
Risk Factors Associated with Ventilator-associated Pneumonia
Incidence in the Intensive Care Unit at Haji Adam Malik
General Hospital, Medan, Indonesia
Miranda
1*
, Achsanuddin Hanafie
2
, Rina Yunita
3
1
Tropical Medicine Program Faculty Medicine, Universitas Sumatera Utara, Jl Dr. Mansur No 5 Medan 20155,
2
Departement of Anesthesiology and Intensive Therapy, Haji Adam Malik General Hospital, Medan, Indonesia.
3
Departement of Mycrobiology, Faculty of Medicine, Universitas Sumatera Utara, Medan Indonesia.
Keywords: Ventilator-Associated Pneumonia, pneumonia, nosocomial, risk factors, Indonesia
Abstract: Ventilator-associated pneumonia (VAP) is defined as nosocomial pneumonia that occurs 48 hours after
using mechanical ventilation. The primary objective of this study is to investigate the risk factors associated
with the incidence of VAP. The secondary objective is to identify the pattern of bacterial sensitivity in
confirmed VAP cases. A retrospective study was conducted in the intensive care unit at Haji Adam Malik
General Hospital, Medan. Data of 60 patients with and without VAP diagnosis between March 2017 and
October 2018 were evaluated. The most common cause of infection was Klebsiella pneumonia (36.7%),
with 90.9% were sensitive to Amikacin. Majority of patients were (76.6%, 46/60) aged < 60 years, used
ventilator longer than 5 days (68.3%, 41/60) and with the smoking habit (53.5%, 32/60). We found no
association between age, duration of ventilator and smoking habit with the increased incidence of VAP.
Further study with a larger sample size may be needed to find the associations.
1 INTRODUCTION
Ventilator Associated pneumonia (VAP) is defined
as pneumonia occurring 48 hours after the initiation
of endotracheal intubation and mechanical
ventilation (MV)
(PDPI, 2003; Goel E et al., 2012;
Widyaningsih R and Buntaran L, 2012; Hezati M E
et al., 2015). The use of endotracheal tube increased
the risk of infectious agents to gain direct access to
the lower respiratory tract leading to pneumonia
(Kalanuria A et al., 2014).
VAP is classified into
early onset (<5 days) and late onset (≥5 days). Early
onset is usually caused by sensitive pathogens, while
late onset is due to multidrug resistance microbial
(Sedwick M B et al., 2012)
.
Clinical assessment,
physical examination and radiographic images
incorporated in the clinical pulmonary infection
scoring (CPIS) is the most common tool used to
predict the occurrence of VAP.
A systematic review of 51 prospective
randomized trial described the incidence of VAP
was 22,8% (Yunita R and Rondhianto W,2015), and
86% of all cases were due to nosocomial infections
(Wahyuning Tyas et al., 2013). VAP was associated
with increased morbidity and mortality, prolonged
hospital stay and patient cost (Koenig S M and
truwit J D, 2006). The incidences of VAP in other
countries varied from 9% to 27% (Chawla, 2008)
while there are no definite incidence rates reported
from Indonesia. High mortality ranging from 24% to
50% has been associated with the presence of
antimicrobial resistance particularly in cases of
Pseudomonas aeruginosa, Acinetobacter baumanii,
Klebsiella, and Enterobacter spp. The wide use of
antimicrobials, the presence of comorbidity and
prolonged used of mechanical ventilator facilitated
the development of antimicrobial resistance
(Resende M et al.,2013). Studies have reported
factors including prior intravenous antibiotic use
within the previous 90 days, septic shock at time of
VAP diagnosis, acute respiratory distress syndrome
(ARDS) preceding VAP, hospitalization > 5 days
prior to the occurrence of VAP, and acute renal
replacement therapy prior to VAP onset to be the
main factors associated with VAP.
There are several risk factors affecting the
development of VAP. Some of these risk factors
may have already been presented at admission to the
Intensive Care Unit (ICU), such as advanced age,
Miranda, ., Hanafie, A. and Yunita, R.
Risk Factors Associated with Ventilator-associated Pneumonia Incidence in the Intensive Care Unit at Haji Adam Malik General Hospital, Medan, Indonesia.
