
Risk Factor Analysis and Outcomes of VAP in ICU Patients
at Arifin Achmad General Hospital in 2018:
Cohort Retrospective Study
Fachriani Putri
1*
, Riza Iriani Nasution
1,2
Ridha Restilla
1
, Misyenni Rumaisya
1
1
Department of Public Health, Faculty of Medicine, University of Riau
2
Infection Prevention And Control Committee, Arifin Achmad General Hospital, Riau Province
*Corresponding author
Keywords: risk factors, outcome, Ventilator-associated pneumonia.
Abstract: Ventilator associated pneumonia (VAP) is a nosocomial pneumonia that occurs 48 hours or more after
mechanical ventilator usage through the endotracheal tube or the tracheostomy tube. VAP is one of the
nosocomial infections often found in the intensive care unit (ICU). The purpose of this study was to
determine the risk factors and outcomes of VAP. This study used a retrospective cohort design involving all
ICU patients at Arifin Achmad General Hospital in 2018 who met the inclusion criteria. The incidence of
VAP was 3.1% (95% CI 2.76 - 3.43). The onset of VAP that occurred within 5 days was 66.7%. A
significant factor was history of pulmonary disease (p = 0.04) with an RR of 8.2 (95% CI 1.7 - 40.1). There
was a significant correlation between the incidence of VAP and length of ICU stay (p = 0.002). The
incidence of VAP in Arifin Achmad General Hospital in 2018 was 3.1%. The onset of VAP incidence is
still within 5 days, so the prognosis is still good. Doctors and paramedics should pay more attention to ICU
patients who have a history of pulmonary disease.
1 INTRODUCTION
The incidence of pneumonia after mechanical
ventilation usage increases 3–10 times (Augustyn,
2007), and may causes nosocomial pneumonia if its
usage is more than 48 hours, either with
endotracheal tubes or after tracheostomy and is
called Ventilator-Associated Pneumonia (VAP)
(Hunter, 2005; Patricia , Dorrie, & Barbara, 2012)
Ventilator Associated Pneumonia (VAP) causes
an increase in morbidity and mortality of patients
that were treated in The Intensive Care Unit (ICU)
(Kahlil, 2017)
The incidence of VAP is quite high, varying
between 9-27% with a mortality rate of more than
50%. The incidence of VAP in Cipto
Mangunkusumo Hospital (RSCM) was 27.4% with a
mortality rate of 57.2% (Saragih, 2014). At
Pamukkale University Hospital, Denizli, Turkey for
38.1% with a mortality rate of 70.3% (Erbay, 2004).
VAP data on patients treated in the ICU and CVCU
rooms at Arifin Achmad General Hospital in Riau
Province was increasing from 3.3% in 2013 to
18.58% in 2015 (Nency, 2015).
There are two risk factors that may increase the
incidence of VAP, they were intervention factors
and patient factors. Intervention factors include
endotracheal intubation, duration of use of
mechanical ventilation, length of hospital stay, use
of Endotracheal Tube (ETT), catheters, central
venous pressure measurement, inappropriate use of
antibiotics, red blood cell transfusion, supine
position, and post-surgery.While the patient factors
include age over 60 years, gender, and Chronic
Obstructive Pulmonary Disease (COPD) (Gillepspie,
2009).
According to Saragih (2014), research on VAP in
Indonesia has not been comprehensive. Most of the
patients were lack of knowledge in VAP and do not
have health insurance, so they were admitted in
severe conditions. This resulted in more frequent
occurrences of VAP. VAP is one of the causes of
morbidity and mortality in ICU but also causes the
prolonging of the patient stay which may result in
the increasing cost of treatment (Wiryana, 20007).
80
Putri, F., Nasution, R., Restilla, R. and Rumaisya, M.
Risk Factor Analysis and Outcomes of VAP in ICU Patients at Arifin Achmad General Hospital in 2018: Cohort Retrospective Study.
DOI: 10.5220/0009859400800086
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 80-86
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
This study was to determine the risk factors and
outcomes of VAP in ICU patients at Arifin Achmad
General Hospital during 2018.
