
A Case Report: Coexistent Pulmonary Tuberculosis and Lung
Cancer Diagnosed from the Same Specimen
Rispan Pratama
1*
, Bintang Yinke Magdalena Sinaga
1
1
Department of Pulmonology and Respiratory Medicine, Faculty of Medicine, Universitas Sumatera Utara
H.Adam Malik General Hospital, Medan, Indonesia.
Keywords: Pulmonary Tuberculosis, Lung Cancer
Abstract: Pulmonary tuberculosis and cancer are common causes of morbidity, mortality and major public health
problem worldwide, Tuberculosis can coexist with lung malignancy making the underlying disorder leading
to delay in diagnosis and management. Here we present an interesting case of a 58-year-old woman who on
initial presentation was diagnosed with tuberculosis but did not a response to antituberculosis therapy.
Further investigation revealed underlying lung cancer. The patient was then treated according to the latest
guideline.
1 INTRODUCTION
Cancer and tuberculosis are common causes of
morbidity and mortality, and a major public health
problem worldwide. The interaction between lung
cancer and active tuberculosis is known for many
years. The first description of ‘cancerous phthisis’
was reported by Bayle in 1815. Tuberculosis is an
important risk factor for cancer. The dormant bacilli
may activate due to disturbed defense mechanisms.
Pulmonary cancer mortality was higher in people
with tuberculosis than in those without. Diagnosis
may be a delay and the patient's survival may be
shorter (Beyhan, Aydin, 2018, p 33-37).
One-third of the world population is infected
with Mycobacterium Tuberculosis bacillus.
According to the WHO 2016 global tuberculosis
report, tuberculosis affects more than 9 million
people and caused death in 1.8 million people,
especially in developing countries (WHO, 2017).
Worldwide, there were approximately 14 million
new cancer cases, 8.2 million death-related cancer
and 32.6 million people living with cancer in 2012.
Among men, the three most common cancer are
lung, prostate, and colorectal cancer, and among
women, breast, colorectal and lung cancer as the
three most common causes (WHO, 2016).
Pulmonary tuberculosis and lung malignancy are
a common disease, especially in endemic areas
including Indonesia, This often requires special
attention to enforce the diagnosis. Clinicians often
find difficulties to identify due to similar symptoms,
which result in one disease or the other to be a delay
to be treated.
In this case report, there was a coexist pulmonary
tuberculosis and lung malignancy in one sample
diagnosed from Bronchoalveolar lavage (BAL) from
bronchoscopy procedure.
2 CASE
A 58-year-old female came to Adam Malik
General Hospital on 29 December 2018 with
complaints of shortness of breath since the previous
two months, which had gotten worse in the previous
one month. It became worse when she performed an
exercise. Cough occurred since the previous month
with whitish sputum production. Left chest pain
also occurred for a month before admission, and
worsened on a deep breath in and heavy coughing.
Hoarseness occurred for a month. Loss of body
weight for about 3 kgs was observed in the last 2
months. The patient was a farmer for 20 years.
History of biomass exposure was found with
pesticide and mosquito coils. The patient was
diagnosed with Diabetes Mellitus in the previous
year.
Before admitted to Adam Malik General
Hospital, patients were treated in another hospital in
Pratama, R. and Sinaga, B.
A Case Report: Coexistent Pulmonary Tuberculosis and Lung Cancer Diagnosed from the Same Specimen.
DOI: 10.5220/0009864402530256
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 253-256
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
253
November 2018, and had pleural fluid an amount of
3000 ml aspirated from the left pleura. The patient
was started on category I Anti Tuberculosis Therapy
(ATT) in November 2018. The patient also received
medication from a pulmonologist, based on chest X-
ray and clinical presentation.
