
Von Willebrand Factor and Thrombocytopenia in Patients with
Dengue Haemorrhagic Fever
L. Mutiara
1*
, Herman Hariman
2
, Stephen C. L. Koh
2
, Adang Bachtiar
3
1
Division of Tropical Medicine, Murni Teguh Memorial Hospital, Medan Indonesia
2
Department of Clinical Pathology, Faculty of Medicine, Universitas Sumatera Utara/Haj Adam Malik Hospital,
Medan Indonesia
3
Department of Public Health Program, Cipto Mangunkusuma Hospital, Universitas Indonesia, Jakarta, Indonesia
Keywords: DHF, endothelium status
Abstract: The clinical manifestation of DHF includes mild or marked febrile syndromes with abrupt onset of
headache, pain behind the eyes, muscle and bone pain, nausea, vomiting and rash. The pathophysiology of
DHF in human is complex involving endothelial cell activation and the impaired endothelial barrier leading
to plasma leakage triggering the activation of the haemostatic system. The objective of this study was to
determine Von Willebrand Factor levels and platelet effects on the vascular endothelium in patients with
dengue haemorrhagic fever. Fifty patients (males 34, females 16), were recruited, Grade 1 (n=41), Grade 2
(n=6), Grade 3 (n=2) and Grade 4 (n=1) DHF. Twenty patients at seventeen years and below (Grade 1) were
compared with 21 adults (Grade 1) showed no statistical differences and grouped together for analysis.
Blood sampling to determine haemoglobin, haematocrit, platelets and Von Willebrand Factor (VWF) at the
febrile, defervescence and convalescent phases was performed. The patients were aged between 4 and 54
years old with Grade 2 patients being significantly older (P=0.03) than Grade 1 DHF. Comparisons between
Grades 1 and 2 DHF showed no statistical differences in the parameters studied. Thrombocytopenia,
elevated VWF levels from normal was evident in all phases suggesting endothelial activation. In Grades 3
and 4 DHF, thrombocytopenia, elevated VWF was also seen. No mortality was observed in the study.
Endothelial activation was evident in dengue haemorrhage fever.
1 INTRODUCTION
Dengue fever is the most serious consequence of
mosquito-borne infection worldwide. There are
more than 2.5 billion persons at risk of infection and
occur mainly in the sub-tropical regions of Asia,
Africa and America (WHO 2008), the attacks have
shifted mainly to adults (WHO 2011). In Indonesia,
the overall incidence increased significantly from
0.05/100,000 in 1968 to 35-40/100,000 in 2013
(Karyanti et al 2014).
The actual numbers of dengue cases are
underreported or misclassified (WHO 2017).
Clinical manifestations of dengue include mild or
marked febrile syndromes of abrupt onset with
headache, pain behind the eyes muscle and bone
pain, nausea, vomiting and rash which is life
threatening. There is no specific treatment for
dengue fever but maintaining patients’ body fluid
volume is critical. Dengue as defined by WHO
(2009) as dengue with and without warning signs of
plasma leakage and defined into four grades (Grades
1 to 4) The endothelium plays an important
regulatory role in the circulation as a physical barrier
and involved in the control of thrombosis and
thrombolysis, vascular tone and growth of blood
vessels (Verhamme & Hoylaerts 2006). Endothelial
activation may be responsible for plasma leakage
and shock (De Castro et al 2007) and endothelial
injury is associated with elevated Von Willebrand
Factor (VWF) (Connolly 1991, Mohle et al 1997).
Thrombocytopenia is commonly observed in both
mild and severe dengue syndrome and associated
with clinical outcome (WHO 2009, Mourao et al
2007, Schexneiden & Reely 2005, Honda et al
2008). The level of platelet count correlates with
severity of DHF and high haematocrit with marked
thrombocytopenia support the diagnosis of dengue
shock syndrome (DSS) (WHO 2011) and has been
considered as an important factor responsible for
bleeding events in DHF (Diaz-Quijano et al 2010).
