
The Comparison of Widal Titer in Healthy Individuals Living in
Good and Poor Sanitation Environment in Langsa City, Aceh
Province, Indonesia
Leni Afriani
1*
, Yosia Ginting
2
, Ricke Loesnihari
3
1
Tropical Medicine Program, Faculty of Medicine, Universitas Sumatera Utara, Jl. Dr. Mansyur No.5 Medan 20155,
Medan, Indonesia.
2
Division of Tropical and Infectious Disease, Department of Internal Medicine, Haji Adam Malik General Hospital, Medan,
Indonesia
³Departement of Clinical Pathology, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia.
Keywords: Typhoid, Salmonella, Sanitation, Widal Test, Indonesia
Abstract: Widal test is one of the diagnostic tools used to establish typhoid fever. However, the test may show false
positive particularly among healthy individuals living in a poor sanitation environment. The aim of this
study is to compare the titer of Widal test among healthy individuals living with good or poor sanitation. A
total of 180 healthy individuals resided in Langsa City were enrolled in the study between March and May
2018. Sanitation status of each individual was recorded, assessed and classified into good or poor sanitation.
Of these, 90 and 90 individuals were defined as having good and poor sanitation, respectively. The
proportion of positive Widal titer on Salmonella typhi O was 66.7% (60/90) in individuals with good
sanitation and 61.1% (55/90) among individuals with poor sanitation (P>0.05). However, conversion of S.
Typhi H was more frequent among healthy individuals living with poor sanitation (OR 3.348, 95 % CI =
1
.
754-6.390). We conclude that the sanitation level increased the antibody titers in the Widal test, and
therefore Widal test has limited use to diagnose typhoid fever. Further study is needed to evaluate
behavioral risk factors associated with increased Widal titer and the cut-off level for Widal titer in
population in Langsa City.
1 INTRODUCTION
One of the most common infectious diseases in
developing countries is typhoid fever. In 2003, the
World Health Organization (WHO) estimated
around 17 million cases of typhoid fever worldwide
with an incidence of 600.000 deaths every year.
Based on data from Basic Health Research in
Indonesia (RISKESDAS) in 2007, the prevalence of
typhoid fever in Indonesia reached 1.7%. However,
there is no report about typhoid prevalence in
RISKESDAS 2013. The highest prevalence was in
children aged 5-14 years (1.9%), followed by aged
1-4 years (1.6%), 15-24 years (1.5%) and ages less
than 1 year (0.8%). According to the WHO data
published in 2014 it is estimated that there are
around 21 million cases of typhoid fever worldwide
with death reaching 222 thousand people
(Masitoh
2009; Elisabeth 2016; WHO 2014). Data from
Langsa City General Hospital showed that from
2016 to 2018, typhoid fever was one of the top ten
diseases in hospitalized patients, which were
902(11%), 801(12%), and 1113(15%) cases,
respectively (Langsa City General Hospital Profile
2016-2018).
Typhoid fever is an acute systemic infectious
disease caused by gram-negative bacteria
Salmonella enterica serotype Typhi (Salmonella
typhi), a quick and precise diagnosis is needed as
early as possible in suspected patients having
typhoid fever in order to get the right treatment
immediately. Widal test is a modality which is often
used to diagnose typhoid fever (Putri Satwika 2016)
due to an easy, inexpensive, and relatively
noninvasive procedure which can be used as a
diagnostic value where blood culture is not available
(Alam et al 2011). The Widal test diagnostic value
is to address a significant increase of antibody titers
in blood against O (somatic) and H (flagellar)
antigen S. typhi. However, Widal test has a low
146
Afriani, L., Ginting, Y. and Loesnihari, R.
The Comparison of Widal Titer in Healthy Individuals Living in Good and Poor Sanitation Environment in Langsa City, Aceh Province, Indonesia.
DOI: 10.5220/0009862201460151
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 146-151
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
sensitivity and specificity, also have limitations in
interpreting the results, with many false positive and
false negative results due to the prevalence of basic
healthy titers in certain endemic or geographical
regions and sanitary conditions (Wardana et al 2014;
Jemilohun 2017; Chauhan 2016).
Data from the Langsa City Health Profile in 2014
reported one of the indicators of good environmental
condition was community-based total sanitation
(STBM). The number of villages implementing
STBM in Langsa Barat District is 100%, while in
Langsa Timur District 37.5%
(Langsa City Public
Health Department, 2014). Seeing the indicators of
environmental conditions that have not met the
requirements, it will be more likely the healthy
person will have positive results, thus when the
person had a fever, diagnostic errors often occur
(false positive). Therefore we want to assess the
difference in Widal titers of healthy individuals who
live in good sanitation compared to in poor
sanitation environments.