2 METHODS
This study was an analytical study with a
retrospective cohort design. General and clinical
data during treatment were obtained from the
register book. The study was conducted in March
2019 at Arifin Achmad General Hospital in Riau
Province. The population in this study were all data
on patients using mechanical ventilators who were
admitted to the ICU in January-December 2018. The
samples in this study were all of the populations that
met the inclusion criteria using a total sampling
technique.
The inclusion criteria in this study were all
patients who used mechanical ventilators for more
than 48 hours in the ICU and had complete data
(age, sex, postoperative procedure, history of
pulmonary disease (COPD, Lung Ca, asthma,
Pneumonia, Pulmonary TB), onset VAP, outcome of
VAP (death or life), and length of stay.
Data obtained from register books are processed
using computer statistics programs. Univariate
analysis was carried out descriptively by using
frequency distribution tables and calculating
percentages. While the bivariate analysis was carried
out using the chi-square statistical test and the
mean/median difference test. Occurrence risk is
measured using the value of Relative Risk (RR).
The permission of this research was
obtainedfrom the Medical and Health Research
Ethics Unit of the University of Riau Medical
School No. 061 / UN.19.5.1.1.8 / UEPKK / 2019.
3 RESULTS
During the period January-December 2018, there
were 456 ICU patients who were treated more than 2
days (48 hours). 259 of them used mechanical
ventilators, but only 192 patients met the inclusion
criteria. Demographic and clinical characteristics of
the research subjects can be seen in table 1.
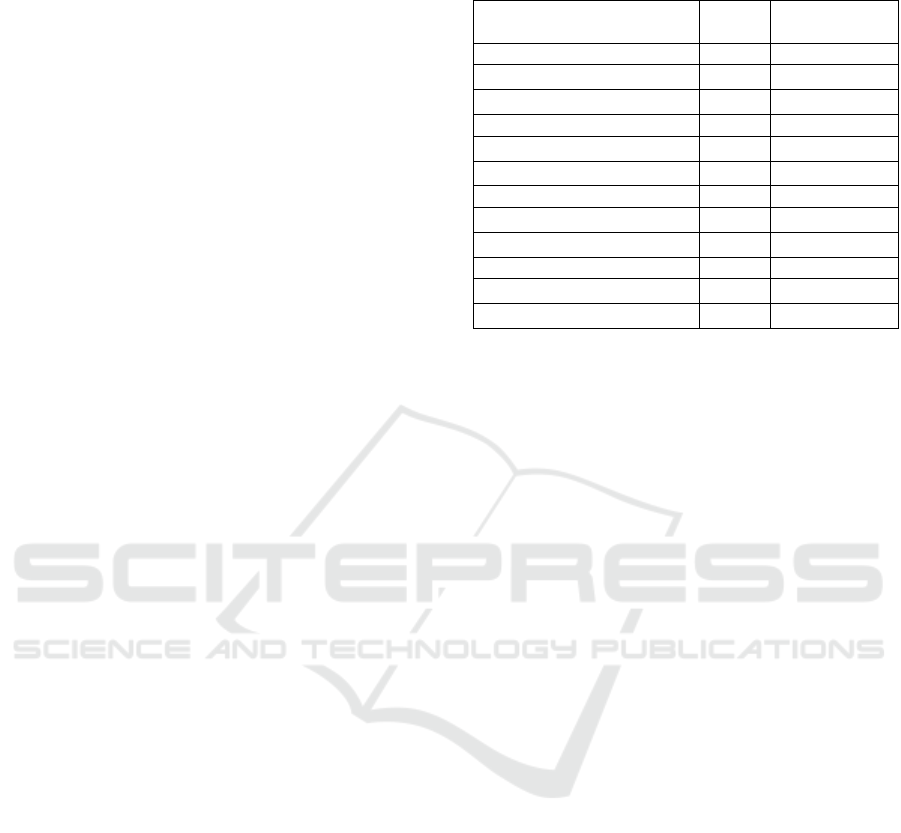
Table 1. Demographic and clinical characteristics of Arifin
Achmad Hospital ICU patients in 2018.