DOI: 10.5220/0009863902370242
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 237-242
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
237
presence of respiratory or cardiovascular system
disease, organ failure, burns, trauma, acute
respiratory distress syndrome (ARDS), gastric
colonization, sinusitis, high volume gastric
aspiration, and seasonal change (Ziyaettin K R I et
al., 2018) . Age is one of the main factors
influencing the VAP events. Susanti et al. described
that the older the age of the patients treating by a
ventilator, the greater the risk to develop VAP. This
is because the age older than 60 years old has a
greater risk of suffering pneumonia in the use of a
mechanical ventilator in the ICU and there is a
decrease in the body’s immune function (Susanti E
et al., 2013)
Another factor influencing VAP events is the
duration of mechanical ventilator used. Mechanical
ventilation is a machine to perform some or all of
the work of breathing and an essential aspect of
critical patient care (Clare M V and Dacvecc H K,
2005). Therefore, identification of risk factors
associated with VAP is needed to implement
preventive measures and to reduce mortality as the
outcome of VAP. In this study, we aimed to evaluate
the association between risk factors and the
incidence of VAP among intensive care unit patients
in Haji Adam Malik General Hospital in Medan,
Indonesia.
2 METHODS
Data from 60 ICU patients admitted at Haji Adam
Malik Hospital between March 2017 and October
2018 was collected (see table 1). CPIS form was
used to assess risk factors and information on VAP.
VAP diagnosis was made by the ICU doctors based
on the following criteria: at least two of the
following points, fever of ≥ 38°C, leukocytosis of
10.000/mm
3
or more, and purulent respiratory
secretions; with chest radiograph showing new,
persistent pulmonary
infiltrates. The diagnosis was
confirmed by sputum culture at the microbiology
laboratory (see table 2).
Inclusion criteria were patients aged more than
18 years old and intubated and mechanically
ventilated for more than 48 hours. Exclusion criteria
included patients with underlying diseases
(tuberculosis, malignancy, chronic obstructive
