
The Role of Anemia to Restless Legs Syndrome in Regular
Hemodialysis Patients in Haji Adam Malik
Medan General Hospital
Rasyidah Hasan Harahap
1
, Riri Andri Muzasti
2*
1
Department of Internal Medicine, Faculty of Medicine, Universitas Sumatera Utara/Haji Adam Malik General Hospital,
Medan, Indonesia
2
Division Nephrology and Hypertension, Department of Internal Medicine, Faculty of Medicine, Universitas Sumatera
Utara/Haji Adam Malik General Hospital, Medan, Indonesia
Corresponding author: Riri Andri Muzasti,
Division Nephrology and Hypertension, Department of Internal Medicine,
Faculty of Medicine, Universitas Sumatera Utara/Haji Adam Malik General Hospital, Medan, Indonesia
Jl. Bunga Lau No.17, Medan, Indonesia, Phone/facsimile:+62-61-8365742.
Keywords: anemia, restless legs syndrome, hemodialysis
Abstract: Background: Restless Syndrome (RLS) has a higher prevalence in hemodialysis (HD) patients compared
to the general population. Anemia as a cause of the high prevalence of RLS in HD is still unclear. Method:
This is a cross-sectional study conducted in October 2017 evaluated 106 regular HD patients in Haji Adam
Malik Medan General Hospital who had fulfilled inclusion and exclusion criteria. RLS diagnoses and
severity was done in face to face interview according to the International Restless Legs Syndrome Study
Group. Biochemical characteristics were measured. Bivariate and multivariate analysis was performed.
Results: Of the 106 patients who took part in this study, RLS was found in 32 patients (30.2%). Hb levels in
regular hemodialysis patients with RLS have a lower mean than patients without RLS. In the multivariate
analysis using multinomial regression it was found that age and TIBC levels were associated with RLS and
Hb as a protection factor for RLS OR 0.697 95% CI 0.496 ± 0.98. Conclusion: Anemia is one of the factors
that influence the occurrence of RLS in addition to age being a matter that must be considered in the
prevention and management of RLS in hemodialysis patients.
1 INTRODUCTION
Restless Legs Syndrome (RLS) is one of the most
common sleep disorders in dialysis patients with a
prevalence reaching 20% in patients with Chronic
Kidney Disease (CKD) (Scherer JS, et al., 2017).
Some literature shows an association between RLS
and quality of life and mortality of patients with HD
(what HD stand for?) (Neves, et al., 2017). Patients
with HD who have RLS, have a higher mortality rate
compared to patients without RLS (32.3% vs.
14.5%; p <0.04) with Hazard Ratio 1.39; 95% CI
1.08-1.79) (Scherer JS, et al., 2017).
Decreasing HD prevalence of RLS in patients
who have received kidney transplantation (4% vs.
11%; p <0.001) illustrates that kidney disease itself
plays a role in the occurrence of RLS (Scherer JS, et
al., 2017).
It was already known that one of the
complications of CKD is anemia (Suwitra, 2014). In
dialysis patients, anemia is considered to be the main
cause of RLS regardless of available iron reserves
(Menezes, et al., 2018). However, several studies are
not in line with this finding (Kim, et al., 2008).
The pathophysiology of anemia with the
occurrence of RLS in regular hemodialysis patients
is still unclear. Therefore, we were interested in
knowing the relationship of anemia with RLS in
regular HD patients. This is important to be used as
prevention and management of RLS in regular
hemodialysis patients. The aim of the study…..
Harahap, R. and Muzasti, R.
The Role of Anemia to Restless Legs Syndrome in Regular Hemodialysis Patients in Haji Adam Malik Medan General Hospital.
DOI: 10.5220/0009863702210226
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 221-226
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
221

2 METHODS
2.1 Data Collection
This is an observational analytic study with cross-
sectional study design. Aim of this study is to
ascertain the relationship between anemia and RLS
in regular hemodialysis patients. The study was
conducted in October 2017 at the Adam Malik Haji
Hospital in Medan.
All patients undergoing hemodialysis therapy at
Adam Malik Haji Hospital in Medan and willing to
take part in the study and fulfill the inclusion and
exclusion criteria were included. Inclusion/exclusion
criteria: age 18 years old or older, patients who have
stably undergone hemodialysis more than 3 months,
not suffering or being treated from infection,
malignancy or drug / alcohol abuse, neurological
disorders, heart, lung and heart disease and have
complete data (what about blood transfusion?