Variable Total Percentage
(%)
Age
≥ 60 years 48 25
< 60 years 144 75
Gender
Man 97 50,5
Woman 95 49,5
Post surgery
Yes 139 72,4
Not 53 27,6
Pulmonary disease history
Yes 11 5,7
Not 181 94,3
In this study, the average age of ICU patients was
52.5 years (19-85) years. Most were found at <60
years of age (75%). The result of this study is the
same as the result of Nency's (2015) study at Arifin
Achmad General Hospital and Salukanan (2017) at
RSUP dr. Hasan Sadikin Bandung, each of whom
found 76.2% and 77.1% of ICU patients aged <60
years.
ICU patients were found slightly more in men
(50.5%) than women (49.5%). The resultof this
study is the same as those of Saragih (2014) at
RSCM, and Susmiarti (2015) in Rumkital, dr.
Ramelan Surabaya, each of which found 53.7%, and
83.3% of ICU patients were male.
139 ICU patients were found after surgery
(72.4%). Similarly, the result of the Ciginskiene
study (2019) at Lithuanian University of Health
Sciences found 38.3% after surgical intervention.
And Turkovic's (2017) research result at the
University Hospital Center in Zagreb, Croatia which
found 72% of ICU patients before tracheotomy and
82% after tracheotomy after neurosurgical. The
resultof the Salukanan study (2017) also found that
40% of ICU patients after post laparotomy for
various reasons, 26.4% after post craniotomy for
various reasons.
In this study, patients who did not have a history
of lung disease were more than those who had a
history of pulmonary disease,181 patients (94.3%).
Similarly, Susanti's (2015) research result at Eka
Hospital Pekanbaru and Abbasinia (2016) in Al-
Zahra Hospital, Isfahan, Iran, each of which found
70% and 46.9% of ICU patients had no history of
pulmonary disease.
Risk Factor Analysis and Outcomes of VAP in ICU Patients at Arifin Achmad General Hospital in 2018: Cohort Retrospective Study
81
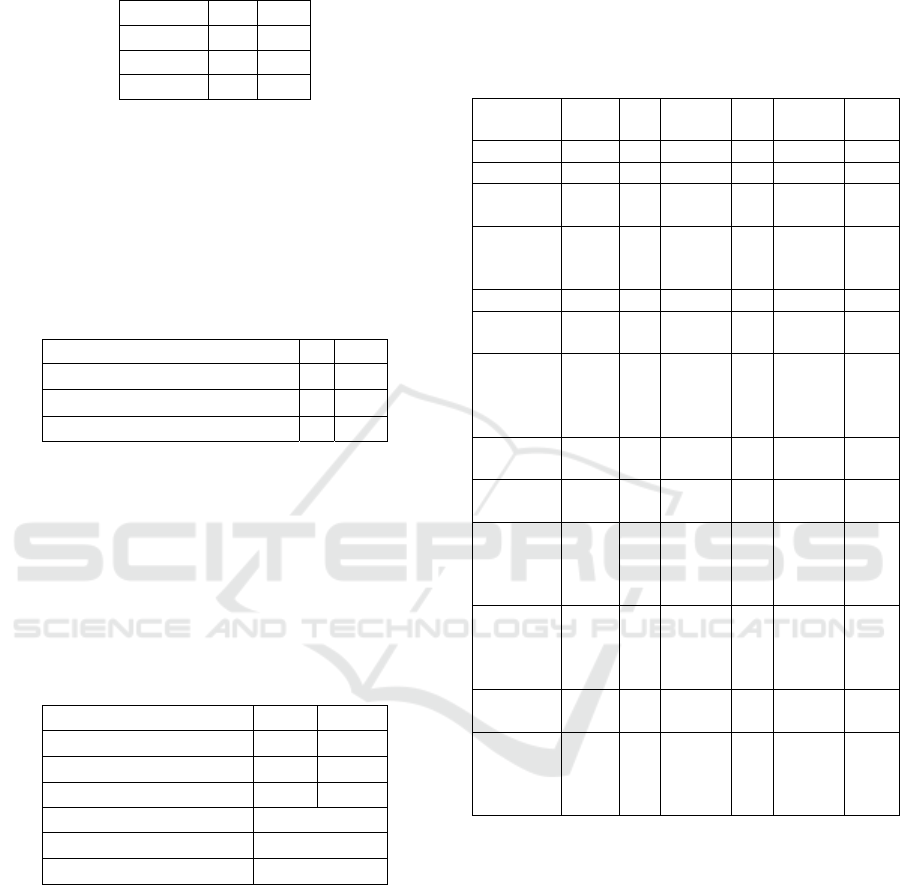
Table 2. The incidence of Ventilator-associated
pneumonia in ICU Arifin Achmad Hospital patients in
2018.