pulmonary diseases, and pneumonia).
The study was reviewed and approved by the
ethics committee at the Faculty of Medicine,
Universitas Sumatera Utara.
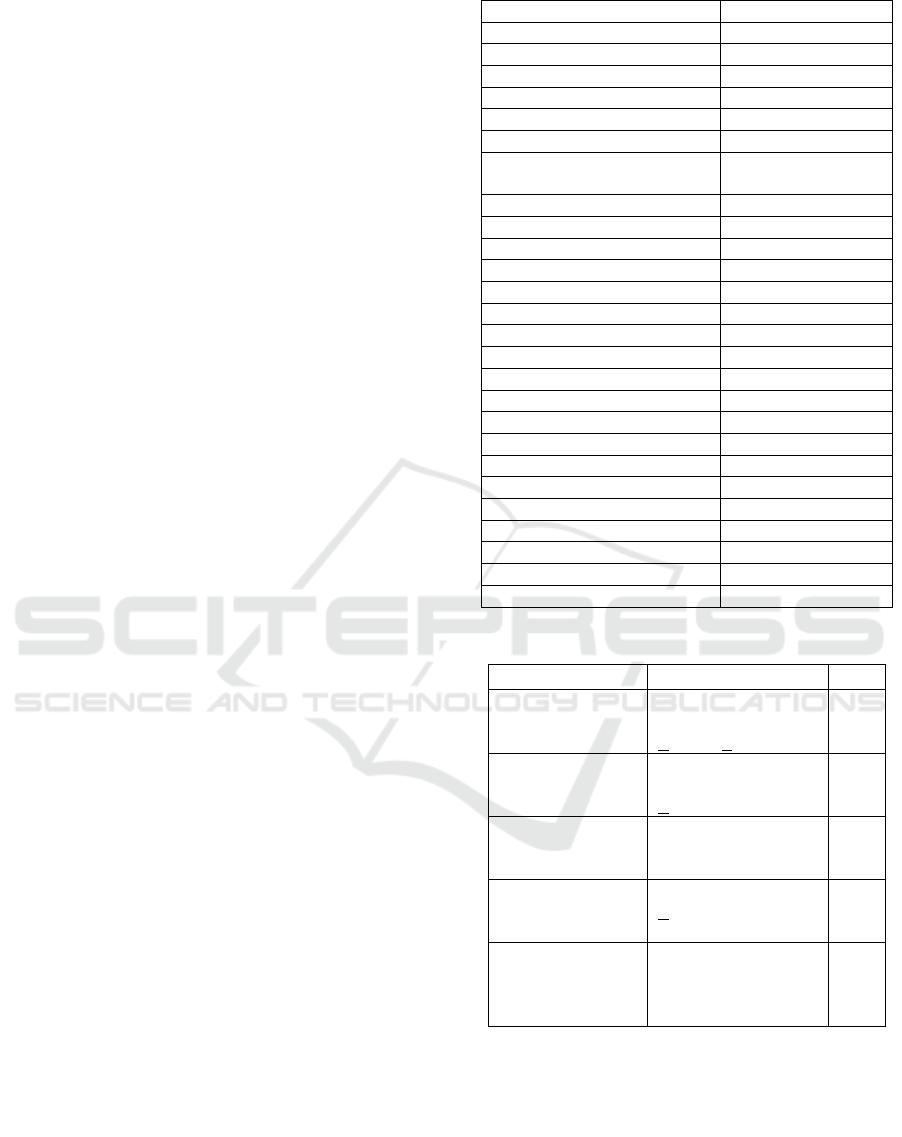
Table 1: Demographic characteristics of research subjects
in ICU
Characteristics n = 60 (%)
Gender, n (%)
Male 35 (58.3)
Female 25 (41.7)
Age (years)
<60 46 (76.7)
≥60 14 (23.3)
Duration of ventilator used
(days)
> 5 41 (68.3)
≤ 5 19 (31.7)
Education level,
Primary school 12 (20.0)
Junior high school 7 (11.7)
High school 38 (63.3)
University 3 (5.0)
Occupation
Private sectors 28 (46.7)
Midwife 16 (26.7)
Farmer 6 (10.0)
Trader 3 (5.0)
Fisherman 2 (3.3)
Government officers 2 (3.3)
Student 2 (3.3)
Retired 1 (1.7)
Smoking habits
Yes 32 (53.3)
No 28 (46.7)
Table 2 : Clinical Pulmonary Infection Score (CPIS)
Component
Score
Temperature (
0
C) 36,5 - 38,4
38,5 - 38,9
<36 and >39
0
1
2
Blood Leukocytes
(/mm
3
)
4000-11000
< 4000 atau > 11000
> 500 cells band
0
1
2
Tracheal
secretions
None
Few or non purulent
Purulent
0
1
2
Oxygenation PaO
2
/FiO
2
mmHg
>120 or ARDS
< 240 and absence
of ARDS
0
2
Chest radiograph No, infiltrate
Patchy or diffuse
infiltrate
Localized infiltrate
0
1
2
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
238
3 RESULTS
Sixty patients were enrolled in the study. Of those,
30 was patients diagnosed with VAP and 30 was not
identified as VAP cases. Baseline characteristics are
shown in Table 1. Thirty-five patients (58.3%) was
male, and 46 (76.7%) aged younger than 60 years
old. The duration of mechanical ventilation use
longer than 5 days occurred in 41 patients (68.3%).
None of the risk factors assessed in this study
increased the risk of VAP incidence in the ICU
(Table 3); being male (OR 1.115, 95% CI 0.364-
3.628, P=0.793), aged > 60 years old (OR 0.688,
95% CI 0.168-2.695, P=0.542), ventilator used
longer than 5 days (OR 1.592, 95% CI 0.465-5.573,
P=0.405), and had smoking habit (OR 1).
Furt
hermore, 30 patients confirmed with VAP
had bacterial growth in culture (See table 4) with
Klebsiella pneumonia (N=11) as the most common
organism, followed by Acinetobacter baumannii
(N=8) and Pseudomonas aeruginosa (N= 4).