Mostly HD with blood transfusion)
Data collected from primary data and secondary
data. Primary data is data obtained from interviews
for patient data and filling out questionnaires.
Secondary data obtained from medical records in the
form of laboratory results. (mention same result of
laboratory use for this research). Before data
collection from the sample is carried out, samples
that are in accordance with the inclusion and
exclusion criteria will be given a research
explanation and informed consent if agreed, the
hemodialysis patients can be used as research
samples. In this study, there were 106 patients who
participated in the study (How to calculate this 106
sample, How to choose the sample, for example,
consecutive sampling or convenience sampling the
author must write it )
Patients are diagnosed with RLS if they fulfill all
criteria by the International Restless Legs Syndrome
Study Group (IRLSSG). Patients who met the
criteria continued with interviews to determine the
degree of RLS based on the International RLS
Severity Scale (IRLS). What kind of research
instrument used in this research, what about ethical
clearance? Is valid and reliable? The author must
mention it clearly)
2.2 Statistical Analysis
All data were analyzed with statistical software
SPSS 22.0 using univariate, bivariate and
multivariate analysis with 95% confidence
interval.
Bivariate analysis was carried out using chi-square
to compare patients with and without RLS. Pearson
correlation examined the relationship between single
variables. Multinomial logistic regression was also
performed to investigate factors associated with
RLS, adjusting for covariates (more explanation
about using chi-square, person correlation, and
multivariate, what data using for each statistical
analytic).
3 RESULTS
Table 1. Of the 106 patients who attended the study,
all patients underwent HD 2 times a month. Men
have a higher prevalence than a woman (66% vs
34%). The Mean age of regular HD patients was
48.4 ± 13.29 with HD duration mean 24.2 ± 12.45.
Mean of hemoglobin level is 9.15 ± 1.47, SI 66.9 ±
33.7, TIBC 191.8 ± 58.8, transferrin saturation 37.3
± 19.61, ferritin levels 983.8 ± 932.86. The mean of