On examination on 14 January 2019, the patient
was alert, blood pressure was 110/80 mmHg, pulse
rate was 104 times/minute, respiratory rate was 24
times/minute, the temperature was 36,5Ԩ, and SpO2
was 97% at room air,
On chest examination, there was an
asymmetrical chest movement, delayed movement
on the left hemithorax, decreased of the tactile
fremitus on the left hemithorax, dullness on the left
hemithorax and diminished breath sound on the left
hemithorax without additional sound. Enlargement
of the liver was found, tenderness of the liver was
found.
Laboratory findings on 29 February 2019
showed haemoglobin 14.0 g/dl, leukocyte 21.910 x
10
3
/mm
3
, erythrocyte 4.98 x 10
6
/mm
3
, hematocrite
39.1%, platelet 323.000 /mm
3
, ad random blood
glucose 400 mg/dL, natrium 131 meq/ml, kalium 2.8
meq/ml, chloride 93 meq/ml, and nonreactive Elisa
Test for HIV.
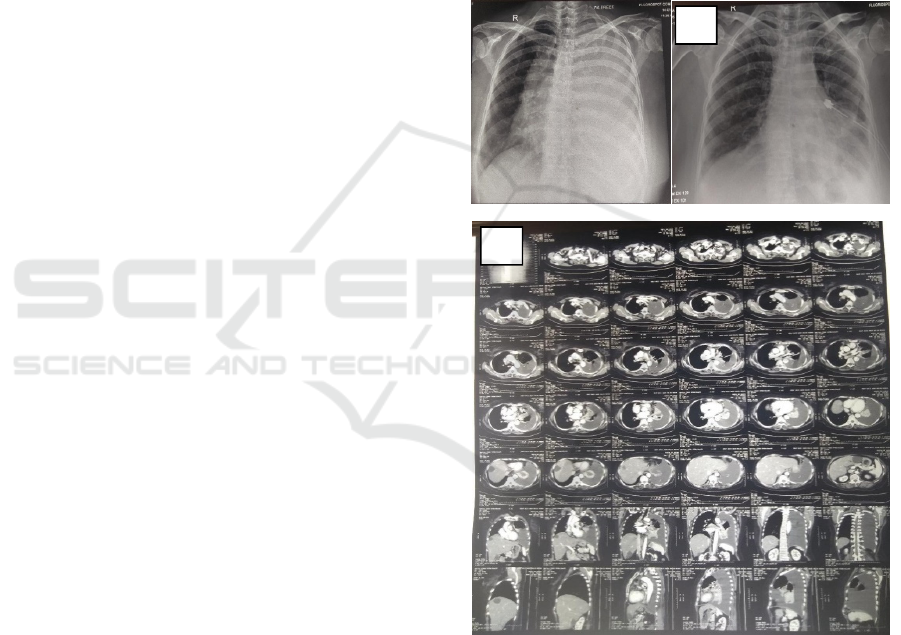
Radiological finding from 14 January 2019
showed homogenous consolidation appearance.
Thorax CT-Scan on 8 January 2019 showed left lung
tumor, enlarged perihilar lymph node, left pleural
effusion T2aN3M1b (liver) (Figure 1).
Bronchoscopy finding showed infiltrative
stenosis in lingula and left lower lobe. Biopsy results
were in line with the image of adenocarcinoma,
cytology with a malignant smear (C5). Results from
cytology of BAL revealed an impression of
adenocarcinoma, with a malignant smear (C5).
Similar findings were also shown in pleural fluid
cytology with C3 atypic smears but tend to be clear
on the impression of reactive mesothel.
GeneXpert analysis of bronchoalveolar lavage
showed Mycobacterium tuberculosis susceptible to
rifampicin. Epidermal Growth Factor Receptor
(EGFR) analysis on 17 January 2019 showed no
mutation detected.
2.1 Working Diagnose
We diagnosed this patient with left lung
adenocarcinoma T4N3M1c (pleura, hear) stage IVb
PS I with a new case of pulmonary tuberculosis, and
diabetes mellitus.
