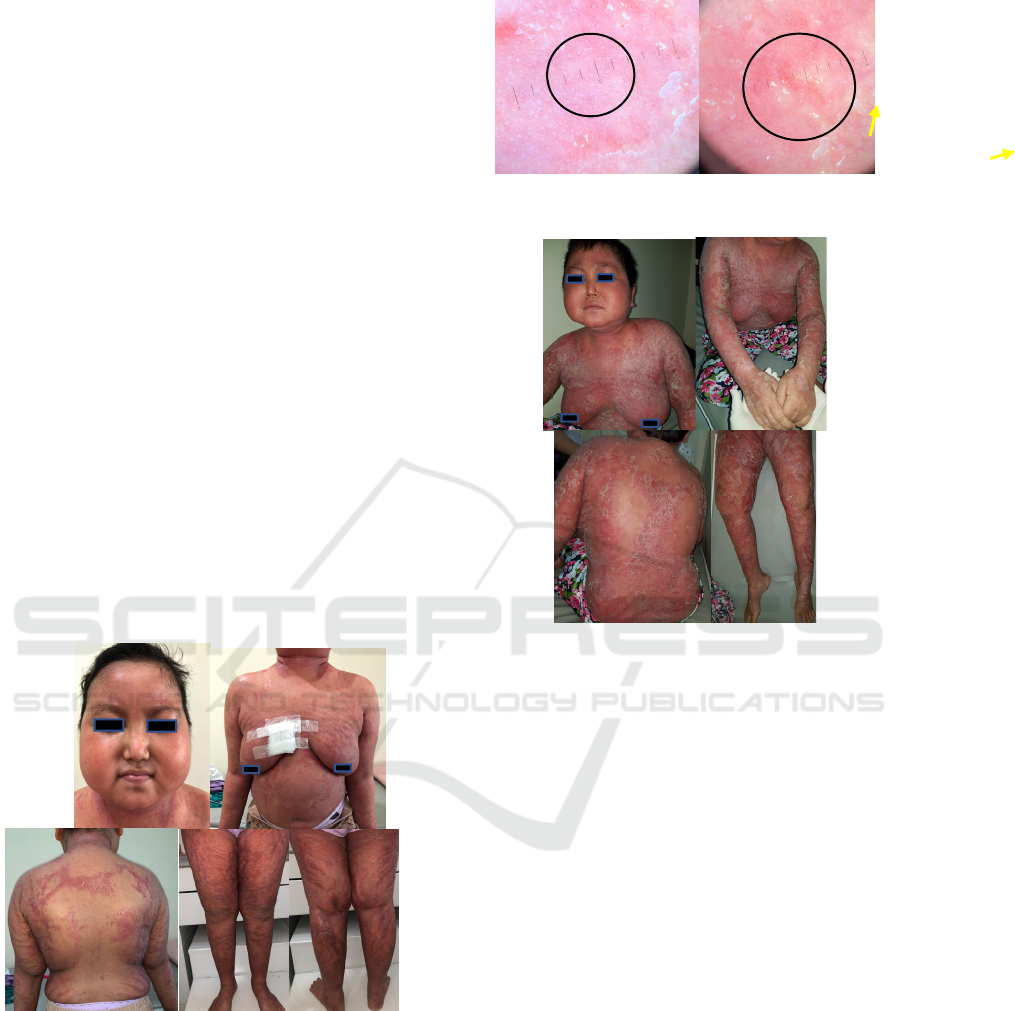
thighs (Figure 1). Dermoscopic findings show regular
dotted vessels distributed uniformly across the plaque
along with white scales (Figure 2). On her first visit,
we tapered off the oral and topicalsteroid.
Figure 1.Moon face, striae, and erythematous plaques with
scales.
Figure 2.Dermoscopy showed regular dotted vessels
(black circle) and white scales (yellow arrows).
Figure 3.Erythroderma with multiple pustules,lake of pus,
and yellow crust.