mineral level calcium is 8.13 ± 0.96, and phosphate
level is 5.6 ± 2.13. Of 32 patients (30.2%) with
respect to the severity of RLS, 4 patients classified
as mild (12.5%), 15 patients had moderate (46.9%),
9 had severe (28.1%) and 4 patients had very severe
(12.5%). 74 patients have no symptom of RLS.
(explanation the table used to after the table, not
before the table show).
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
222
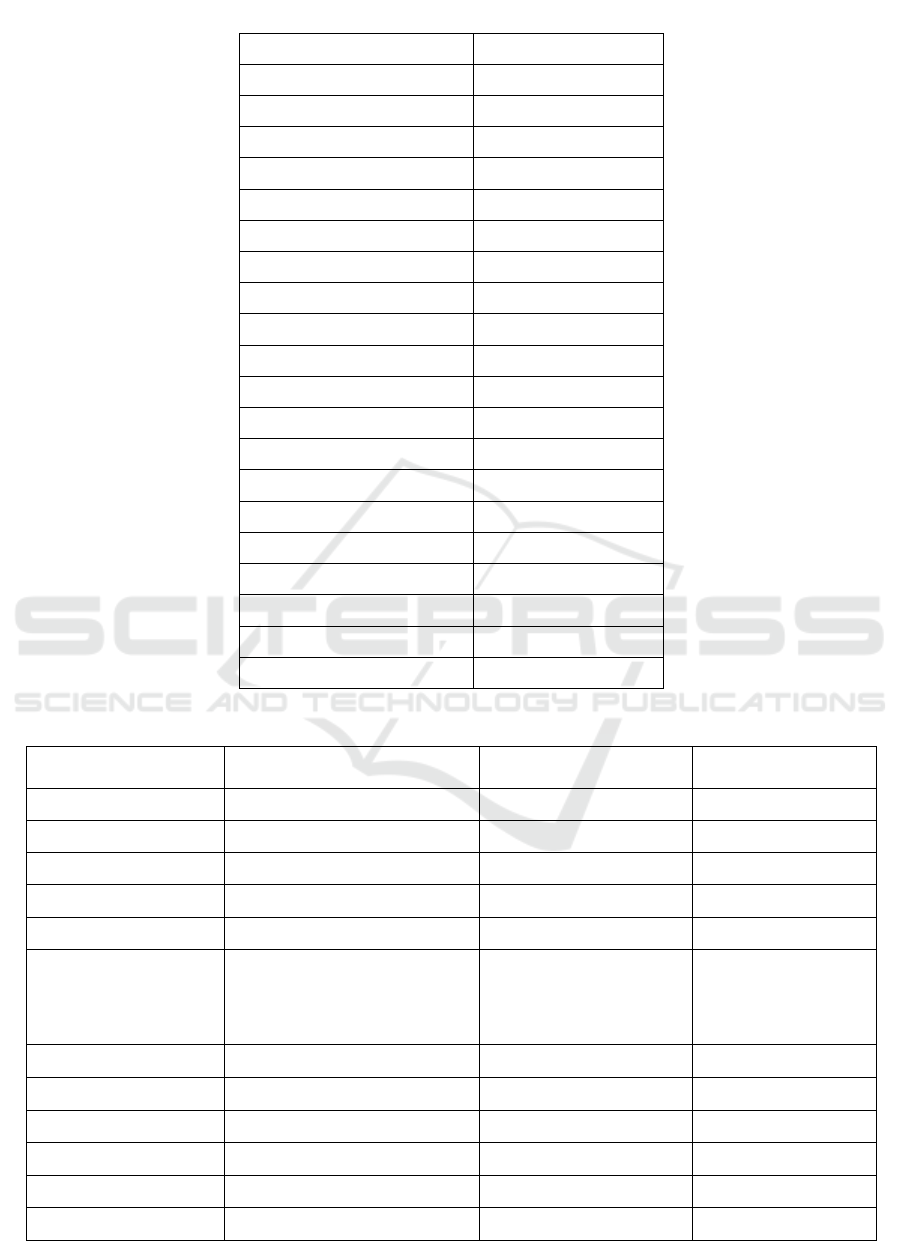
Table 1: Baseline characteristic regular hemodialysis patients in Haji Adam Malik General Hospital.
Variable n (%); Mean ± SD
Gender
Men 70 (66%)
Women 36 (34%)
Age (years) 48,4 ± 13,29
HD (month) 24,2 ± 12,45
Hb (gr/dL) 9,15 ± 1,47
SI (µg/dL) 66,9 ± 33,7
TIBC (µg/dL) 191,8 ± 58,8
Ferritin (µg/dL) 983,8 ± 932,86
ST (%) 37,3 ± 19,61
Ca (mg/dL) 8,13 ± 0,96
P (mg/dL) 5,6 ± 2,13
RLS
RLS 32 (30,2)
without RLS 74 (69,8)
RLS severity
Mild 4 (12,5)
Moderate 15 (46,9)
Severe 9 (28,1)
Very severe 4 (12,5)
Table 2: Characteristic of patients according to restless legs syndrome presence or absence
Tanpa RLS
(n = 74)
RLS
(n = 32)
P value
Gender 0,377
Men 51 (68,9) 19 (59,4)
Women 23 (31,1) 13 (40,6)
Age (years)
44,4 14,32 50,1 12,55
0,044*
HD (month)
25,2 12,76 23,8 12,08
0,604
Hb (gr/dL)
<10
>10
9,5 1,42
56
18
9,0 1,47
21
11
0,102
0,287
SI (µg/dL)
68,4 39,43 66,3 31,1
0,764
TIBC (µg/dL)
178,8 52,35 197,4 60,89
0,135
Ferritin (µg/dL)
893,3 952,94 1193 862,75
0,129
ST (%)
38,3 21,41 36,8 18,92
0,714
Ca (mg/dL)
8,3 0,84 8,1 1,01
0,251
P (mg/dL)
5,7 2,24 5,5 2,09
0,675
The Role of Anemia to Restless Legs Syndrome in Regular Hemodialysis Patients in Haji Adam Malik Medan General Hospital
223

We found age was significantly associated with
the incidence (prevalence) of RLS with p = 0.044,
where the mean age at RLS (50.1 ± 12.55) was older
than without RLS (44.4 ± 14.32). In this study long
HD was not significantly different between RLS and
without RLS. Anemia profile showed lower Hb
levels (Hb averaged 9,0 ± 1.47 vs. 9.5 ± 1.42), lower
SI and TSAT ?? levels and higher of TIBC and
ferritin level in RLS than without RLS. There was
no statistically significant difference in calcium and
phosphate levels in this study between RLS and
without RLS.
