
Bacterial Pattern and Antibiotic Susceptibility in the Perinatology
Unit of Haji Adam Malik General Hospital Medan, Indonesia
Nisa Nurjannah
1*
, Beby Syofiani Hasibuan
2
1
Faculty of Medicine, Universitas Sumatera Utara, Dr. Mansyur st. 5, Medan, Indonesia
2
Department of Pediatrics, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
*Corresponding author
Keywords: bacterial pattern, antibiotic susceptibility, neonatal sepsis
Abstract: Neonatal sepsis affects the high mortality and morbidity rates of the newborns. The causative bacteria are
different between countries or hospitals, it affects the choice of antibiotics usage. Irrational antibiotic
administration can cause resistance problem and aggravate patients’ conditions. Culture and sensitivity test
can be done to determine the species of bacteria and their antibiotic susceptibilities, allowing appropriate
and rational antibiotic administration. This is a retrospective observational descriptive study, describing the
bacterial pattern and antibiotic susceptibility of patients admitted to the perinatology ward at Haji Adam
Malik General Hospital in 2016. Neonates suspected with sepsis underwent blood culture and sensitivity
test. Secondary data from the medical record was obtained using total sampling method. Of 97 subjects, and
neonatal sepsis patients were found predominantly in males (68%). Aterm neonates who had sepsis (75.3%)
with late-onset sepsis were more dominant (87.6%). Mean age of neonatal sepsis patients was 14.9 days.
Acinetobacter baumannii was the most common etiology (19.6%), the most sensitive antibiotics were
amikacin (57.7%) and levofloxacin (57.7%). In addition, antibiotic with the highest resistance is cefotaxime
(74.2%).
1 INTRODUCTION
The first 28 days of life are the most vulnerable
periods in human’s life. One of the main causes of
neonatal death is sepsis and with lack of proper
treatment, the mortality rates will increase.
Therefore, sepsis is still a problem in the field of
neonatology to date (Rasyidah, 2014; Wardlaw et
al., 2014; World Health Organization, 2016)
.
Bacteria that cause sepsis are different for each
country and each hospital so that will affect the
selection of antibiotics. The Centers for Disease
Control and Prevention (CDC) estimates that as
many as 50% of antibiotics prescriptions are not
optimal or not necessary (Rasyidah 2014; Schulman
et al. 2015).
Antibiotics are drugs commonly used in the
Neonatal Intensive Care Unit (NICU). Irrational use
of antibiotics at the NICU will increase the adverse
events, such as increased morbidity, mortality, costs,
hospital length of stay and is also associated with
antibiotic resistance problem.
In order to use antibiotics rationally, the most
likely etiology and the susceptibility patterns should
first be identified (Irene et al. 2013; Katarnida et al.
2013; Schulman et al. 2015). This study objective is
to describe the bacterial pattern of neonatal sepsis
and antibiotics susceptibility in Perinatology of Unit
Haji Adam Malik General Hospital, Medan,
Indonesia in 2016.
2 METHOD
This study was a retrospective observational
descriptive study based on medical records in Haji
Adam Malik General Hospital, Medan, Indonesia in
2016. All perinatology unit patients in Haji Adam
Malik General Hospital suspected with sepsis who
underwent blood culture and sensitivity test during
2016 was included in this study, using total sampling
technique. If data from medical records were not
complete or could not be read, the samples were
excluded. Data were then analyzed with statistical
software. This study was approved by the Research
Nurjannah, N. and Hasibuan, B.
Bacterial Pattern and Antibiotic Susceptibility in the Perinatology Unit of Haji Adam Malik General Hospital Medan, Indonesia.
DOI: 10.5220/0009861601150118
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 115-118
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
115
Ethics Committee, Faculty of Medicine, Universitas
Sumatera Utara, Medan, Indonesia.