Platelet activation is significantly increased in
106
Mutiara, L., Hariman, H., Koh, S. and Bachtiar, A.
Von Willebrand Factor and Thrombocytopenia in Patients with Dengue Haemorrhagic Fever.
DOI: 10.5220/0009861401060110
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 106-110
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
dengue-patients especially with thrombocytopenia
which exhibited signs of apoptosis pathway
activation (Hottz et al 2013)
The objective of the study was to determine Von
Willlebrand Factor levels and platelet effects on the
vascular endothelium in patients with dengue
haemorrhagic fever.
2 MATERIALS AND METHODS
The study received ethical approval from the Health
Research Ethical Committee (No.438/TGL/KEPK
FK USU-RSUP-HAM/2018), Faculty of Medicine,
University of North Sumatera, Jakarta, Indonesia.
The study was conducted at the Murni Teguh
Memorial Hospital, Medan Indonesia. Subjects.
Fifty patients (males 34, females 16) admitted to the
hospital with fever were recruited and diagnosed
according to WHO protocol (2009) to have Grade 1
(n=41), Grade 2 (n=6), Grade 3 (n=2) and Grade 4
(n=1) DHF. The Inclusion criteria: patients who met
WHO criteria for dengue fever and willing to take
part in the study and had one or more dengue
serology positive for either IgM/IgG or NS1,
Exclusion criteria: patients with other infections and
systemic diseases and not willing to take part in the
study. Normal Controls. Fifteen normal subjects
(males n=14, female n=1) who are normotensive and
not taken any medication, no history of health issues
was recruited to serve as normal controls for the
DHF study.
Blood Sampling and Laboratory Investigation.
EDTA blood was used to determine Haemoglobin
(Hb), Haematocrit (Hct) and platelets in the Siemens
high volume haematological analyser (Advia
2120/1); Citrated plasma for Elisa analysis of Von
Willebrand Factor (VWF) (USCN Life Sciences,
Wuhan, China). Statistical Analysis. The Statistical
Package for Social Sciences (SPSS 22 IBM Corp)
was used to perform statistical analysis. The
independent t-test for differences between groups at
different phases of febrile, defervescence and
convalescence and Analysis of Variance (ANOVA)
was performed. A P-value of <0.05 was considered
statistically significant.
3 RESULTS
Comparison of parameters (mean ± SD) studied in
dengue haemorrhagic fever at febrile phase (Grade
1) between cohorts at age seventeen and below and
above 17 years.
There were twenty cohorts (males n=13, females
n= 7) at seventeen years and below and twenty-one
cohorts (males n=14, females n=7) above 17 years
old. Except for the significance in age (P=<0.001)
there were no statistical significance in haemoglobin
(Hb), haematocrit (Hct), platelets and VWF studied
(Table 1). They were therefore combined (Grade 1)
for further statistical analysis.
Table 1. Comparison of parameters (mean and SD) in dengue haemorrhage fever at febrile stage (Grade 1) between cohorts
at age seventeen years and below and above.
≤ 17 years
>17 years P
N (male/female) 20 (13/7) 21 (14/7)
Age years 10.9 (3.9) 29.8 (9.0)
<0.001
Range years 4 – 17 18 - 54
Haemoglobin g//L 13.1 (1.3) 14.1 (2.1) 0.06
Haematocrit % 39.0 (4.4) 42.2 (6.2) 0.07
Platelets x10
9
/L 111.7 (82.5) 73.1 (50.7) 0.05
VWF ng/mL 108.4 (29.0) 111.0 (30.7) 0.78
Normal values for VWF. Of the fifteen normal
controls studied, the level of VWF were non-
detectable in fourteen controls and one at 83.1
ng/mL (sensitivity of assay <0.94 ng/mL) mean 11.9
± 31.4 ng/mL. The VWF levels of DHF at various
phases are shown in Figure 1.