2 METHODS
This was an analytic observational study with a
cross-sectional design. This study was conducted in
Langsa City, located in Langsa Timur and Langsa
Barat District, from March to May 2018. The
samples were healthy individuals aged >18 years
who lived in environments with good sanitation
characteristics in Langsa Barat district and poor
sanitation characteristics in Langsa Timur district.
The initial assessment used an observation sheet on
basic environmental sanitation according to the
Minister of Health Decree No. 829 / Menkes / SK /
VII / 1999, covering assessment including clean
water facilities, latrines (sewage disposal facilities),
wastewater disposal facilities and waste disposal
facilities, with a total assessment of > or = 334
categorized as good sanitation criteria and <334 as a
poor sanitation criteria. A total sample of 180 people
was enrolled. Data collection used purposive
sampling method. Populations that meet the
inclusion criteria are subjects in good health, not
suffering fever (normal body temperature 36.5ºC -
37.2ºC), aged >18 years and residing in Langsa
Barat and Langsa Timur District. While the
exclusion criteria were subjects who were not
willing to take blood samples and participate in the
study.
Widal serological tests were performed on blood
samples from all study subjects to observe the
occurring agglutination
(Agarwal et al 2016), using
the "AIM" brand reagents which consisted of;
Antigen S. typhi H, S. paratyphi AH Antigen, S.
paratyphi BH Antigen, S. paratyphi CH Antigen, S.
Typhi O Antigen, S. paratyphi AO Antigen, S.
paratyphi BO Antigen and S. paratyphi CO Antigen.
All samples were taken directly to the Langsa City
General Hospital Laboratory for examination. The
procedure was carried out in accordance with the
Standard Operating Procedure of the Widal
examination at the Langsa City General Hospital
Laboratory.
Data processing using Statistical Package for the
Social Science (SPSS) version 22.0 was presented
descriptively to see the proportion of Widal titers of
healthy individuals in good environmental sanitation
and poor environmental sanitation. Analysis using
Chi-Square Test and Odds Ratio with significance
level p <0.05 and 95% confidence interval to assess
the relationship of risk factors with positive Widal
results.
This study has been approved by the Ethics
Committee of Faculty of Medicine, Universitas
Sumatera Utara with ethical clearance No. 158 /
DATE / KEPK FK USU-RSUP HAM / 2018.
3 RESULTS
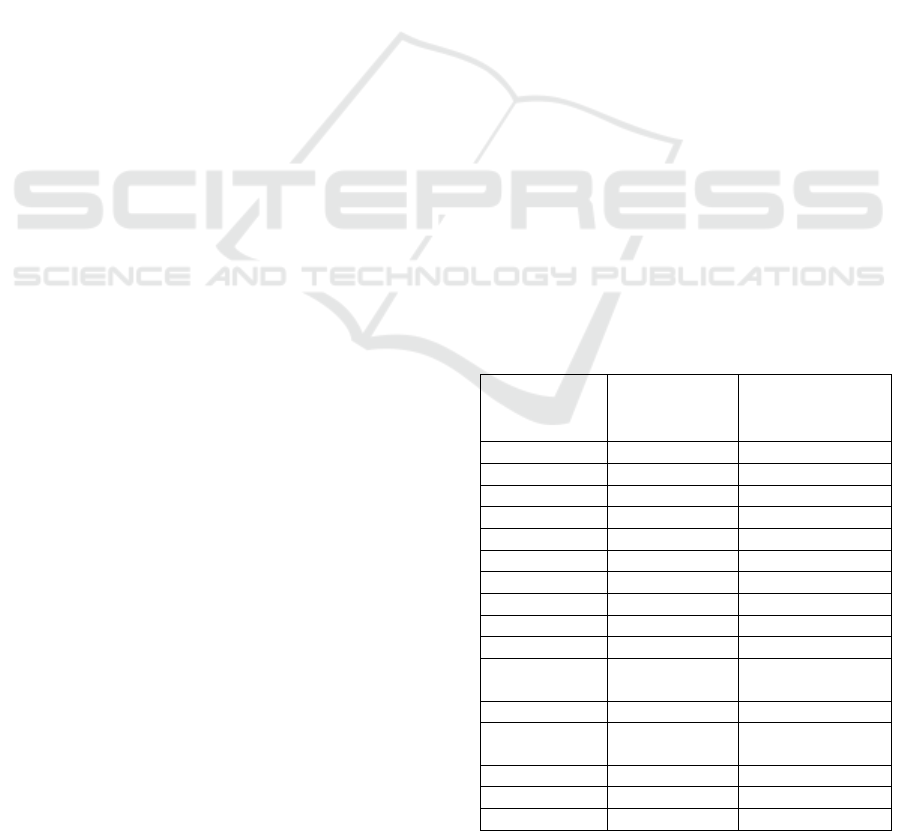
There was no difference in the age group between
the two study groups. Most of the participants were
educated until high school in both groups, 38 people
(42.2%) in the poor sanitation group and 48 (53.3%)
in the good sanitation group (see Table 1).