Table 3. Variables that have a value of p <0.25
are included in the multivariate analysis. From the
results of multivariate analysis, it was found that
RLS was influenced by levels of TIBC, Hb and age.
Table 3: Multinomial logistic regression predicting the
presence/ absence of restless legs syndrome
Variable OR P Value 95% CI
TIBC 1,010 0,020
1,002 1,019
Hb 0,697 0,038
0,496 0,981
Age 1,040 0,025
1,005 1,076
4 DISCUSSION
In this study, the prevalence of RLS in regular HD
patients was 30.2%. This prevalence is in
accordance with previous research reports using
IRLSSG where the prevalence of RLS in dialysis
patients was around 20% -62% (Saraji, et al., 2017).
This was also in line with previous studies by Marta
et al (12-25%), Scherer JS et al (10-20%) (Scherer
JS, et al., 2017), Guo et al (20-30%) (Guo, et al.,
2017), Rohani et al (37.4%) (Rohani, et al., 2015).
Higher incidence of RLS in HD patients is also
supported by data from various other studies such as
in Sao Paolo on 101 dialysis patients found 29
patients (28.7%) with RLS (Kim, et al., 2008), the
study of Zamani et al in Mashad Iran found RLS
prevalence reached 31.7% (Saraji, et al., 2017), and
Al-Jahdali et al with RLS prevalence of 50.22%
(Higuchi, et al., 2015). The prevalence that is quite
varied in various regions can be caused by
differences in race, culture, socio-economic status,
or available health facilities (Takaki, et al., 2003).
In this study, there was no relationship between
sex and RLS. In this study, RLS was more common
in men than in women as in the study by Takaki et al
(Takaki, et al., 2003). Previous studies by Kim et al
also showed the same thing (Kim, et al., 2008).
Gender does not affect the occurrence of RLS in
dialysis patients (Kim, et al., 2008). Differences
from previous studies may be explained by
differences in proportions in each study (Saraji, et
al., 2017).
The existence of a relationship that was
statistically significant between age and the
incidence of RLS was found in this study. The
average age of patients with RLS is higher than the
group without RLS. Although different from the
study by Jeong Min Kim et al who found age did not
affect the occurrence of RLS (Kim, et al., 2008).
Secondary RLS usually occurs in patients over 40
years of age and is associated with various
neurological disorders (Guo, et al., 2017). The
previous study has concluded that the prevalence
and severity of RLS levels that increase with age
suggest that the neurodegeneration process plays an
important role in the occurrence of RLS (Kim, et al.,
2008) (Guo, et al., 2017).
This is in line with the study of Saraji et al on
dialysis patients who showed an increase in the
prevalence of RLS with age (p = 0.002) (Saraji, et
al., 2017) and a study by Ki et al. Which showed a
tendency of RLS with age (Ki, et al., 2010).
In a previous study by Kim et al and Araujo et
al, The duration of dialysis did not affect the
occurrence of RLS in dialysis patients (Kim, et al.,
2008) (Araujo, et al., 2010). This study also showed
no association between the duration of hemodialysis
and the occurrence of RLS. The duration of dialysis
is not proven to improve or worsen RLS complaints.
Significant relationship between Hb level and
RLS (OR 0.697 0.496 ± 0.981, p = 0.038) can be
seen in this study. This is in accordance with the
study by Takaki et al (OR 0.741 0.551-0.997, p =
0.0475) (Takaki, et al., 2003). Precil et al. Also
proved that there was a relationship between Hb
levels <9.8 g / dL and the occurrence of RLS (OR
1.84 1.03-2.79, p = 0.040) (Neves, et al., 2017).
Similarly, Araujo et al. proved the association of
RLS in dialysis patients and decreased Hb (p
<0.005) (Araujo, et al., 2010). Based on the results
of a Meta-analysis study of 23 previous studies Mao
et al found lower Hb levels than patients without
RLS (Menezes, et al., 2018). Along with decreased
kidney function, there will be a decrease in the
production of erythropoietin which is the main cause
of anemia in kidney disease (Babitt & Lin, 2012).
Decreasing erythropoietin will cause a decrease in
erythropoiesis where in a way that is still not fully
(Kim, et al., 2008)known, reduce iron transport to
the central nervous system (CNS) and medulla
(Menezes, et al., 2018). Several recent studies have
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
224

shown that anemia, regardless of the iron content, is
a major cause of RLS (Menezes, et al., 2018).