Until one month later she could not came back to our
outpatient clinic. Her medication ran out for the past
one week, both oral and topical steroid. Four months
ago, she was admitted to the emergency unit with
generalized erythematous plaques and multiple
pustules with lake of pus and yellow crust (Figure 3).
She was moderately ill and tachycardic but without
any fever. Her laboratory studies showed elevated
white blood cell count of 16,400/µL, low morning
cortisol level of 1.5 µg/dL (3.7 – 19.4), and normal
level of liver and kidney function. She was given 50
mg cyclosporine twice daily and a change course of
oral steroid to hydrocortisone under pediatric
endocrinologist’s supervision. She had
hydrocortisone 40-40 mg and 40-20 mg, every other
day and a decrease of 25% of her dose each week was
planned to tapered off. She also had petroleum jelly
and coconut oil for her scalp.
After two to four weeks of 100 mg cyclosporine
per day, her lesions were getting better but then she
experienced a flaredup which was suspected from
stress due to her school’s exam.After two months of
treatment, her lesions were not fully subsided so her
dose was titrated to 125 mg/day and her condition has
Generalized Pustular Psoriasis in Childhood with Exogenous Cushing’s Syndrome
263

improved a lot up until now (Figure 4).Currently her
oral steroid is still tapered off, changing back to
methylprednisolone 3 mg and 2 mg every other day.
Her gynecology ultrasound revealed uterus and
ovarium hypoplasia and low level of LH 0.8 mIU/mL,
normal level of FSH 6.7 mIU/mL, normal level of
estradiol 16.6 pg/mL, and normal level of anti
Mullerian hormone 1.39 ng/mL. She still has not had
her period and currently on obstetrician-gynecologist
supervision because her clinical and laboratory
studies did not add up.
Figure 4. Improvement in both moon face and skin lesions
after 3 months.
3 DISCUSSION
Pustular psoriasis is characterized clinically by
widespread yellowish sterile pustules surrounded by
erythema. The acute generalized type (von
Zumbusch) usually presents with systemic symptoms
and might evolve into erythroderma.(Al aboud DM.,
2019). Pustular psoriasis in children is very rare,
according to a review from Australia, there were only
0.6% cases with pustular variants in 1262 childhood
psoriasis patients.(Wang Q, 2017). Various
precipitating factors have been reported to trigger
acute generalized pustular psoriasis, including
corticosteroid use and withdrawal. (Hyde K et al.,
2016). Cutaneous lesions characteristics of psoriasis
vulgaris can be present before, during, or after an
acute pustular episode. In childhood psoriasis,
majority of children can be managed only with topical
treatment, such as topical steroids. .(Bronckers et al.,
2015) But when stopped abruptly after long period of
usage, corticosteroids withdrawal could triggered the
flare of generalized pustular psoriasis. In our case,
initially she had psoriasis vulgaris but later developed
generalized pustular psoriasis when her medication
stopped.
Misuse of topical steroids in children could easily
lead to systemic reactions because of their higher
ratio of total body surface area to body weight.
Topical corticosteroids were easily absorbed through
normal intact skin. Damaged or inflamed skin may
increase percutaneous absorption of the drug.
Application of steroids to large surface areas,
occlusion, vehicle, location of application, and more
potent derivatives such as clobetasol propionate,
directly increase the risk of hypotalamic-pituitary-
adrenal (HPA) axis suppression.
8
As little as 2 g/day
of clobetasol propionate 0.05% cream can cause a
decreased morning cortisol level after only a few
days.(Hengge UR et al., 2016). (Rahmayunita G et
al.,2008) reported a case of Cushing’s syndrome due
to misuse of topical steroid in a childhood psoriasis
but fortunately the patient was able to recover from
Cushing’s syndrome completely only with permanent
striae. In childhood, the characteristics of Cushing’s
syndrome are truncal obesity, growth failure, striae,
hypertension, appearance of dorsocervical and
supraclavicular fat pads, and moon face. Clinically,
there is no difference between exogenous or
endogenous Cushing’s syndrome. (Stratakis
CA,2018;Lodish MB et al., 2018). Hypercortisolism
is also associated with bone age advancement and
premature epiphyseal maturation. Decreased bone
mineral density, osteoporosis, and related fragility
fractures have been reported in in almost 60%
patients with glucocorticoid excess.(Raff H et al.,
2014). The likelihood of catch up growth after the
cure of Cushing’s syndrome depends on bone age
advancement at the time of diagnosis, but final height
in patients with Cushing’s syndrome in childhood is
known to be compromised. (Raff H et al., 2014). Our
patient had low morning cortisol level, moon face,
striae, growth retardation, and secondary amenorrhea.