Table 1: Demographic characteristic of research subjects.
Demographic
Characteristi
c
Poor
Sanitation
(=90)
Good Sanitatio
n
(n=90)
Sex, n (%)
Man 28 (31.1) 33 (36.7)
Woman 62 (68.9) 57 (63.3)
Age, n (%)
< 20 year 3 (3.3) 1 (1.1)
20-29 year 17 (18.9) 20 (22.2)
30-39 year 28 (31.1) 20 (22.2)
40-49 year 16 (17.8) 17 (18.9)
50-59 year 16 (17.8) 21 (23.3)
≥ 60 year 10 (11.1) 11 (12.2)
Education, n
(%)
Uneducated 4 (4.4) 0
PS*
undergraduate
6 (6.7) 4 (4.4)
PS 11 (12.2) 6 (6.7)
JHS** 22 (24.4) 2 (2.2)
SHS*** 38 (42.2) 29 (32.2)
The Comparison of Widal Titer in Healthy Individuals Living in Good and Poor Sanitation Environment in Langsa City, Aceh Province,
Indonesia
147
University 9 (10) 48 (53.3)
Occupation, n
(%)
Housewife 40 (44.4) 19 (21.1)
Unemployed
2(2.2) 3 (3.3)
Entrepreneur
13 (14.1) 30 (33.4)
Student 4 (4.4) 4 (4.4)
Farmer 26 (28.9) 0
Civil
Servant
5 (5.6) 34 (37.8)
*primary school, **junior high school, ***senior high
school
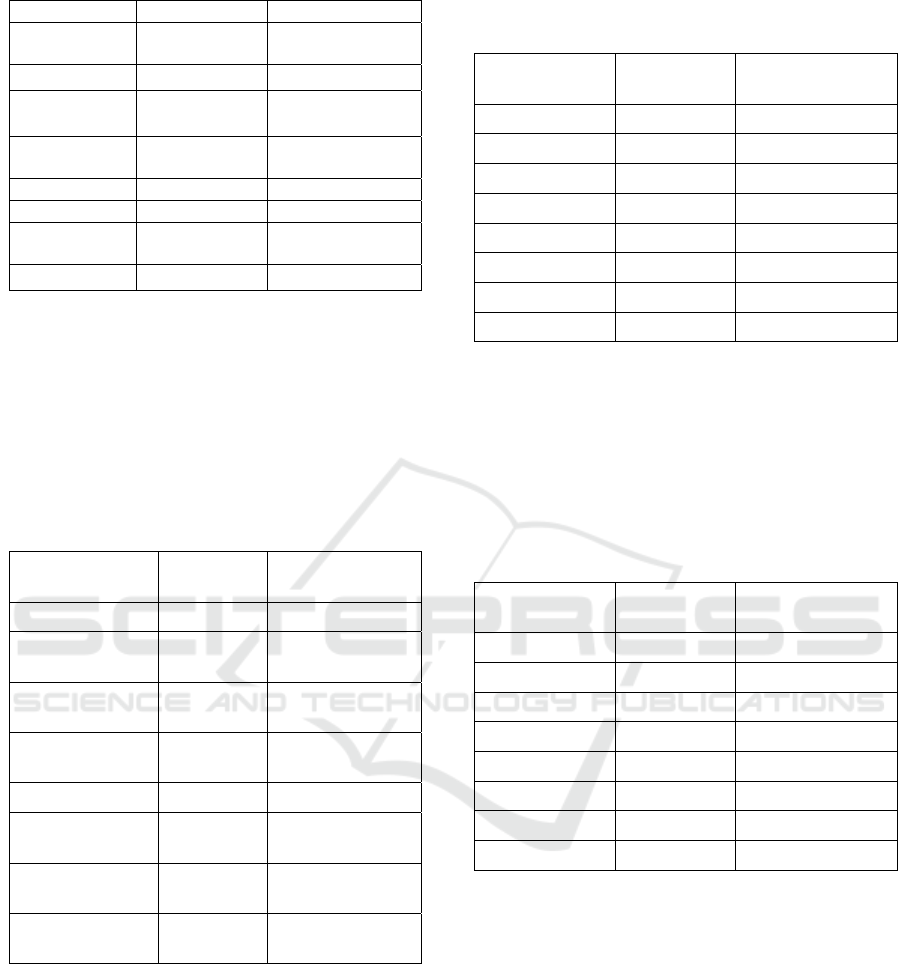
Conversion for Widal test was most occurred for
S. Typhi O in 115 people (63.9%), followed by
conversion for S. Typhi H in 64 people (35.6%).