However, several other studies are not in line with
this finding (Kim, et al., 2008).
Iron deficiency anemia is known to be one of the
risk factors for RLS (Kim, et al., 2008). Iron is
needed for recycling dopamine in the nervous
system and is the main cofactor for the regulation of
dopamine synthesis (eg Tyrosine hydroxylase)
(Scherer JS, et al., 2017). However, this is not very
clear in dialysis patients because of the use of iron
supplements in this population (Scherer JS, et al.,
2017). Iron deficiency in dialysis patients defined by
the Japanese Society for Dialysis Therapy (JSDT) is
serum ferritin levels <100ng / dL and TSAT <20%
(Higuchi, et al., 2015) (Yamamoto, et al., 2015). In
patients who meet the criteria will receive iron
supplementation both oral and intravenous (Kim, et
al., 2008). This, of course, can obscure the
relationship between serum iron and serum ferritin
and TSAT with RLS in this study (Kim, et al.,
2008). In this study, no significant association was
found between serum iron and TSAT with RLS in
line with Terumi et al (Higuchi, et al., 2015). In
addition, in some circumstances, RLS can be found
even though the serum iron value is normal
(Wijemanne & Ondo, 2017). This is because
peripheral iron values cannot describe the low iron
in the brain (Wijemanne & Ondo, 2017). Therefore a
neuropathological examination such as imaging
(MRI) and cerebrospinal fluid examination is needed
(Wijemanne & Ondo, 2017).
In this study, there was no association between
serum ferritin and TSAT in RLS patients and
without RLS. These results are in line with the study
by Terumi et al.who did not find any association
between serum ferritin and RLS (Higuchi, et al.,
2015). This is in contrast to the study of Guo et al.
who found an association of the degree of RLS with
ferritin values (Guo, et al., 2017). Mean serum
ferritin which tended to increase and lower TSAT in
RLS patients than patients without RLS showed that
ferritin values could not be used as deposit
predictors iron and can better describe iron status in
iron deficiency (Menezes, et al., 2018) (Saraji, et al.,
2017). In addition, iron supplementation also
obscures the relationship between them (Saraji, et
al., 2017). Ferritin levels can also be affected by
other factors such as inflammation and oxidative
stress (Higuchi, et al., 2015) (Babitt & Lin, 2012). In
this study, we have excluded patients in treatment,
infections, malignancies, and other factors that cause
inflammation based on interviews and physical
examinations. But this cannot rule out other
inflammatory factors. Therefore, in subsequent
studies, it is recommended to examine inflammatory
markers as monitoring.
From the bivariate analysis, we found a
significant relationship between the increase in
TIBC values and the occurrence of RLS. This is
something new in this study. Previous studies were
more likely to analyze hemoglobin, serum iron and
ferritin to see the iron status in the body (KDIGO,
2012). TIBC examinations to see as iron status
analysis are rare. Serum iron and TIBC comparison
values to see TSAT is more commonly found and
show insignificant results as in a study by Precil et al
and Terumi et al (Neves, et al., 2017) (Rohani, et al.,
2015) (Neves, et al., 2017) (Higuchi, et al., 2015).
Serum ferritin values that can be influenced by
factors such as inflammation also have a non-
significant relationship in RLS in this study.
Therefore, TIBC can be considered a marker for
assessing iron status in dialysis patients.
The relationship between phosphate levels to
RLS cannot be proven in this study. The calcium-
phosphate balance associated with RLS is
controversial (Saraji, et al., 2017). Study by Roberto
et al found an improvement in RLS complaints and a
decrease in phosphate levels after parathyroidectomy
(Menezes, et al., 2018), was not in line with other
studies by Filho et al., La manna et al, Terumi et al,
and Saraji et al. who also found no association
between phosphate and calcium levels with RLS
(Higuchi, et al., 2015) (Saraji, et al., 2017).
Of the 106 patients who took part in the study,
32 patients (30.2%) had RLS with mild severity of 4
patients (12.5%), moderate 15 patients (46.9%),
severe 9 patients (28,1%) and very severe 4 patients
(12.5%). Patients who did not experience RLS were
74 patients (69.8%). Based on the results of
statistical tests by comparing age, Hb levels and
TIBC values in light-to-moderate and severely
severe RLS patients no significant differences were
found between the two groups. The number of
samples and proportions may be the factors that
influence the results of the study. In addition, other
factors such as drug use and iron supplementation
can be biased.