Category N %
VAP 6 3,1
Not VAP 186 96,9
Total 192 100
From table 2, it was found that of 192 patients
admitted to the ICU, there were 6 patients suffered
from VAP (3.1%). Similarly, Saragih's research
result: 27.4%; Nency: 18.58%; Salukanan: 8.5% and
Turkovic: 42%.
Table 3. Onset of The Incidence of Ventilator-Associated
Pneumonia in ICU Patients at Arifin Achmad Hospital in
2018.
Ventilator associated pneumonia N %
≤ 5 days
4 66,6
>5 days
2 33,4
Total 6 100
From table 3, it is known from 6 patients suffered
from VAP, 4 patients experienced it in ≤ 5 days
(66.6%). Similarly, the result of Nency's research:
95.2%; Saragih: 52.2%; Abbasinia (2016) in the ICU
of Al-Zahra Hospital, Isfahan, Iran: 18.8% and
Agustina (2018) in the RSUD Dr. Loekmono Kudus
Hadi: 46.7%.
Table 4. Outputs for Arifin Achmad Hospital ICU patients
in 2018.
Outcome N %
Died
66 34,4
Life
126 65,6
Total 192 100
Length of ICU stay (days) (med,min-max)
VAP
12,5 (7 – 36)
Not VAP
4 (2 – 52)
From table 4, it is known that from 192 patients
admitted to the ICU, more patients lived than died.
(65.6% vs 34.4%). The result of this study is the
same as those of Turkovic (2017) who found that
more patients lived than died. 65% before
tracheotomy and 75% after tracheotomy. However,
it is different from the result of Erbay (2004) in
Pamukkale University Hospital, Denizli, Turkey,
Saragih (2014) and Salukanan (2017), which found
more patients died than living. Each of them was
70.3%, 57.2%, 60%.
The average length of ICU stay for VAP patients
in this study was 12.5 (7-36) days. Similarly, the
research result of Dewi (2014) at Dr. RSUP Kariadi
Semarang found an average of 12.21 ± 9.578 days
and Erbay (2004) 8 days.
Table 5. Bivariate Analysis of VAP Risk Factors.
VAP Not
VAP
P
value
RR
N % n %
Age
≥ 60
years
1 16
,7
47 25
,3
1 0,6
< 60
years
5 83
,3
139 74
,7
(0,0
72-
5)
Genders
Man 3 50 94 50
,5
1 0,97
Woman 3 50 92 49
,5
(0,2
03-
4,73
)
Post
surgery
Yes 4 66
,7
135 72
,6
0,669 0,76
Not 2 33
,3
51 27
,4
(0,1
44-
4,04
)
Pulmon
ary
disease
history
Yes 2 33
,3
9 4,
8
0,04* 8,2
Not 4 66
,7
177 95
,2
(1,6
-
40,1
)
* Pulmonary disease history: COPD, Lung Ca, asthma,
Pneumonia, Pulmonary TB
Table 5 shows that pulmonary disease history is the
only variable that has a significant difference in the
incidence of VAP (p = 0.04). This is similar to the
result of Saragih (2014) and Ibrahim (2000) at
Barnes Jewish Hospital in St. Louis, MO, who found
significant differences in patients with
comorbidities, one of which was Chronic
Obstructive Pulmonary Disease. While other
variables such as age, gender and postoperative
procedures did not show a significant difference
with the incidence of VAP.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
82
Table 6. VAP Outcome Bivariate Analysis.