Von Willebrand Factor and Thrombocytopenia in Patients with Dengue Haemorrhagic Fever
107
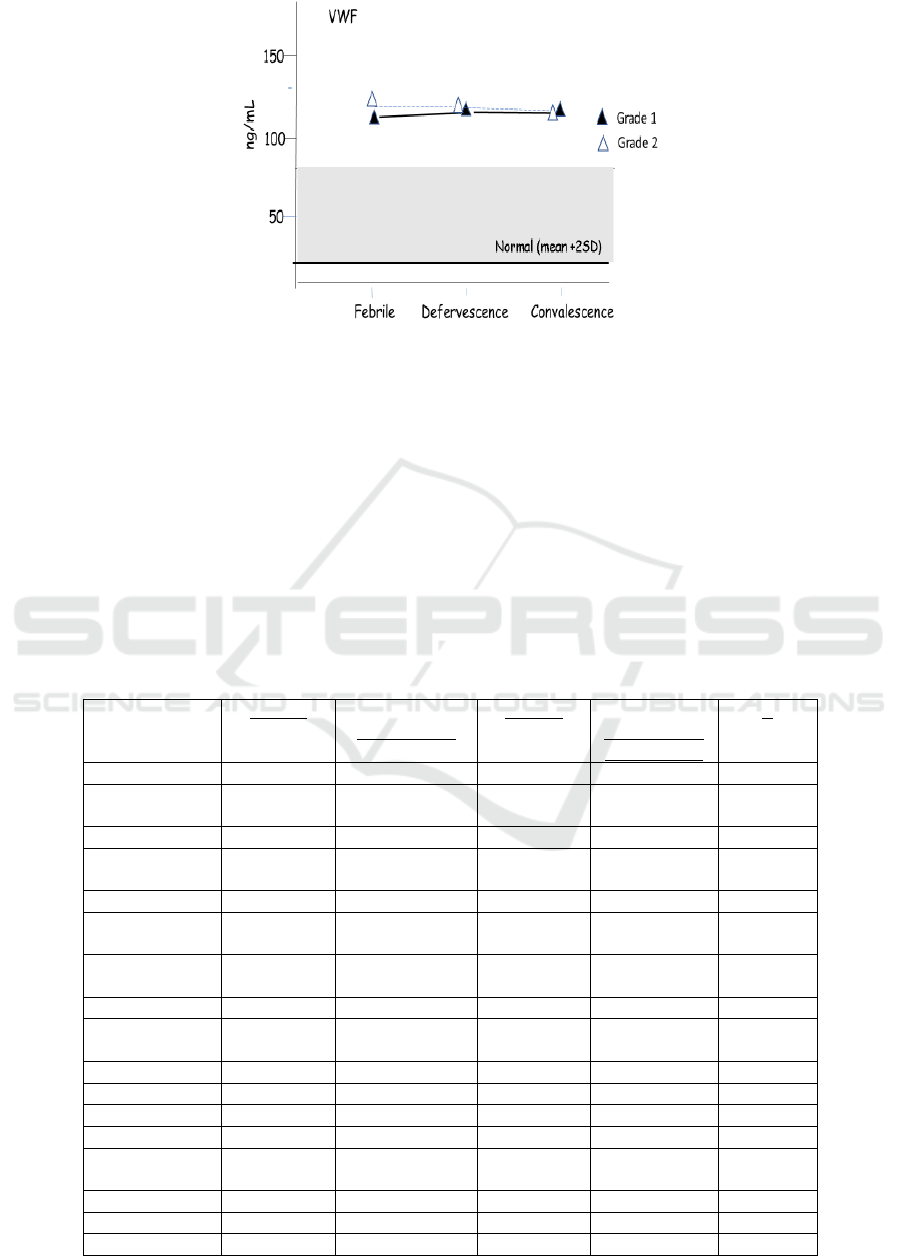
Figure 1.VWF in Grades 1 and 2 DHF at febrile, defervescence and conva;escence phases compared to normal controls
(mean +2SD)
Dengue haemorrhagic fever: Comparison of Hb,
Hct, platelets and VWF (mean ± SD) between
Grades 1 and 2 at febrile, defervescence and
convalescence phases and comparison to febrile
phase. Thrombocytopenia (platelets <100 x10
9
/L)
was evident in both Grades 1 and 2 DHF at febrile,
defervescence and convalescence phases with
normal haematocrit and haemoglobin levels seen.