While the smallest numbers of positive results in
Widal was for agglutinin S. paratyphi 35 people
(19.4%) (see Table 2).
Table 2 Widal test result from overall research subjects.
Agglutinin
Positive
(>1/80)
Negative (< or =
1/80)
S.thypi O, n (%) 115 (63.9) 65 (36.1)
S.parathypi AO,
n (%)
57 (31.7) 123 (68.3)
S.parathypi BO,
n (%)
60 (33.3) 120 (66.7)
S.parathypi CO,
n (%)
47 (26.1) 133 (73.9)
S.thypi H, n (%) 64 (35.6) 116 (64.4)
S.parathypi A H,
n (%)
35 (19.4) 145 (80.6)
S.parathypi B H,
n (%)
36 (20) 144 (80)
S.parathypi CH,
n (%)
37 (20.6) 143 (79.4)
According to the study group, the conversion for
Widal test in the good sanitation group was for S.
thypi O as many as 60 people (66.7%), followed by
S. parathypi agglutinin AO as many as 33 people
(36.7%) The smallest positive results were 13 people
(14.4%) on agglutinin S. paratyphi B H (see Table
3).
Table 3 Comparison of Healthy Individual Widal Titer in
Good Sanitation Environment in Langsa City.
Agglutinin
Positive (>
1/80)
Negative (< or
=1/80)
S.typhi O 60 (66.7) 30 (33.3)
S.paratyphi A O 33 (36.7) 57 (63.3)
S.paratyphi B O 30 (33.3) 60 (66.7)
S.paratyphi C O 32 (35.6) 58 (64.4)
S.typhi H 20 (22.2) 70 (77.8)
S.paratyphi A H 15 (16.7) 75 (83.3)
S.paratyphi B H 13 (14.4) 77 (85.6)
S.paratyphi C H 16 (17.8) 74 (82.2)
While in the poor sanitation group, the agglutinin
conversion was more likely to occur in S. Typhi O
(55 people, 61.1%), followed by agglutinin S. typhi
H as many as 44 people (48.9%), and the least likely
to occur in agglutinin S. Paratyphi CO in 15 people
(16.7%) on (see Table 4).
Table 4 Comparison of Healthy Widal Individual Titer in
Poor Sanitation Environment in Langsa City.
Agglutinin
Positif ( >
1/80 )
Negative ( < atau =
1/80 )
S.typhi O 55 (61.1) 35 (38.9)
S.paratyphi A O 24 (26.7) 66 (73.3)
S.paratyphi B O 30 (33.3) 60 (66.7)
S.paratyphi C O 15 (16.7) 75(83.3)
S.typhi H 44 (48.9) 46 (51.1)
S.paratyphi A H 20 (22.2) 70 (77.8)
S.paratyphi B H 23 (25.6) 67 (74.4)
S.paratyphi C H 21 (23.3) 69 (76.7)
In Langsa Barat district, the highest percentage
of S. Typhi O agglutinin was 1/320 titer in 42 (46%)
subjects. Whereas in East Langsa Timur District, S.
Typhi O agglutinin titers were obtained with the
highest percentage was 1/80 titers in 35 (38.9%)
subjects (see Table 5).
Analysis of the Widal test results between the
subjects who live in the area with good and poor
sanitation are presented in table 6. People living in
poor sanitation were more likely to show agglutinin
S. typhi H (OR = 3.348, 95% CI, P<0.001), S.
paratyphi A H (OR = 1.429, 95% CI, P<0.346), S.
paratyphi B H (OR = 2.033, 95% CI, P<0.062), S.
paratyphi C H (OR = 1.408, 95% CI, P<0.356).