This research is a cross-sectional study.
Therefore, the cause of the relationship cannot be
determined. There is limited research that has the
potential to be biased because of the limited sample
and data obtained from interviews such as medical
history, drug use (HD patients tend to consume more
drugs including benzodiazepines, gabapentin,
tricyclics) cannot play a role in RLS. Further
The Role of Anemia to Restless Legs Syndrome in Regular Hemodialysis Patients in Haji Adam Malik Medan General Hospital
225

research is needed to approach risk factors and
pathophysiology in RLS.
5 CONCLUSION
In this study, the prevalence of RLS in regular HD
patients is 30.2%. We found that RLS status was
influenced by Hb, TIBC, and age. RLS is often
found in HD patients but is still often undiagnosed
and untreated. RLS creates a disruption in quality of
life and increases mortality risk, therefore screening
for RLS is best done at health facilities that provide
services for renal replacement therapy especially
hemodialysis. The need for education about RLS for
HD patients to make it more routine for screening
(anemia) and prevention, especially for patients who
are older.
Pathophysiology of RLS is still unknown and
multifactorial, with the availability of complete data
and larger samples it is expected that other factors
related to RLS can be identified. In accordance with
the results of the study where low Hb levels and
high TIBC are significant risk factors, it is
recommended to correct anemia as prevention and
management of RLS.
REFERENCES
Araujo, S. et al., 2010. Restless legs syndrome in end-
stage renal disease: clinical characteristic and
associated comorbidities. J sleep, 11(8), pp. 789-790.
Babitt, J. & Lin, H., 2012. Mechanism of anemia in CKD.
JAm Soc Nephrol, Volume 23, pp. 1631-1634.
Guo, S. et al., 2017. Restless legs syndrome: from
pathophysiology to clinical diagnosis and
management. Front Aging Neurosci, 171(9), pp. 1-14.
Higuchi, T. et al., 2015. Association of Restless Legs
Patient syndrome with oxidative stress and
inflammation. Jsleep, Volume 16, pp. 941-948.
KDIGO, 2012. KDIGO Clinical practice guideline for
anemia in chronoc kidney disease. Kidney Int Suppl,
Volume 2, pp. 2279-2335.
Ki, K. et al., 2010. Prevalence, comorbidities and risk
factor of restlesslegs syndrome in the Korean elderly
population-result from the korean longitudinal study
on health and aging. J Sleep res, Volume 26, pp. 1976-
1983.
Kim, J. et al., 2008. Restless legs syndrome in patient on
hemodialysis. J Clin Neurol, Volume 4, pp. 153-157.
Menezes, A. F. d. et al., 2018. Restless legs syndrome in
dialysis patients: does dialysis modality influence its
occurence and severity. Int J Neph, Volume 2018, pp.
1-6.
Neves, P. et al., 2017. Effect of mineral and bone
metabolism on restless legs syndrome in hemodialysis
patients. J slsci, 13(1), pp. 89-94.
Rohani, M., Aghaei, M., Jenabi, A. & Yazdanfar, S., 2015.
Restless legs syndrome in hemodialysis patients in
Iran. Neurol Sci, 36(5), pp. 723-727.
Saraji, N., Hami, M., B, R. & Mojahedi, M., 2017.
Restless legs syndrome in chronic hemodialysis
patients in Mashad hemodialysis centers. J renal inj
prev, 6(2), pp. 137-141.
Scherer JS, Combs SA & Brennan F, 2017. Sleep
disorders, Restless Legs Syndrome and Uremic
Pruritus: Diagnosis and Treatment of common
symptoms in dialysis patients. AmJ Kidney Dis, 69(1),
pp. 117-128.
Suwitra, K., 2014. Penyakit Ginjal Kronik. 6 ed. Jakarta:
InternaPublishing.
Takaki, J. et al., 2003. Clinical and physilogical aspects of
restless legs syndrome in uremic patients on
hemodialysis. AmJ Kidney Dis, Volume 41, pp. 833-
839.
Wijemanne, S. & Ondo, W., 2017. Restless Leg
Syndrome: clinical features, diagnosis and practical
approach to management. Pract Neurol, Volume 17,
pp. 444-452.
Yamamoto, H. et al., 2015. Japanese study for dialysis
therapy: Guidelines for renal anemia in chronic kidney
disease. Renal replacement therapy, 3(36), pp. 1-46.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
226