3 RESULTS
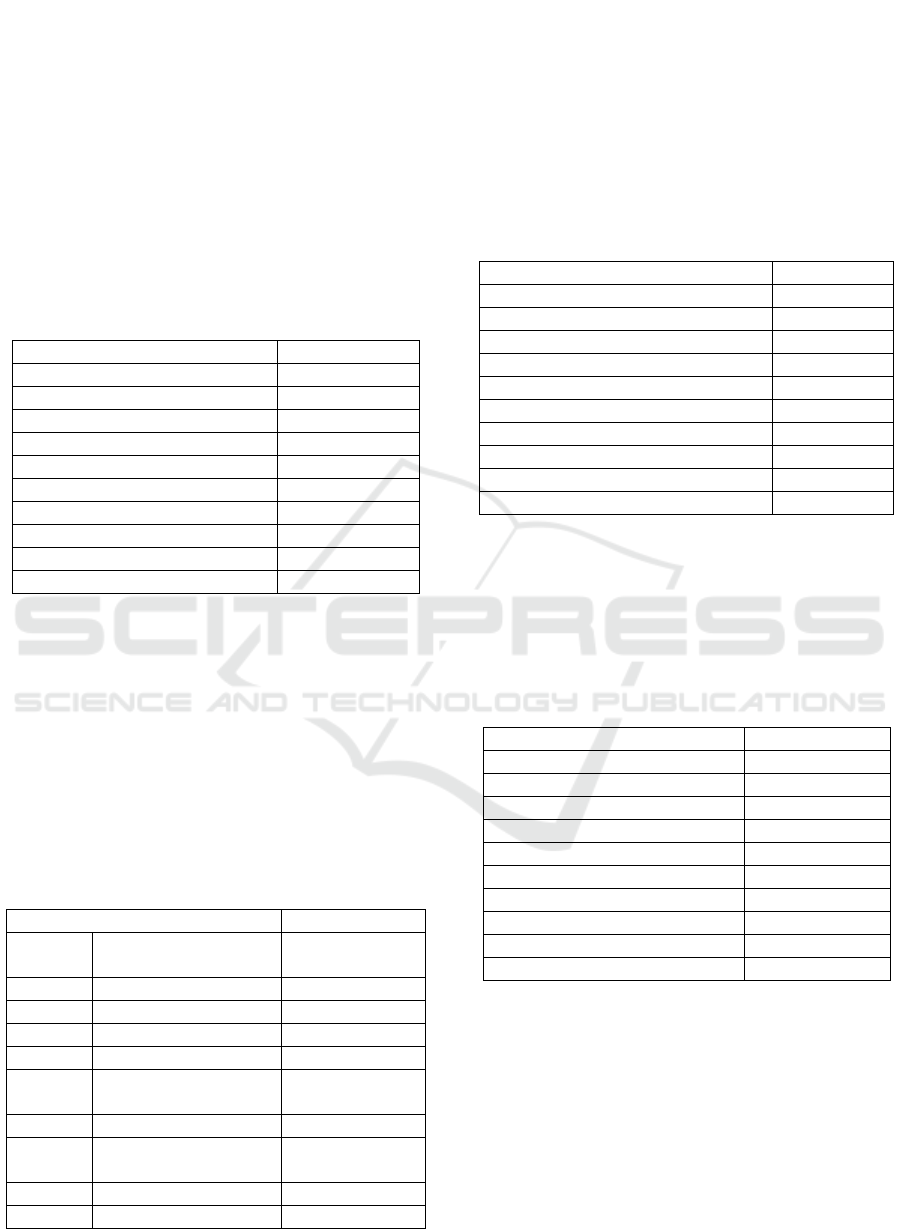
Table 1 shows the baseline characteristics of
patients. Male patients were more common in this
study (68%), 75.3% were term neonates, and late-
onset sepsis was more commonly found (87.6%).
The subject’s mean of age was 14.8 days.
Table 1: Characteristics of neonates with positive blood
culture in Haji Adam Malik General Hospital during 2016.
Characteristics n=97
Gender, n (%)
Boys 66 (68)
Girls 31 (32)
Gestational week, n (%)
Preterm 24 (24.7)
Atom 73 (75.3)
The onset of sepsis, n (%)
Early 12 (12.4)
Late 85 (87.6)
Mean of age, days (SD) 14.88 (8.14)
Table 2 shows the cause of neonatal sepsis in
this study. Gram-negative bacteria were the most
common etiology found in neonatal sepsis, with
Acinetobacter baumanii as the leading organism
(19.6%), followed by Klebsiella pneumonia
(16.5%). The most common gram-positive bacteria
found in neonatal sepsis was Staphylococcus
haemolyticus (6.2%) followed by Bacillus spp
(4.1%).