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
148
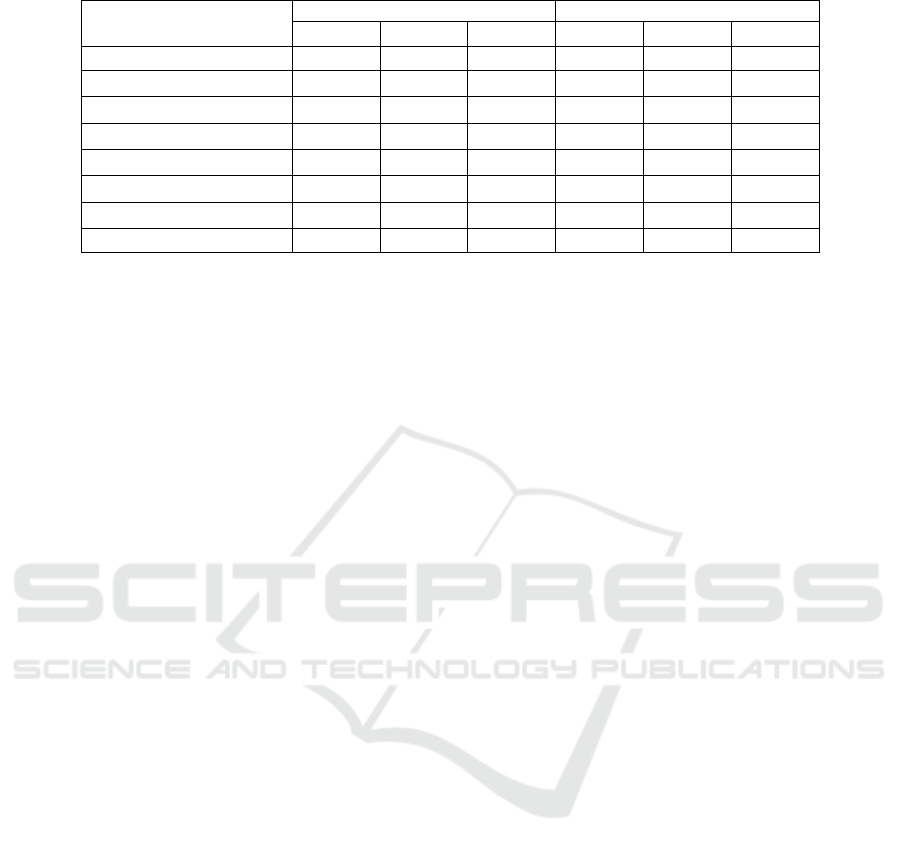
Table 5 Percentage of Widal Titer in the Good Sanitation and Poor Sanitation Area in Langsa City.
Agglutinin
Good Sanitation (n=90) Poor Sanitation (n=90)
1/80 1/160 1/320 1/80 1/160 1/320
S. Typhi O, n(%) 30(33.3) 18(20) 42(46.7) 35(38.9) 34(37.8) 21(23.3)
S. paratyphi AO, n(%) 57(63.3) 22(24.4) 11(12.2)
66(73.3)
18(20) 6(6.7)
S. paratyphi BO, n(%) 60(66.7) 20(22.2) 10(11.1)
60(66.7)
25(27.8) 5(5.6)
S. paratyphi CO, n(%) 58(64.4) 19(21.1) 13(14.4)
75(83.3)
12(13.3) 3(3.3)
S. Typhi H, n(%) 70(77.8) 8(8.9) 12(13.3)
46(51.1)
24(26.7) 20(22.2)
S. paratyphi AH, n(%) 75(83.3) 10(11.1) 5(5.6)
70(77.8)
9(10) 11(12.2)
S. paratyphi BH, n(%) 77(85.6) 8(8.9) 5(5.6)
67(74.4)
15(16.7) 8(8.9)
S. paratyphi CH, n(%) 74(82.2) 11(12.2) 5(5.6) 69(76.7) 11(12.2) 10(11.1)
4 DISCUSSION
Our study showed there is an influence of the level
of sanitation on the results of S. Typhi H. agglutinin
test, where individuals living in poor sanitation was
more likely to have positive results compared to
individuals living in a good sanitation environment.