Elevated VWF levels are seen but they were not
significantly different between Grades 1 and 2.
There were also no significant differences between
the two groups of cohorts in the parameters studied.
Similarly, no differences when compared to febrile
phase (Table 2). Analysis of Variance (ANOVA)
One-way ANOVA analysis for Hb, Hct, platelets
and VWF. in either Grades 1 or 2 between different
DHF phases showed no significant differences (not
shown).
Table 2. Dengue haemorrhage fever: Comparison of parameters studied (mean and SD) between Grades 1 & 2 at febrile,
defervescence and convalescence phases and compared to febrile phase.
Grade 1
Grade1 – P vs
Febrile phase
Grade 2 Grade 2- P vs
Febrile phase
(Gr1 vs Gr 2)
P
Febrile
N
(male/female)
41 (28/13) 6 (4/2)
0.03
Age years 20.6 (11.8) 30.8 (8.7) 0.46
Haemoglobin
g//L
13.6 (1.8) 14.3 (2.1) 0.45
Haematocrit % 40.6 (5.6) 42.8 (6.1) 0.4
Platelets x10
9
/L 94.8 (70.9) 70.5 (60.4)
0
VWF ng/mL 109.7 (29.6) 120.0 (29.1) 0.4
Defervescence
Haemoglobin
g//L
13.6 (1.7) 0.93 14.2 (2.0) 0.91 0.49
Haematocrit % 41.2 (6.6) 0.64 41.4 (8.3) 0.75 0.96
Platelets x10
9
/L 78.4 (51.3) 0.23 66.5 (413) 0.90 0.54
VWF ng/mL 114.0 (24.9) 0.48 112.3 (26.1) 0.37 0.89
Convalescence
Haemoglobin
g//L
13.2 (1.7) 0.35 13.6 (1.8) 0.65 0.63
Haematocrit % 40.1 (5.3) 0.68 40.4 (5.6) 0.50 0.91
Platelets x10
9
/L 101.8 (58.8) 0.63 97.0 (55.3) 0.45 0.85
VWF ng/mL 113.7 (24.8) 0.51 114.3 (13.0) 0.68 0.9
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
108

4 DISCUSSION
Dengue fever is the most serious consequence of
mosquito-borne infection worldwide. Endothelial
damage may also be caused by the virus itself.
Thrombocytopenia is responsible for bleeding events
in DHF (Diaz-Quijano et al 2010, Orsi et al 2013)
but many factors can contribute to the onset of
thrombocytopenia from a reactive immune response
against platelets and decreased platelet production
(Lin et al 2001, De-Castro et al 2007, Saito et al
2004), platelet activation and apoptosis (Hottz et al
2013). Bleeding manifestations and plasma leakage
are complications seen in dengue and bleeding
manifestation in adults may occur in the absence of
plasma leakage (Wichmann et al 2004). In our study,
thrombocytopenia was observed in all phases of
DHF even though in convalescence phase the mean
platelet numbers were higher than febrile and
defervescence phases they did not reach statistical
significance. Normal haemoglobin level and no
haemoconcentration was observed indicating no
bleeding episodes occurred despite the
thrombocytopenia. Endothelial activation as evident
by elevated VWF level suggest the possibility of
plasma leakage in Grades 1 and 2 DHF. Other
evidence like activation of the coagulation system
and thrombocytopenia with haemoconcentration will
support the cause of dengue shock syndrome (WHO
2011) and bleeding episodes (Diaz-Quijano et al
2010) which was not seen in our cohorts. Identifying
the mechanisms affecting DHF would improve
diagnosis and management therapy. No mortality
was recorded in our study.
5 CONCLUSION
Thrombocytopenia and elevated VWF are seen in
dengue haemorrhagic fever despite normal
haemoglobin and haematocrit levels suggesting
endothelial activation.in dengue haemorrhagic fever.