Died Life p value RR
N %
n % 95% CI
VAP
Yes 3 50 3 50 0,415 1,47
Not 63 33,9 123 66,1 66,1
0,64 –
3,36
Table 6 shows that the proportion of VAP patients
who died and lived was equal to 50% but did not
show a significant difference. Similarly, the results
of a study by Kahlil (2017) which found no
significant difference (p = 0.662) in group I (60%)
and group II (70%) deaths that shared a positive
culture after 48 h of mechanical ventilatio.
Table 7. Differences in duration of care for ICU patients
who experience VAP and not VAP.
VAP Not VAP p value
Length of
ICU stay
(days)
(med,min
-max)
12,5
(7 – 36)
4
(2 – 52)
0,002*
Table 7 shows that the incidence of VAP showed a
significant difference with the length of ICU stay of
patients in the ICU (12.5 days). The results of the
Turkovic (2017) study also found a significant
difference in the length of stay of VAP patients
before and after the tracheotomy, which was 5 (4-9)
days to 11 (10-13) days with p = 0.001. Similarly,
the Rello (2002) study found a greater number of
ICU days (11.7 ± 11.0 days, p <0.001) and longer
hospital length of stay (25.5 ± 22.8 days, p <0.001).
4 DISCUSSION
4.1 Age
In this study, the average age of ICU patients was
52.5 years (19-85) years. Most were found at <60
years of age (75%). The incidence of VAP was also
more common at <60 years of age (83.3%) but was
not significantly associated.
According to Smeltzer and Bare (2013) age is
one of the factors that may affect a person's immune
system which will affect someone’s ability to react
to microorganisms. In addition, an increase in age
will also reduce the production and function of T
and B lymphocytes and thus increase the incidence
of autoimmune diseases. Therefore, the frequency
and intensity of infections will increase in old age. It
can be said that age <60 years or 60 years is equally
at risk of VAP.
4.2 Gender
In this study, the comparison of male and female
patients in ICU are similar (50.5% vs. 49.5%). The
incidence of VAP was also similar in male and
female patients (50% vs 50%) and was not
significantly associated.
Pneumonia infection is more common in men
than women because of the estrogen in women
which can activate nitric oxide synthase-3 (NOS3)
that can increase the activity of macrophages to kill
infectious microbes (Lee, 2008 & Yang et al, 2014)
But according to Sukmadi (2018), patients
admitted to the ICU are not always dominated by
one sex either male or female.
4.3 Post Surgery
In this study, most ICU patients were patients who
were treated after surgery (72.4%). VAP events were
also more common in patients after surgery (66.7%)
but were not significantly associated.
The results of the Cunnion study (1996) found
more incidence of VAP in postoperative patients
than non-surgical patients. Especially in patients
after cardiothoracic surgery and head injury. This is
due to low preoperative albumin levels, prolonged
preoperative care and difficult surgical procedures.
According to Mc Carthy et al (2008) the
installation of the endotracheal tube (ETT) and
decreased consciousness due to anesthesia after
surgery will reduce the patient's ability to swallow
effectively and eliminate coughing which is the
body's natural defense mechanism against
respiratory tract infections. As a result, when
microorganisms enter the lungs, the body's defense
mechanism cannot kill the organism. In addition,
esophageal reflux and aspiration of gastric contents
in ETT patients can also cause endobronchial
colonization and pneumonia.
4.4 Pulmonary Disease History
In this study, 94.3% of ICU patients had not a
history of pulmonary disease (COPD, Lung Ca,
asthma, Pneumonia, Pulmonary TB). 33.3%
developed into VAP but were significantly
associated (p value = 0.04).
Risk Factor Analysis and Outcomes of VAP in ICU Patients at Arifin Achmad General Hospital in 2018: Cohort Retrospective Study
83

Susanti's (2015) study found 30% of patients
with pulmonary disease: COPD, respiratory failure
and Acute Long Oedema (ALO) using a ventilator.
When using a ventilator, the risk of being treated
will be longer compared to patients who do not use a
ventilator, and will increase the risk of suffering
from VAP.
According to Price (2006), one lung disease that
can cause pneumonia is COPD. Patients with COPD
experience epithelial and ciliary damage in their
respiratory tract. Because it is damaged, the
production of goblet cells will increase. Goblet cells
produce sputum which becomes a place for microbes
to develop. This explains why pneumonia infection
often occurs in acutely exacerbated COPD patients
(Sogaard et al, 2016).