This result is in line with other studies which have
described the results of Widal test rely on sanitary
conditions, the prevalence of basic titers of healthy
residency in certain endemic and geographical
regions
(Wardana et al 2014; Jemilohun 2017;
Chauhan 2016).
Poor environmental sanitation and health
conditions affect the yield of high titers. In addition,
several factors such as nutritional condition at the
time of test, prior administration of antibiotics,
immunological status, vaccination, use of
immunosuppressive drugs, cross-reaction with other
Enterobacteriaceae and Widal test methods used
also affect the results. These factors are not further
evaluated in this study. The increase in titer of
agglutinin H alone without an increase in agglutinin
O should not be used to diagnose typhoid fever
(Zorgani et al 2014), but may help in diagnosing
suspected typhoid fever in adult patients from non-
endemic areas or in children less than 10 years old in
endemic area, due to the possibility of contact with
S. Typhi in subinfection doses. Thus, if Widal is still
needed to support the diagnosis of typhoid fever, the
threshold for referral titers, both in children and
adults, needs to be determined
(Gaikwad et al 2014).
Widal results on 180 total blood samples from
the study subjects showed an agglutination reaction
between antibodies with Widal antigen. Widal tests
were considered positive if the antibody titer is
1/160 (Loho et al 2000), both for agglutinin O and H
with single or combined diagnostic criteria if a
single criterion is used. Furthermore, agglutinin O is
also found to be more diagnostic than agglutinin H
(Zorgani et al 2014). In this study, we found more
than 50% of the healthy individuals studied were
positive for Widal test (titer>1/80). This is in line
with Chauhan's (2016) study in Uttar Pradesh, India
that among 250 healthy individuals who were
performed Widal test, 56.8 % of them showed a titer
of 1/80 for anti-0 and anti-H antibodies, leading to
set this titer as the baseline titer for diagnosing
typhoid fever
(Chauhan 2016). Having known the
titer for the conversion of Widal test among our
population in Langsa, we set up a titer of 1/80
against antibody H to be used for the diagnosis of
typhoid fever.
Based on the results of Widal test of healthy
individuals in the two sanitation area groups, the
most frequent positive test result was for agglutinin
S. thypi O in 60 people (66.7%) in good sanitation
and in 55 people (61.1%) in poor sanitation. This
shows that Salmonella agglutinin is generally found