ACKNOWLEDGEMENTS
The authors wish to express their sincere gratitude to
the staff of the research laboratories at the Medical
Faculty, University of Sumatera Utara and Murni
Teguh Memorial Hospital for their expert technical
assistance.
CONFLICT OF INTEREST
The authors declared that they have no Conflict of
Interest.
REFERENCES
Connolly DT. Vascular permeability factor: a unique
regulator of blood vessel function. J Cell Biochem
1991; 47:219-23.
Diaz-Quijano FA, Villa-Centeno LA, Marinez-Vega RA.
Predictors of spontaneous bleeding in patients with
acute febrile syndrome from a dengue endemic area. J
Clin Virol 2010; 49:11-5.
Honda S, Saito M, Dimano EM et al. Increased of
phagocytosis of platelets from patients with secondary
dengue virus infection by human macrophages. Am J
Trop Med Hyg 2009; 80:841-5
Hottz ED, Oliviera MF, Nunes CG et al. Dengue induces
platelet activation, mitochondrial dysfunction and cell
death through mechanisms that involve DC-SIGN and
caspases. J Thromb Haemostas 2013; 11:951-62.
Karayanti MK, Ulterwaal CSPM, Kusriantuti R et al. The
changing incidence of dengue haemorrhagic fever in
Indonesia: a 45-year registry-based analysis. BMC
Infectious Diseases 2014; 14:412
http://www.biomedcentral.com/1471:2334/14/412.
Lin CF, Lei HY, Liu CC et al. Generation of IgM anti-
platelet autoantibody in dengue patients. J Med Virol
2001; 63 (2):143-9..
Mohle R, Green D, Moore MAS, Nachman RL, Rafil S.
Constitutive production of thrombin-induced release
of vascular endothelial growth factor by human
megakaryocytes and platelet. Proc Natl Acad Sci
1997; 94:663-8.
Mourao MP, Lacerda MV, Macedo VO, Santos JB.
Thrombocytopenia in patients with dengue virus
infection in the Brazilian Amazon. Platelets 2007;
18:605-12.
Orsi FA, Angerami RN, Mazetto BM et al. Reduced
thrombin formation and excessive fibrinolysis are
associated with bleeding complications in patients
with dengue fever: a case-control study comparing
dengue fever patients with and without bleeding. BMC
Infect Dis 2013; 13:250-6.
Saito M, Oishi K, Inoue S et al. Association of increased
platelet-associated immunoglobulins with
thrombocytopenia and the severity of disease in
secondary dengue virus infections. Clin Exp Immunol
2004; 138 (2):299-303
Schexneider KL, Reedy EA.Thrombocytopenia in dengue
fever. Curr Hematol Rep 2005; 4:145-8.
Verhamme P, Hoylaerts MF. The pivotal role of the
endothelium in haemostasis and thrombosis. Acta
Clinica Belgica 2006; 61 (5):213-9.
Wichmann O, Hongsinwon S, Bowonwatanuwong C,
Chotivanich K, Sukthana K, Pukrittayakmee S. Risk
factors and clinical features associated with severe
Von Willebrand Factor and Thrombocytopenia in Patients with Dengue Haemorrhagic Fever
109

dengue infection in adults and children during the
2001 epidemic in Chonburi, Thailand. Trop Med Int
Health, 2004; 9 (9):1022-9.
World Health Organisation (WHO). Dengue and dengue
haemorrhagic fever Factsheet No. 117, Geneva,
Switzerland WHO 2008.
World Health Organisation (WHO). Dengue: guidelines
for diagnosis, treatment, prevention and control New
ed., Geneva Switzerland, World Health Organisation
2009.
World Health Organisation (WHO). Comprehensive
guidelines for prevention and control of dengue and
dengue haemorrhagic fever. Revised and expanded
version WHO 2011.
World Health Organisation Media Centre. Dengue and
severe dengue. WHO Factsheet updated 2017.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
110