High cortisol levels could supress gonadotropin
releasing hormone (GnRH), luteinizing hormone
(LH), and follicle stimulating hormone (FSH) release
thus ended in amenorrhea. (Raff H et al., 2014). Due
to the inconsistent laboratory and clinical data, our
patient is currently planned to have more diagnostic
tests.
To slowly tapered down exogenous steroids, our
patient was given hydrocortisone by pediatric
endocrinologist from Department of Child Health.
Hydrocortisone are the least potent glucocorticoids
but with the highest mineralocorticoid property.
Thus, hydrocortisone and cortisone are generally
preferred for use in patients with adrenal
insufficiency. (Liu D et al., 2013). Recovery from
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
264

steroid-induced adrenal insufficiency is time
dependent and the adverse effects are generally
reversible with lower dosage or discontinuation of
treatment. Abrupt cessation of the drugs may
precipitate adrenocortical insufficiency, therefore the
drugs must be gradually discontinued. (Stratakis
CA,2018;Lodish MB et al., 2018). The physiologic
dose of steroids should be given for about 6-9 months
because the recovery period of HPA axis suppression
is 3.49 ± 2.92 months.(
Tempark T et al., 2010). Our
patient was tapered down slowly over the past 3
months and was planned to have her morning cortisol
level check again in May 2019, 6 months after the
initial test.
Depends on the severity, treatments available for
childhood psoriasis are emollients, salicylic acid,
calcipotriol, coal tar, topical steroids, phototherapy,
retinoids, and cyclosporine (Rahmayunita G et al.,
2008). Topical steroids are not indicated in severe
psoriasis due to the possible side effects of excessive
usage. Whereas first line treatment for erythrodermic
or pustular psoriasis is acitretin, followed by
cyclosporine, phototherapy, methotrexate, anti-TNF
agents, and systemic steroids.(Bronckers et al., 2015;
Gudjonsson JE et al, 2012). Acute GPP has proven to
be, like many psoriasis variants, a difficult disease to
treat. (Hyde K et al., 2016). Severe and extensive
disease is likely to most effectively be treated with
infliximab (TNF-α inhibitor) or cyclosporine, given
the quicker onset of action with these drugs. (Hyde K
et al., 2016). Our patient was prescribed cyclosporine
with initial dose of 100 mg daily. Cyclosporine is an
calcineurin inhibitor which inhibits the T-cell
activation mediated by antigen. (Gudjonsson JE et al,
2012) It has a rapid onset of action of 2-4 weeks and
notable side effects are nephrotoxicity, hypertension,
nausea, and diarrhea.(Bronckers et al., 2015;
Gudjonsson JE et al, 2012) To date, the efficacy of
cyclosporine in pediatric psoriasis is limited. (Hyde K
et al., 2016).
Children may require higher dosage than
recommended in adults because of greater body
surface area to weight ratio. Therefore, the lowest
possible dose and shortest treatment period should be
used.(Bronckers et al., 2015;Al Aboud DM et al et
al., 2019;Hyde K et al., 2016).