Table 2: Bacteria and the etiology of neonatal sepsis in
Haji Adam Malik General Hospital.
Bacteria Percentage (%)
Gram-
negative
Acinetobacter
baumannii
19.6
Klebsiella pneumonia 16.5
Enterobacter cloacae 8.2
Burkholderiacepacia 4.1
Pantoeaspp 4.1
Gram-
positive
Staphylococcus
haemolyticus
6.2
Bacillus spp 4.1
Staphylococcus
epidermidis
3.1
Clostridium spp 2.1
Enterococcus faecium 2.1
Table 3 shows that amikacin (57.7%) and
levofloxacin (57.7%) as the most sensitive
antibiotics obtained from the susceptibility test on
bacteria that cause neonatal sepsis on the
perinatology unit. Those were followed by
meropenem and ciprofloxacin, and
cefoperazone/sulbactam with sensitivity rates of
45.4%, 41.2%, and 35.1%, respectively.
Table 3: Antibiotic susceptibility in neonatal sepsis in Haji
Adam Malik General Hospital.
Antibiotics n (%)
Amikacin 56 (57.7)
Levofloxacin 56 (57.7)
Meropenem 44 (45.4)
Ciprofloxacin 40 (41.2)
Cefoperazone/Sulbactam 34 (35.1)
Doxycycline 33 (34.0)
Imipenem 31 (32.0)
Gentamicin 27 (27.8)
Tetracycline 21 (21.6)
Fosfomycin 21 (21.6)
Table 4 showed that cefotaxime, as one of the
cephalosporin group antibiotics, had the highest
resistance rate in this study (74.2%), followed by
ampicillin and ceftriaxone with resistance rates of
73.2% and 72.2% respectively.
Table 4: Antibiotic resistance in neonatal sepsis in Haji
Adam Malik General Hospital.
Antibiotics n (%)
Cefotaxime 72 (74,2)
Ampicillin 71 (73,2)
Ceftriaxone 70 (72,2)
Ceftazidime 66 (68,0)
Gentamicin 55 (56,7)
Ampicillin/Sulbactam 53 (54,6)
Tetracycline 47 (48,5)
Amoxicillin / Clavulanic acid 44 (45,4)
Netilmicin 41 (42,3)
Meropenem 37 (38,1)
In this study, we found that Klebsiella
pneumonia and Enterobacter cloacae were still
sensitive to amikacin (100%). On the other hand,
Bacillus spp. had a high sensitivity rate to
Ciprofloxacin (100%). Enterobacter cloacae had the
highest resistance to antibiotics such as cefotaxime,
ampicillin, and ceftriaxone, with resistance rate to
each antibiotic at 100%, respectively.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
116

4 DISCUSSION
Neonatal sepsis in this study was found to be more
common in males. This is similar to other studies
which stated that males were more common to have
neonatal sepsis than females. There are several
factors that might be associated with it. First is
Glucose-6-Phosphate Dehydrogenase (G6PD)
deficiency. It is a genetic defect that affects males
more than females and this defect increases the risk
of infection. Other studies showed that factors
associated with gamma globulin synthesis were
located on the X chromosome so that immunological
protection on females was better than males (Far Z
et al. 2016; Verma et al. 2017).
Neonatal sepsis in this study was more
predominant in term neonates. It was similar to the
study by Afridi, in 2015 where a term neonates were
more commonly found to have neonatal sepsis than
preterm neonates. It might be due to the more
vulnerable preterm babies to have neonatal sepsis
with higher mortality rates which caused them a
delay to reach the health facilities. This situation
caused more a term neonates to be more often to be
diagnosed with neonatal sepsis.
Late-onset sepsis was associated with
horizontal transmissions, such as very low birth
weight in preterm neonates. It was due to the
immaturity of the immune system, prolonged
mechanical ventilation, prolonged length of hospital
stay, vascular catheterization, and other invasive
procedures. Those factors made opportunist
pathogens, like Acinetobacter baumannii, could
infect neonates easier (Shah and Padbury 2014; Wei
et al. 2015).