Pneumonia in COPD patients will increase
pulmonary function disorders, increase hypoxemia
and infection, resulting in systemic inflammation,
sepsis to organ failure (Sogaard et al, 2016).
Bronchitis and pneumonia are the most common
hospital infections in ICUs Kahlil (2017).
4.5 VAP Incidence
The incidence of VAP in this study was only 3.1%.
According to Agustyn (2007) the incidence of VAP
in patients using mechanical ventilation was 22.8%
and contributed to 86% of nosocomial infections.
Whereas according to Turkovic (2017) the incidence
of VAP in ICU which is reported as 15.5% and
9.3%. Chen et al's research in Taiwan found a VAP
incidence of 3.18 per 1000 days of ventilator use and
ranked second in the ICU.
The results of the Salukanan study (2017) found
an incidence of VAP of 8.5 cases per 1,000 days of
ventilator use. This figure is quite high, but it is still
within tolerance in developing countries. Because
the incidence of VAP in developing countries range
from 1.2 to 8.5 per 1,000 days of ventilator use.
Compare this with developed countries ranging from
0.2 to 4.4 per 1,000 days of ventilator use.
According to Amanullah and Posner (2010),
28% of complications of the patients who use
mechanical ventilation cause VAP. The incidence is
directly proportional to the duration of use of
mechanical ventilation. Estimated incidence of 3%
per day for the first 5 days, 2% per day for 6-10
days, and 1% per day after 10 days.
4.6 VAP Onset
The onset of VAP≤ 5 days in this study was 66.6%.
According to Ibrahim (2000), in general, early onset
VAP (≤ 5 days) has a better prognosis because
germs are still sensitive to antibiotics. Conversely,
late-onset VAP (> 5 days) has a worse prognosis
because there has been colonization of Multi-Drug
Resistant (MDR) bacteria so that the mortality rate
will increase (Torres, 2004 & Nency, 2015)
4.7 Outcome
4.7.1 Died/Life
The number of ICU patients who died in this study
was less than those living (34.4% vs. 65.6%).
However, the number of VAP patients who died and
lived was equal (50% vs. 50%), although it was not
significantly related.
Some studies have found a relationship between
death and VAP. These include the Turkovic (2017)
case-control study in 85 VAP patients and 85 non
VAP patients at the University Hospital Center in
Zagreb, Croatia. He found 40% of deaths in VAP
patients and 38.8% in non VAP patients. There were
no significant differences between the two
classifications.
The Fagon et al. Study, in 1.118 patients using
mechanical ventilation, found an association
between VAP and a one-and-a-half increase in the
risk of death (odds ratio, 1.51; 95% CI, 1.11-2.03)
(Safdar, 2005) .
According to Erbay (2004) the main cause of
death from hospital-acquired infections is
Nosocomial Pneumonia (NP). 25% of nosocomial
infections in hospitals are distributed by patients
admitted to the ICU. The cause of high nosocomial
infections in the ICU is due to the patient’s main
diagnosis, the severity of the disease, the length of
treatment and the invasive device used by the
patient. The estimated prevalence of NP within the
hospital settings ranges from 10% to 65%, with case
fatality rates which is greater than 25% in most
studies.
According to Saragih (2014) the high mortality
rate of VAP in Indonesia besides due to improper
use of antibiotics, also caused by the management is
not optimal, which is caused by limited funds (66%
of the research subjects have no health insurance).
4.7.2 Length of ICU Stay (days)
The average length of stay for VAP patients in this
study was 12.5 (7-36) days. 3 times longer than the
treatment of patients who were not diagnosed with
VAP. The results of the analysis showed a
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
84

significant difference between the length of stay
with the incidence of VAP (p-value: 0.002).
The results of the study by Kahlil (2017) found
that the length of stay in the ICU was around 7-54
days. According to the study, VAP is an infection in
a hospital that has an impact on the length of stay,
increased hospital costs and a greater risk of death.