Sensitivity test showed amikacin to be sensitive to
K. pneumonia infection (90.9%).
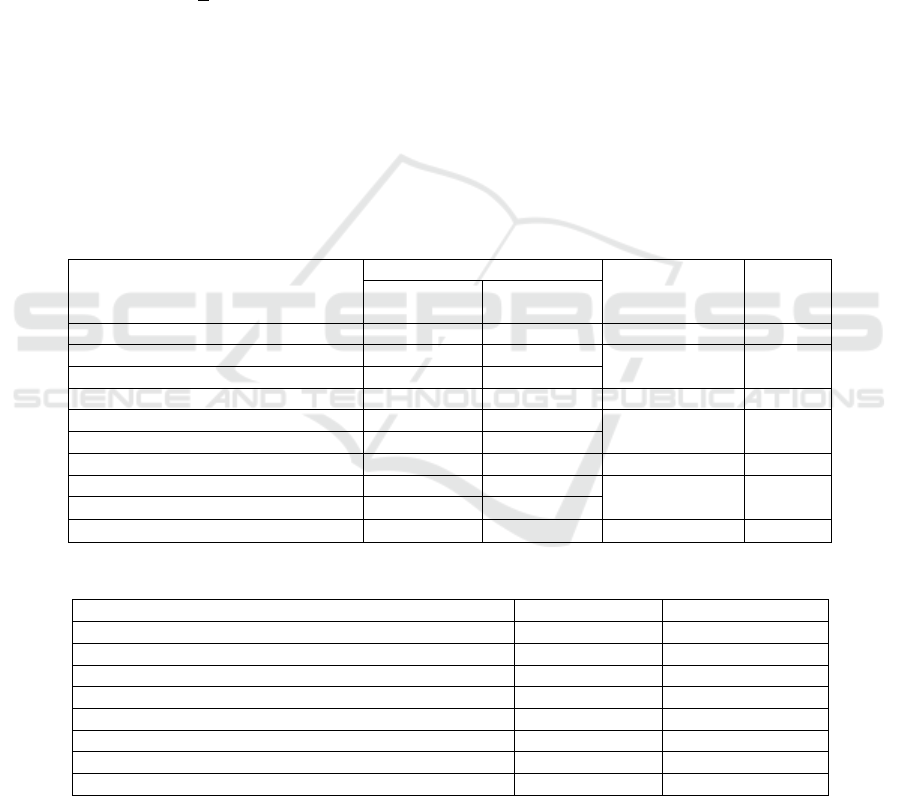
The evaluation of sensitivity and antibiotic
resistance on the pathogens are described in Table 5.
Nine antibiotics were still sensitive against P.
aeruginosa
including ceftazidime, amikacin,
ceftriaxone, meropenem, ertapenem, cefazoline,
cefixime, ciprofloxacin, and a
ztreonam. While there
were 14 antibiotics that were highly resistant to P.
aeruginosa.
Sensitivity analysis on K
. pneumoniae showed
12 antibiotics were still sensitive including
amikacin, ertapenem, meropenem, gentamycin,
ciprofloxacin, cefoperazone/sulbactam, ceftazidime,
amoxicillin/ clavulanic acid, levofloxacin,
tetracycline, tigecycline, and polymixin B. Fourteen
antibiotics showed resistance to K. pneumoniae (see
table 5).