The most common bacteria isolated from
neonatal sepsis in this study was Acinetobacter
baumannii, an opportunist bacteria that become
pathogen in immunocompromised subjects and
worsen in neonatal infection (Wei et al. 2015). Study
in Iran comparing bacterial patterns in two decades
found that in 1992 the most common bacteria were
Staphylococcus aureus (59%) while in 2015 the
most common was coagulase-negative
Staphylococci (CoNS) (33.9%). It showed that
bacterial pattern changed over time and was
different in every center (Radfar et al. 2017).
Most bacteria isolated from this study were still
sensitive to amikacin and had a high resistance to
cefotaxime. The previous study in Haji Adam Malik
General Hospital Medan showed that vancomycin
had high sensitivity rate while ampicillin,
gentamicin, and cefotaxime had high resistance
rates. It explained that there were no significant
antibiotics susceptibilities changes in neonatal sepsis
during these recent years in Haji Adam Malik
General Hospital Medan (Sianturi et al. 2012).
5 CONCLUSION
The most frequent etiology of neonatal sepsis was
Acinetobacter baumannii. Amikacin and
levofloxacin were the most sensitive antibiotics
while cefotaxime was the least.
ACKNOWLEDGMENTS
The researchers especially thank, to the counselor,
Haji Adam Malik General Hospital for giving
permission to the researchers.
REFERENCES
Far Z, Rostami et al. 2016. Glucose 6 Phosphate
Dehydrogenase as A Risk Factor of Male Neonatal
Sepsis. Journal of Medicine and Life 9(1): 34–38.
Irene, Yuniar, Mulya Rahma Karyanti, Taralan Tambunan,
and Nanda Asyura Rizkyani. 2013. Evaluasi
Penggunaan Antibiotik Dengan Kartu Monitoring
Antibiotik Gyssens. Sari Pediatri 14(6): 384–90.
Katarnida, Sri Sulastri, Mulya Rahma Karyanti, Dewi
Murniati Oman, and Yusticia Katar. 2013. Pola
Sensitifitas Bakteri Dan Penggunaan Antibiotik.Sari
Pediatri 15(2): 122–26.
Radfar, Mitra, Minoo Fallahi, Mohammad Kazemian, and
Samira Borhani. 2017. A Comparative Evaluation of
Microbial Pattern and Antibiotic Susceptibility in a
Level III NICU between Two Decades. Pediartric
Infections Research Center 5(2): 2–7.
Rasyidah. 2014. Pola Kuman Dan Uji Kepekaan
Antibiotik Pada Sepsis Neonatorum Di Unit
Perawatan Neonatus. Sari Pediatri 3(1): 431–36.
Schulman, J. et al. 2015. Neonatal Intensive Care Unit
Antibiotic Use. PEDIATRICS 135(5): 826–33.
http://pediatrics.aappublications.org/cgi/doi/10.1542/p
eds.2014-3409.
Shah, Birju A, and James F Padbury. 2014. Neonatal
Sepsis, An Old Problem with New Insights. Virulence
5(1): 170–1778.
Verma, Pradeep et al. 2017. Neonatal Sepsis:
Epidemiology, Clinical Spectrum, Recent
Antimicrobial Agents and Their Antibiotic
Susceptibility Pattern.” International Journal of
Contemporary Pediatrics 2(3): 176–80.
http://www.ijpediatrics.com/index.php/ijcp/article/vie
w/465/429.
Wardlaw, Tessa et al. 2014. UNICEF Report: Enormous
Bacterial Pattern and Antibiotic Susceptibility in the Perinatology Unit of Haji Adam Malik General Hospital Medan, Indonesia
117

Progress in Child Survival but Greater Focus on
Newborns Urgently Needed. Reproductive Health: 1–
4.https://reproductive-health-
journal.biomedcentral.com/articles/10.1186/1742-
4755-11-82.
Wei, Hsui-Mei et al. 2015. Multidrugs-Resistant
Acinetobacter Baumannii Infection Among Neonates
in A Neonatal Intensive Care Unit At A Medical
Center in Central Taiwan. Journal of Microbiology,
Immunology and Infection 48(1): 531–39.
World Health Organization. 2016. Newborns: Reducing
Mortality.http://www.who.int/mediacentre/factsheets/f
s333/en/.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
118