Turkovic (2017) also found that VAP patients
were treated longer in the ICU than patients without
VAP. Several studies report that patients with VAP
have increased the length of stay and hospital costs
(Safdar, 2005). Warren et al. (2003) reported that the
cost of hospitalization for patients with VAP was
significantly higher than for patients without VAP ($
70,568 vs. $ 21,620). Rello (2002) found the average
hospital bill for VAP patients to be $ 104,983 ± $
91,080. Which is significantly bigger.
In addition Rello (2002) also found that patients
with VAP had a significantly longer hospital length
of stay (25.5 ± 22.8 days, p <0.001) and a greater
number of ICU days (11.7 ± 11.0 days, p <0.001).
The number of days of treatment for patients with
VAP is longer than for patients without VAP. 9.6
days longer due to mechanical ventilation, 6.1 days
longer in the ICU, and 11.5 days longer in the
hospital. And the average hospital bill cost of VAP
patients is $ 40,000, which is significantly higher
than patients without VAP.
5 CONCLUSION
VAP study was as much as 3.1%. The onset of VAP
found within 5 days 66.6%, it is expected that the
prognosis will be better. This study showed that risk
factors for pulmonary disease history were only
33.3% but were significantly associated with the
incidence of VAP (p-value = 0.04, RR = 8.2 (1.6-
40.1)). VAP occurrencewere significantly related
with length of stay for patients in the ICU (p-value =
0.002), with a median of 12.5 (7-36) days.
From this study we concluded that VAP needs
more attention to prevent its occurrence. As once
diagnosed, it usually increases ICUs mortality rates
and its potentially substantial attributable moretality
rates.
ACKNOWLEDGMENTS
Appreciation goes to Arifin Achmad General
Hospital and staff of the ICU and infection
prevention and control committee who helped us in
conducting this study.
REFERENCES
Abbasinia M, Bahrami N, Bakhtiari S, Yazdannik A,
Babaii A. 2016. The Effect of a Designed Respiratory
Care Program on the Incidence of Ventilator-
Associated Pneumonia: A Clinical Trial. Journal of
Caring Sciences, 5(2) : 161-167.
Augustyn, B. 2007. Ventilator-associated pneumonia risk
factors and prevention. Critical Care Nurse, 27(4) : 32-
39.
Ciginskien A, Dambrauskien A, Rello J and Adukauskien
D. 2019. Ventilator-Associated Pneumonia due to
Drug-Resistant Acinetobacter baumannii: Risk Factors
and Mortality Relation with Resistance Profiles, and
Independent Predictors of In-Hospital Mortality.
Medicina, 55, 49 : 1-13.
Dewi H, Harahap MS. 2014. Hubungan Usia Penderita
Ventilator Associated Pneumonia Dengan Lama
Rawat Inap Di ICU RSUP Dr. Kariadi Semarang.
Jurnal Media Medika Muda : 1-14.
Erbay RH, Yalcin AN, Zencir M, Serin S, Atalay H. 2004.
Costs and risk factors for ventilator-associated
pneumonia in a Turkish University Hospital's
Intensive Care Unit: A case-control study. BMC
Pulmonary Medicine 4 : 1-7.
Gillespie, R., 2009. Prevention and Management of
Ventilator-Associated Pneumonia – The Care Bundle
Approach, (Online), available from
(http://ajol.info/index.php., 15th march 2019).
Ibrahim EH, Ward S, Sherman G, Kollef MH. 2000. A
comparative anlysis of patients with early-oset vs late-
onset nosocomial pneumonia in the ICU setting. Chest
117 : 1434-42.
Kahlil, NH , Khalil AT , Abdelaal DE. 2017. Comparison
study between bacteriological aetiology and outcome
of VAT & VAP. Egyptian Journal of chest Diseases
and Tuberculosis 66 : 169-174.
Hunter JD. 2006. Ventilator associated pneumonia.
Postgrad Med J 82 (965) : 172-8.
McCarthy, S.O, et al., 2008. Ventilator Associated
Pneumonia Bundled Strategies; An Evidence-Based
Practice. Worldview on Evidence-Based Nursing
fourth quarter : 193–204.