in individuals who appear to be healthy and not
suffering from fever when having their blood
examined in different populations and sanitation. It
also concluded that the Widal test is easy to
applicate but has limitations in endemic areas,
including Indonesia
(Suryani et al 2018). Therefore,
if the Widal test is still needed to support the
diagnosis of typhoid fever, the threshold for
reference titers for both children and adults needs to
be determined
(Zorgani et al 2014).
The Comparison of Widal Titer in Healthy Individuals Living in Good and Poor Sanitation Environment in Langsa City, Aceh Province,
Indonesia
149
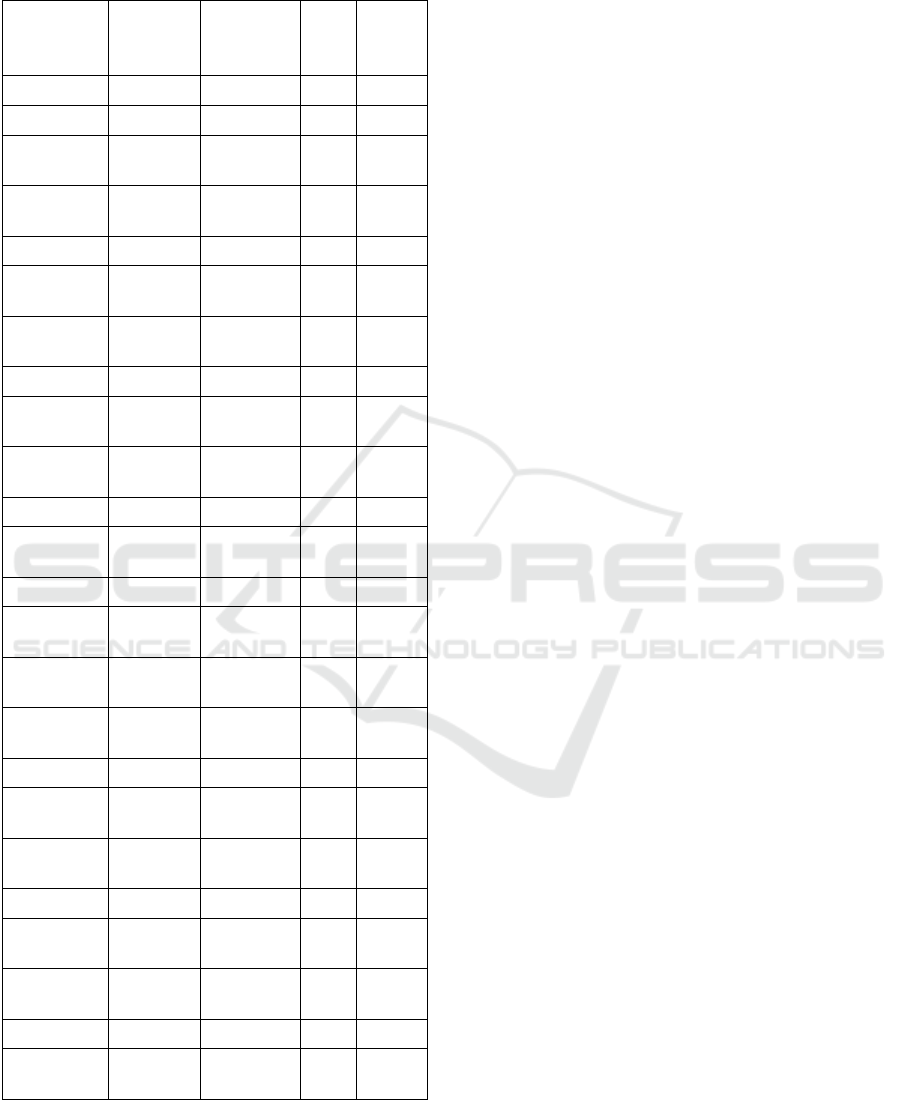
Table 6 Differences in Widal Test Results Based on
Environmental Sanitation Conditions.
Agglutinin
Poor
Sanitation
n=90
Good
Sanitation
n=90
Ρ OR
95%CI
S. typhi O
Positive 55 (61.1) 60 (66.7) 0.438 0.786
Negative 35 (38.9) 30 (33.3)
0.427-
1.446
S. paratyphi
A O
Positive 24 (26.7) 33 (36.7) 0.149 0.628
Negative 66 (73.3) 57 (63.3)
0.333-
1.184
S. paratyphi
B O
Positive 30 (33.3) 30 (33.3) 1.000 1.000
Negative 60 (66.7) 60 (66.7)
0.538-
1.859
S. paratyphi
C O
Positive 15 (16.7) 32 (35.6) 0.004 0.363
Negative 75(83.3) 58 (64.4)
0.180-
0.732
S. Typhi H
Positive 44 (48.9) 20 (22.2)
<0.00
1
3.348
Negative 46 (51.1) 70 (77.8)
1.754-
6.390
S. paratyphi
A H
Positive 20 (22.2) 15 (16.7) 0.346 1.429
Negative 70 (77.8) 75 (83.3)
0.679-
3.008
S. paratyphi
B H
Positive 23 (25.6) 13 (14.4) 0.062 2.033
Negative 67 (74.4) 77 (85.6)
0.956-
4.325
S. paratyphi
C H
Positive 21 (23.3) 16 (17.8) 0.356 1.408
Negative 69 (76.7) 74 (82.2)
0.679-
2.916
Our study also showed the highest value of
agglutinin was at 1/320, this was also reported in
another study by Bahadur and Peerapur (2013) in
healthy individuals in Karnataka, India
(Bahadur et
al 2013). Thus, if the same Widal titer obtained from
patients with suspected typhoid fever who seek
treatment at health care facilities in Langsa City,
relying on Widal as the only diagnostic laboratory
test of typhoid fever will generate a misleading
diagnosis, with a false positive possibility. When
blood culture is compared to the Widal test for the
diagnosis of typhoid fever, the specificity of the
Widal test reduced significantly. Of 270 individuals
with suspected typhoid fever and positive O and H
antibodies, 74.4% were negative in blood culture
and only small proportion was positive for S. Typhi
(N=7, 2.6%) and S. paratyphi (N=1.5%) (Andualem,
2014). Therefore, it is very important to do more
accurate tests such as culture to confirm typhoid
fever.