The analysis also showed that amikacin,
ertapenem, meropenem, polymixin B, ceftazidime,
ciprofloxacin and piperacillin/tazobactam to be
sensitive to A. baumannii (see table 5)
Table 3: Relationship between risk factors with VAP in the ICU at Haji Adam Malik General Hospital, Medan, Indonesia
Variables
VAP
OR
(95% CI)
P
Cases
(n=30)
Controls
(n=30)
Age, (Year)
≥ 60 6 (20.0) 8 (16.7) 0.688
(0.168-2.695)
0,542
< 60 24 (80.0) 22 (73.3)
Duration of ventilator used, (days)
> 5 22 (73.3) 7 (63.3) 1.592
(0.465-5.573)
0,405
≤ 5 8 (26.7) 3 (36.7)
Smoking habits
Yes 16 (53.3) 16 (53.3) 1
(0.322-3.109)
1,000
No 14 (46.7) 14 (46.7)
Table 4: Bacterial profile of patients diagnosed with VAP
Bacterial isolated N %
Klebsiella pneumonia 11 36,7
Acinetobacter baumanii 8 26,7
Pseudomonas aeruginosa 4 13,3
Staphylococcus aureus 3 10.0
Enterobacter cloacae 2 6,7
Elizabethkinqia meni 1 3,3
Raoultella ornithine 1 3,3
Total 30 100,0
Risk Factors Associated with Ventilator-associated Pneumonia Incidence in the Intensive Care Unit at Haji Adam Malik General Hospital,
Medan, Indonesia
239
Table 5: Antibiotic sensitivity and resistance to bacteria caused VAP in ICU Haji Adam Malik General hospital
Antibiotic
KP
AB
PA
S I R S I R S I R
Amikasin 90,9 9,1 0 75 0 25 50 0 50
Ampicillin 0 54,5 45,5 0 87,5 12,5 0 100 0
Ampicillin/Sulbaktam 0 54,5 0 0 87,5 12,5 0 100 0
Cefazolin 0 36,4 63,6 0 50 50 25 25 50
Cefixim 0 45,5 54,5 0 75 25 25 75 0
Ceftazidime 9,1 36,4 0 12,5 12,5 75 100 0 0
Ceftriaxone 0 27,3 72,7 0 25 75 50 50 0
Ertapenem 81,8 0 18,2 25 12,5 62,5 50 0 50
Meropenem 81,8 0 18,2 25 12,5 62,5 50 0 50
Ciprofloxacin 27,3 0 18,2 12,5 62,5 25 25 75 0
Erithromycin 0 100 0 0 100 0 0 100 0
Gentamycin 36,4 45,5 18,2 0 100 0 0 75 25
Lefofloxacin 9,1 81,8 9,1 0 87,5 12,5 0 100 0
Netilmicin 0 90,9 9,1 0 100 0 0 100 0
Tetracycline 9,1 81,8 9,1 0 100 0 0 50 50
Vancomycin 0 100 0 0 100 0 0 100 0
Trimthoprime/Sulfamethoxazole 0 90,9 9,1 0 87,5 12,5 0 50 50
Aztreonam 0 90,9 9,1 0 100 0 25 75 0
Fosfomycin 0 100 0 0 100 0 0 100 0
Amoxicillin/Clavulanic Acid 9,1 90,9 0 0 100 0 0 100 0
Polymixin B 9,1 90,9 0 25 75 0 0 100 0
Linezolid 0 100 0 0 100 0 0 100 0
Tigecycline 9,1 90,9 0 0 100 0 0 100 0
Cefotaxime 0 63,6 36,4 0 37,5 62,5 0 100 0
Cefuroxime 0 90,9 9,1 0 87,5 12,5 0 100 0
Cotrimoxazole 0 100 0 0 100 0 0 100 0
Cefoperazone/Sulbactam 18,2 81,8 0 0 100 0 0 100 0
Nitrofurantoin 0 81,8 18,2 0 100 0 0 75 25
Piperacillin/Tazobactam 0 90,9 9,1 12,5 87,5 0 0 75 25
Clindamycin 0 100 0 0 100 0 0 100 0
KP Klebsiella pneumoniae, AB Acinetobacter baumanii, PA Pseudomonas aeruginosa, S sensitive, I intermediate,
R resistance
4 DISCUSSIONS
VAP has been associated with mortality, and this
study evaluated the risk factors associated with the
incidence of VAP in order to implement preventive
measures in order to reduce mortality in ICU
patients.
In this study, we found age not to be a risk factor
for VAP in contrast to other studies. This can be
explained by the age distribution among our
patients. The majority of patients hospitalized in the
ICU were aged less than 60 years old with the most
common diagnosis of post-craniotomy with a history
of traffic accidents. Similar results were shown in
studies from Kurdistan Iran which described the
majority of patients exposed to VAP was younger
than 60 years old, as also in a study reported in
Indonesia (Riatsa A et al., 2013).