Nency C, Irawan D, Andrini F. 2015. Gambaran Kejadian
Ventilator-Associated Pneumonia Pada Pasien Yang
Dirawat Di ICU Dan CVCU RSUD Arifin Achmad
Periode Januari 2013 S/D Agustus 2014. JOM FK
Volume 2 No. 2 Oktober 2015 : 1-9.
Patricia, G., Dorrie, F., & Barbara, M. 2012. Keperawatan
kritis pendekatan asuhan holistik: Jakarta: EGC.
Price, A. 2006. Patofisiologi konsep kilinis proses-proses
penyakit. Jakarta: EGC.
Rello J, et al. 2002. VAP Outcomes Scientific Advisory
Group. Epidemiology and outcomes of ventilator-
Risk Factor Analysis and Outcomes of VAP in ICU Patients at Arifin Achmad General Hospital in 2018: Cohort Retrospective Study
85

associated pneumonia in a large US database. Chest
122 : 2115-2121.
Safdar N, Dezfulian C, Collard HR, Saint S. 2005. Clinical
And Economic Consequences Of Ventilator-
Associated Pneumonia: A Systematic Review. Crit
Care Med 2005 Vol. 33, No. 10 : 2184-2193.
Saragih RJ, Amin Z, Soedono R, Pitoyo CW, Rumende
CM. 2014. Prediktor mortalitas pasien dengan
ventilator-associated pneumonia di RS Cipto
Mengunkusumo. Departemen Anestesiologi dan
Perawatan Intensif FK UI: Vol.2 No.2.
Salukanan RT, Zulfariansyah A, Sitanggang RH. 2018.
Pola Pneumonia Nosokomial di Unit Perawatan
Intensif Rumah Sakit Umum Pusat Dr. Hasan Sadikin
Bandung Periode Januari–Desember 2017. JAP,
Volume 6 Nomor 2, Agustus 2018 : 126-136.
Smeltzer, Bare SC, Brenda. G, 2013. Buku Ajar
Keperawatan Medikal Bedah Brunner & Suddarth.
Ed.8. Vol. 3. Jakarta: EGC :1698 – 1700.
Sukmadi A, Pujiastuti SE, Santjaka A, Supriyadi. 2018.
Effectiveness Of Suction Above Cuff Endotracheal
Tube In Preventing Ventilator Associated Pneumonia
In Critical Patients In Intensive Care Unit. Belitung
Nursing Journal. 2018 August; 4 (4) : 380-389.
Susmiarti D, Harmayetty, Dewi YS. 2015. Intervensi Vap
Bundle Dalam Pencegahan Ventilator Associated
Pneumonia (Vap) Pada Pasien Dengan Ventilasi
Mekanis (The Incidence of VAP after VAP Bundle
Intervention Among Patients with Mechanical
Ventilation). Jurnal Ners Vol. 10 No. 1 April 2015 :
138–146.
Susanti E , Utomo W , Dewi YI. 2004. Identifikasi Faktor
Resiko Kejadian Infeksi Nosokomial Pneumonia Pada
Pasien Yang Terpasang Ventilator Di Ruang Intensive
Care. JOM Vol 2 No 1, Februari 2015 590 : 590-599.
Torres A, Ewig S. 2004. Diagnosing ventilator associated
pneumonia. N Engl J Med 2004. 350 : 433-522.
Turković TM, Obraz M, Glogoški MZ, Juranić I, Bodulica
B, Kovačić J. 2017. Incidence, Etiology And Outcome
Of Ventilator-Associated Pneumonia In Patients With
Percutaneous Tracheotomy. Acta Clin Croat, Vol. 56,
No.1, 2017: 99-109.
Warren DK, Shukla SJ, Olsen MA, Kollef MH,
Hollenbeak CS, Cox MJ, Cohen MM, Fraser VJ. 2003.
Outcome and attributable cost of ventilator-associated
pneumonia among intensive care unit patients in a
suburban medical center. Crit Care Med 2003,
31:1312-1317.
Wiryana, M. 2007. Ventilator Associated Pneumonia. J
Peny Dalam, Volume 8 Nomor 3 Bulan September;
2007 : 254-268.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
86