5 CONCLUSION
This study showed there was an increase in Widal
titers of healthy individuals in good and poor
sanitation environment in Langsa City. Healthy
individuals living in poor sanitation environment
were at risk of having 3.348 times positive S. Typhi
Widal titers compared to healthy individuals living
in good sanitation environment. Widal test,
therefore, can give a false-positive interpretation in
the diagnosis of typhoid fever and should be used
with other tools with better specificity. There are
limitations in this study, particularly in factors
related to high yield titer. Further study is needed to
evaluate behavioral risk factors associated with
increased Widal titer and the cut-off level for Widal
titer in population in Langsa City.
REFERENCES
Agarwal Y, Gupta D, Sethi R. Enteric Fever: Resurrecting
the epidemiologic footprints. Astrocyte.
2016;3(3):153-61.
Alam ABM, Rupam FA, Chaiti F. Utility of a single
Widal test in the diagnosis of typhoid fever.
Bangladesh J Child Health. 2011;35(2):53-58
Andualem G, Abebe T, Kebede N, Gebre-Selassie S,
Mihret A. A comparative study of Widal test with
blood culture in the diagnosis of Typhoid fever in
febrile patients. BMC Res Notes. 2014 Sep;7(1): p.
653. Available at:
https://ojs.unud.ac.id/index.php/eum/article/view/1768
1. [Cited 2018 March].
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
150

Bahadur AK, Peerapur B V. Baseline titer of Widal
amongst healthy blood donors in Raichur, Karnataka.
JKIMSU. 2013;2(2):30–6.
Chauhan S. Study of baseline Widal titer amongst
apparently healthy individuals in and around
Muzaffarnagar City of Uttarpradesh, India.
International Journal of Pharma and BioSciences.
2016 Feb;7(1):p.152–155.
Dinas Kesehatan Kota Langsa. 2014. Profil kesehatan
Kota Langsa tahun 2014. Langsa: Dinas Kesehatan
Kota Langsa
Elisabeth Purba I, Wandra T, Nugrahini N, Nawawi S,
Kandun N. Program pengendalian demam tifoid di
Indonesia: tantangan dan peluang. Media Penelitian
dan Pengembangan Kesehatan [Internet].
2016;26(2):99–108. Available from:
http://ejournal.litbang.kemkes.go.id/index.php/MPK/ar
ticle/view/5447
Gaikwad UN, Rajurkar M. Diagnostic efficacy of Widal
slide agglutination test against Widal tube
agglutination test in enteric fever. Int J Med Public
Health. 2014 Jul;4(3):227-30
Jemilohun AC. How useful is the Widal test in modern
clinical practice in developing countries? A review.
IJTDH. 2017;26(3):1-11
Loho T, Sutanto H, Silman E. In: Demam tifoid peran
mediator, diagnosis, dan terapi (Editor: Zulkarnain).
Pusat Informasi dan Penerbitan bagian Ilmu Penyakit
Dalam. 2000:22-42
Masitoh D. Hubungan antara perilaku higiene
perseorangan dengan kejadian demam tifoid pada
pasien rawat inap di Rumah Sakit Islam Sultan
Hadlirin Jepara Tahun 2009. Skripsi. UNNES. 2009
June;1:58-65.
Rumah Sakit Umum Daerah Kota Langsa. 2018. Profil
RSUD Kota Langsa Tahun 2016-2018. Langsa:
Rumah Sakit Umum Daerah Kota Langsa
Putri Satwika, Anak Agung; Lestari, A.A. Wiradewi. Uji
diagnostik tes serologi Widal dibandingkan dengan tes
IgM Anti Salmonella Typhi sebagai baku emas pada
pasien suspect demam Tifoid di Rumah Sakit Surya
Husadha pada bulan Januari sampai dengan Desember
2013. E-Jurnal Medika Udayana. 2016 Jan;1:1-18
Suryani DY. Shodikin MA, Astuti IS. Widal titre among
healthy population in University of Jember. E-Jurnal
Pustaka Kesehatan.2018 May;6(2):245-250
Wardana IMTN, Herawati S, Yasa IWPS. Diagnosis
demam Typhoid dengan pemeriksaan Widal. E-Jurnal
Med Udayana. 2014;3(2):237-50.
WHO. WHO International. [Online].; 2014 [cited 2018
March. Available from:
www.wpro.who.int/philippines/typhoon_haiyan/media
/Typhoid_fever.pdf.
Zorgani A, Ziglam H. Typhoid fever: misuse of Widal test
in Libya. J Infect Dev Ctries. 2014;8(6):680-687
The Comparison of Widal Titer in Healthy Individuals Living in Good and Poor Sanitation Environment in Langsa City, Aceh Province,
Indonesia
151