Ideally high-potency topical steroids should be
obtained only with prescription in order to prevent
misuse of topical steroids.(Sahana PK et al., 2015)
Patients and especially parents should be informed
about the appropriate usage and the possible side
effects of the drug.Children are more susceptible to
side effects, thus parents should clearly understand
how to use topical steroid wisely. One of the side
effects of steroids is immunosuppression which may
increase the risk of opportunistic and bacterial
infections. Semiz et al reported a fatal case of
disseminated cytomegalovirus infection in a
Cushing’s syndrome patient due to topical steroid use
in the diaper area.(Semiz S et al., 2008). Therefore,
topical steroids should be used wisely especially in
children.
4 CONCLUSION
Adverse effects of steroid-induced adrenal
insufficiency is generally reversible and the recovery
is time dependent thus the cessation of exogenous
steroid should be gradual. During the gradual
discontinued of exogenous steroids, systemic agents
for psoriasis ie.acitretin orcyclosporine should be
initiated. Parents should be noted that misuse of
topical and oral corticosteroids could be harmful for
children and severe immunosuppression state could
end fatally.
REFERENCES
Al Aboud DM, Kumar S. Pustular psoriasis. 2019. In:
StatPearls [Internet]. Treasure Island (FL).
Bronckers IMGJ, Paller AS, Geel MJ, Kerkhof PCM,
Seyger MMB. 2015. Psoriasis in children and
adolescents: diagnosis, management and comorbidities.
Pediatr Drugs.;17(5):373-384.
Gudjonsson JE, Elder JT. Psoriasis. In: Goldsmith L, Katz
S, Gilchrest B, Paller A, Leffell D, Wolff K, eds 2012..
Fitzpatricks’s Dermatology in General Medicine.
Eight. McGraw-Hill;:197-231
Hyde K, Kivelevitch D, Mansouri B. 2016. Pustular
psoriasis: pathophysiology and current treatment
perspectives. Psoriasis Targets Ther.;6:131-144.
Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. 2006.
Adverse effects of topical glucocorticosteroids. J Am
Acad Dermatol.:1-15.
Liu D, Ahmet A, Ward L, et al. 2013. A practical guide to
the monitoring and management of the complications
of systemic corticosteroid therapy. Allergy Asthma Clin
Immunol.;9(1):30.
Lodish MB, Keil MF, Stratakis CA. 2018. Cushing’s
syndrome in pediatrics: an update. Endocrinol Metab
Clin N Am.;47:451-462.
Meena S, Gupta LK, Khare AK, et al. 2017.Topical
corticosteroids abuse: a clinical study of cutaneous
adverse effects. Indian J Dermatol.;62(6):675.
Rahmayunita G, Pulungan AB, Wiryadi BE, Wisesa TW,
Sugito TL. 2008. Cushing’s syndrome induced by
misuse of topical corticosteroids in a child with
psoriasis vulgaris. Med J Indones.;17(4):281-286.
Raff H, Sharma ST, Nieman LK. 2014.Physiological basis
for the etiology, diagnosis, and treatment of adrenal
Generalized Pustular Psoriasis in Childhood with Exogenous Cushing’s Syndrome
265

disorders: Cushing’s syndrome, adrenal insufficiency,
and congenital adrenal hyperplasia. Compr Physiol.
;4(2):739-769.
Stratakis CA.2008.. An update on Cushing syndrome in
pediatrics. Ann Endocrinol (Paris)
Sahana PK, Sarma N, Sengupta N, Somani PS. 2015. A
florid case of iatrogenic Cushing’s syndrome induced
by topical steroid with osteoporosis and hypogonadism.
Indian J Dermatol.;60(4):420.
Semiz S, Is Y, D M. 2008.Two cases of Cushing’s
syndrome due to overuse of topical steroid in the diaper
area. Pediatr Dermatol.;25(5):544-547.
Tempark T, Phatarakijnirund V, Chatproedprai S,
Watcharasindhu S, Supornsilchai V, Wananukul S.
2010. Exogenous Cushing’s syndrome due to topical
corticosteroid application: case report and review
literature. Endocr.;38:328-334.
Wang Q. 2017.Clinical features of von Zumbusch type of
generalized pustular psoriasis in children : a
retrospective study of 26 patients in southwestern
China.;92:319-322.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
266