2.2 Treatment
Tuberculosis treatment consisted of two months of
RHZE (R: rifampicin, H: isoniazide E: ethambutol,
Z: pyrazinamide) plus 7 months of RH daily until
complete TB treatment. The evaluation was
performed two months after the initiation of
treatment including clinical and physical
examinations, chest x-ray, and AFB smear.
The patient also received chemotherapy with
platinum-based therapy such as carboplatin and
paclitaxel. Chemotherapy was planned for 6 cycles
and would be evaluated every 2 cycles.
Fig 1: Radiological findings. (A) shows homogenous
consolidation, large pleural effusion, (B) after insertion of
water sealed drainage (WSD) in Adam Malik Hospital.
(C) Thorax CT-Scan
A
B
C
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
254
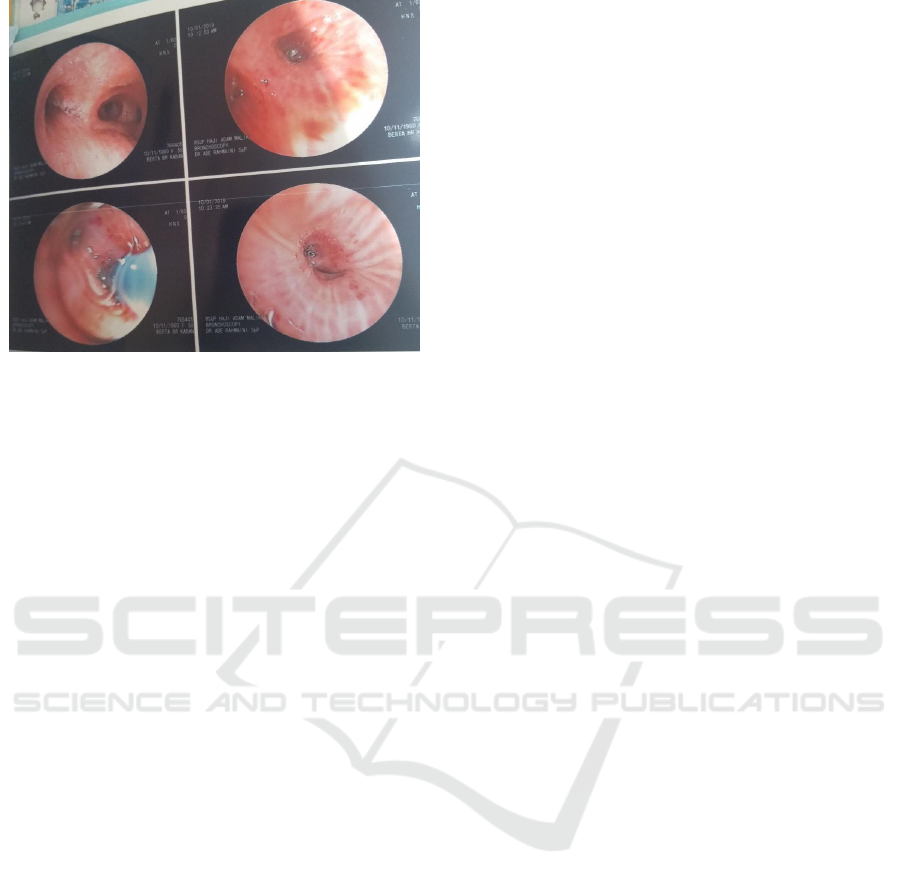
Figure 2: Bronchoscopy Finding
3 DISCUSSION
The relationship between pulmonary tuberculosis
and lung cancer has been known for years.