VAP has also been reported to likely occur in the
first week of mechanical ventilation due to the
interaction of more risk factors at the beginning of
admission (Putri Y and Budiono, 2014). However, in
this study, the length of ventilator use was not
significantly associated with the development of
VAP. Neither the longer use of a ventilator (>5
days), as determined to be the cutoff for longer use
of a ventilator, nor shorter us increased the risk of
VAP. This is also supported by the results of a study
from the ICU of Dr. Kariadi General Hospital
Semarang Indonesia (Santoso B, 2015).
In addition, we also did not find a significant
association between smoking habit and the incidence
of VAP, similar to the findings in other studies
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
240

(Santoso B, 2015; Maria YS, 2011; Othman HA et
al, 2017).
This retrospective study had several limitations.
First, this study was conducted in a single medical
center and there may have been patient selection
bias. Second, this study was a retrospective survey,
which not only resulted in incomplete data for some
patients. Third, the disproportion of the samples in
the collecting stage. This disproportion may result in
different findings from others, including age,
duration of ventilator used and smoking habits.
VAP remains an important nosocomial infection
especially among the critically ill patients admitted
to the ICU in our setting. Further study involving
more detailed risk factors, diagnosis at admission,
and presence of high-risk microorganisms need to be
conducted to determine the risk factor for this event.
5 CONCLUSIONS
1 The risk factor that has no significant related
with VAP infection in ICU patient at Haji
Adam Malik General hospital Medan are age
(OR= 0.688, 95% CI 0.168-2.695, P=0.542)
2 There was no significant association between
duration of ventilator used with VAP incidence
but the duration of ventilator used more than 5
days are more 1.592 at risk for VAP than ≤ 5
days OR 0.592, 95% CI 0.465-5.573, P=0.405)
3 There was no significant association between
smoking habits with VAP incidence. The risk
value cannot be assessed because the group of
cases exposed and the control group exposed to
the same number. (OR=1, 95% CI 0.322-3.109,
P=1,000)
4 There are seven bacteria cause VAP found in
this study: Klebsiella pneumonia, Acinetobacter
baumanii, Pseudomonas aeruginosa,
Staphylococcus aureus, Enterobacter cloacae,
Elizabethkinqia meni, and Staphylococcus
aureus.
5 The results of sensitivity test for K.pneumoniae,
Amikacin, Ertapenem, Meropenem,
Gentamycin,
Ciprofloxacin,Cefoperazone/Sulbactam,
Ceftazidime Amoxycillin/Clavulanic acid,
Levofloxacin, Tetracycline, Tigecycline and
Polymixin B. The results of sensitivity test for
A.baumanii Amikacin, Ertapenem,
Meropenem, Polymixin B, Ceftazidime,
Ciprofloxacin, and Piperacillin/Tazobactam.
The results of a sensitivity test for P.aeruginosa
Ceftazidime, Amikacin, Ceftriaxone,
Meropenem, Ertapenem, Cefazoline, Cefixime,
Ciprofloxacin, and Aztreonam.
REFERENCES
Chawla, R. M., 2008. Epidemiology, Etiology and
Diagnosis of Hospital-Acquired Pneumonia and
Ventilator-Associated Pneumonia in Asian Countries.
36(4), pp. S93-S100.
Clare, M. V., & DACVECC, H. K. Mechanical
ventilation: Indication, goals, and prognosis.
2005.p.195-208.
Goel, V., A Hogade, S. & Karadesai, S., 2012. Ventilator
Associated Pneumonia in a Medical Intensive Care
Unit: Microbial Aetiology, Sesceptibility Pattern of
Isolated Microorganism and Outcome,. Indian journal
of Anaesthesia. 2012:56(6) : 558-562.
Hezati, M. E., Nazamiyeh, M., Seifar, F. & Beheshti, F.,
2015. Polymicrobial Ventilatoe Associated Pneumonia
and Antibiotic Susceptibility of Bacterial Isolates in a
University Hospital, Tabriz, Iran. African Journal of
Bacteriology Research.2015 : 7(5), p. 52-55.
Kalanuria, A. A., Zai, W. & Mirski, M. Ventilator
Associated Pneumonia in the ICU.2014: 18(2), p. 1-8.