Pulmonary tuberculosis and lung cancer are able to
mimic each other, often on clinical symptoms and
radiological features. The common symptoms are
fever, night sweats, loss of appetite, weight loss,
fatigue, and chest pain. Cancer cells invasion in
healed tuberculosis lesions might also lead to
tuberculosis reactivation by weakening the local
immunity. Two diseases may be located in the
ipsilateral lung, contralateral lung or same lobe
location. Tuberculosis bacilli may live at a dormant
status in granulomas and induce tuberculosis
sensitivity (WHO, 2016). When the local immunity
deteriorates, reactivation of latent TB, primary
mycobacterial infection, the new exogenous
infection may cause tuberculosis infection. Chronic
inflammation like pulmonary tuberculosis process
may also lead to carcinogenesis of the lung tissue
which can lead to DNA damage by nitric oxide
synthase from the infected macrophage. Thus,
chronic inflammation and scarring due to
tuberculosis can lead to the development of cancer.
An occurrence of lung cancer at the site of the scars
of old tuberculosis lesions has been shown in other
studies (Jacobs, Gu, Chachoua, 2015). According to
Harikrishna et al., the possible association between
cancer and tuberculosis is a coincidence without any
apparent relation, can be a simultaneous
development of both tuberculosis and cancer, a
metastatic carcinoma developed in an old
tuberculosis scar, or a secondary TB infection in
cancer (Harikrishna, Sukaveni, Kumar, 2012). The
discordant organ involvement may be by chance
without any apparent relation. Smoking is an
important risk factor for lung cancer. Chemotherapy,
immune dysfunction, radiotherapy, severe
malnutrition may lead to immune suppression.
Radiotherapy might lead to deregulation of
granulomas microenvironment, allowing
tuberculosis mycobacteria to proliferate
(Wu, et al,
2011). Kurasawa et al. showed that coexistence of
lung cancer and pulmonary tuberculosis occurred in
about 2 to 4% of lung cancer cases and in about 1 to
2% of tuberculosis cases. Histopathology analysis of
lung cancer revealed a more periphery origin and a
squamous cell carcinoma. As previously reported
(Kurasawa, et al, 1998), the authors concluded that
in this case report, lung cancer is comorbid that is
most likely to be a risk factor for the decrease in
endurance, hence patient became susceptible to
tuberculosis.
4 CONCLUSION
In this case report, a patient was diagnosed with
pulmonary malignancy and tuberculosis infection.
The patient was planned to be continuously observed
to evaluate the response of therapy. Although with
the worst prognosis, it was expected that appropriate
therapy would improve the quality of life. As a
clinician, we should be able to make this case report
as a reference to be more active in looking the
possible risks of tuberculosis and lung cancer to
occur together so that treatment of either disease will
not be delayed.
REFERENCES
Beyhan C, Aydin C, Evaluation of coexistence of cancer
and active tuberculosis;16 case series, respiratory
medicine case report 23 (2018) 33-37.
Harikrishna, J., Sukaveni, V., Kumar, D.P., Cancer and
tuberculosis, J. Indian Acad.Clin. 13 (2) (2012) 142–
144.
Jacobs R.E., Gu P., Chachoua, A., Reactivation of
pulmonary tuberculosis during cancer treatment, Int.
J. Mycobacteriol. 4 (4) (2015) 337–340.
Karnak, D., Kayacan, O., Beder, S., Reactivation of
pulmonary tuberculosis in malignancy, Tumori 88
(2002) 251–254.
Kurasawa, T., The coexistence of pulmonary tuberculosis
and lung cancer, Nihon Rinsho 56 (12) (1998) 3167–
3170.
A Case Report: Coexistent Pulmonary Tuberculosis and Lung Cancer Diagnosed from the Same Specimen
255

World Health Organization. Global tuberculosis report.
2016. Available at http://who.int/tb/publications/global
report/en/.
WHO, WHO list of priority medical devices for cancer
management, (2017), pp. 9–10 ISBN: 978-92-4-
156546-2.
Wu, C.Y., Hu, H.Y., Pu, C.Y., Huang, N., Shen, H.C., Li,
C.P, Chou, Y.J., Pulmonary tuberculosis increases the
risk of lung cancer: a population-based cohort study,
Cancer 117 (2011) 618–624.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
256