Koenig, S. M. & Truwit, J. D. Ventilator-A ssociated
Pneumonia: Diagnosis, Treatment, and Prevention.
Clinical microbiology reviews.2006: 19(4), p. 637-
657.
Lahoorpour, F., Delpisheh, A., & Afkamzadeh, A. Risk
factors for acquisition of ventilator associated
pneumonia in adult intensive care unit.2013:29 (5),
1105-1107.
Maria Yosephine Sutiastuti. faktor-faktor yang
Berhubungan dengan Kejadian Pneumonia pada
Pasien pada unit Unit Intensif di Rumah Sakit Pondok
Indah Jakarta Selatan, Skripsi, Universitas
Pembangunan Nasional, Jakarta.2011.
Othman, H. A., Gamil, N. M., Elgazzar, A. E., & Fouad,
T. A. (2017). Ventilator associted pneumonia,
Incidence and risk factors in emergency intensive care
unit Zagazig university hospital . Egyptian journal of
chest diseses and tuberculosis.2017: 66. 703-708.
PDPI . Pneumonia Nosokomial. Dalam: Pedoman
Diagnosis & Penatalaksanaan Pneumonia
Nosokomial di Indonesia. Jakarta.2003 : p 1-17.
Putri, Yolanda, D., & Budiono. (2014). Hubungan antara
Lama penggunaan ventilator mekanik dengan
Kejadian Ventilator Associated Pneumonia (VAP)
Pada pasien Nonsepsis di ICU RSUP Dr Kariadi
Semarang . E-Journal Undip.2014: 1-16.
Resende,Marilia M. et al. Epidemiology and outcomes of
ventilator associated pneumonia in northern Brazol:
an analytical descriptive prospective cohort study
.Biomed Central.2013:13(119) p.1-6
Riatsa, A., Nana, R. & Nur, K. Faktor-faktor yang
berhubungan dengan kejadian ventilator associated
pneumonia (VAP) pada pasien yang menggunakan
Risk Factors Associated with Ventilator-associated Pneumonia Incidence in the Intensive Care Unit at Haji Adam Malik General Hospital,
Medan, Indonesia
241

ventilator mekanik di ICU RSUD Tugurejo Semarang.
Ners widya husada Semarang.20152(1), p. 1-14.
Santoso Budi. Faktor-faktor yang Berhubungan dengan
Kejadian Pneumonia pada Pasien di Intensive Care
Unit (ICU) Rumah Sakit Islam
Surakarta.2015.file.///C/User/perpustakaan
/Downloads/42-83-2-PB%20(1).pdf
Sedwick,M.B.,et al. Using evidence based practise to
preven Ventilator Associated Pneumonia.
2012:32(4).p.41-52
Susanti, E., Utomo, W. & Irvani D, Y. Identifikasi Faktor
Resiko Kejadian Infeksi Nosokomial Pneumonia pada
Pasien yang Terpasang Ventilator di Ruang Intensive
Care.2015:2(1).p. 590-598
Wahyuning Tyas, M., Suprapti, B. & Hardiono. Analysis
of Antibiotic use in VAP (Ventilator Associated
Pneumonia) Patients. Folia Medica
Indonesiana.2013:49(3), p. 168-172.
Widyaningsih, R. & Buntaran, L. Pola Kuman Penyebab
Ventilator Associated Pneumonia (VAP) dan
Sensitivitas terhadap Antibiotik di RSAB Harapan
Kita. Sari Pediatri.2012:13(6), pp. 384-390.
Yunita, R. & Rondhianto, W., 2015. Pengaruh Open
Suction System terhadap Kolonisasi Staphylococcus
Aureus pada Pasien dengan Ventilator Mekanik di
Ruang Intensive Care Unit (ICU) RSD dr. Soebandi
Jember. 3(1), pp. 103-110.
Ziyaettin, K., R, I., H, A., Girgin, N. K., F, K., & M, S.
Prognostic risk factors in Ventilator Associated
Pneumonia. ISI Journal Master List .2018: 24, 1321-
1328.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
242
