
Combination of Trunk Mobilization and Neuro Development
Treatment against Spasticity Reduction of Spastic Type Cerebral
Palsy
Siti Sarah Bintang*, Miftahul Zannah, Isidorus Jehaman, Elsaria Br Sembiring, Raynald Ignasius
Ginting and Sabirin Berampu
*Faculty of Nursing and Physiotherapy, Institut Kesehatan Medistra Lubuk Pakam, Indonesia
Keywords: Cerebral Palsy, Spastisitas, Mobilisasi Trunk, Neuro Development Treatment
Abstract: Spastic cerebral palsy is a type of brain damage that occurs in the extreme part of the pyramids that results in
an increase in reflexes that make muscle tone higher than normal. This study aims to look at the effect of a
combination of Trunk Mobilization and Neuro Development Treatment on reducing spasticity in spastic type
cerebral palsy children. The research design used was one group pre and post test design. Test Results for the
results of reducing spasticity in cerebral palsy children before and after the intervention of Trunk Mobilization
and Neuro Development Treatment, it can be seen that the value of p = 0.157 which means greater than 0.05
(p> 0.05) so that the null hypothesis (Ho) accepted and the alternative hypothesis (Ha) was rejected. So the
conclusion with the acceptance of Ho means there is no effect of a combination of Trunk Mobilization and
Neuro Development Treatment to reduce spasticity in children with cerebral palsy after intervention.
1 INTRODUCTION
Cerebral palsy or abbreviated (CP) is a disability that
was first raised by William Little in the 1840s. This
condition is a diagnostic and therapeutic challenge
which is quite large (Bajraszewski, 2014). There are
mild degrees with minimal disabilities up to severe
degrees. Disability that occurs for a lifetime, will
generally be the cause of autism and mental
retardation which causes difficulties for the impact on
their individuals and families (Myoung and MPH,
2017).
Cerebral palsy is a disorder of motion and attitude.
This is defined as a non progressive disorder of
posture, motor disturbances and secondary disorders
that occur due to lesions or anomalies that occur in
the brain that arise in the early stages of development.
Primary lesions or static injuries will affect the
growth and development of plasticity and maturity of
the central nervous system (Myoung and MPH,
2017). Cerebral palsy occurs worldwide 2-2.5/1000
births. One cause is trauma at birth, and the progress
of neonatal management has not been able to show a
decrease in the incidence of CP patients (Ryan and
Sandra, 2011).
The neurologic impairment is nonprogressive,
although secondary disability can occur.
Characteristics of cerebral palsy change with
developmental stages, especially in the first few years
of life. This impairment and resultant disability are
both permanent (Bosanquet, 2013).
The prevalence of people with Cerebral Palsy at
birth is based on research data from health care
centers in the United States from mild to severe
ranging from 1.5 to 2.5 per 1000 live births. Research
data on school-age children, the prevalence of
cerebral palsy found 1.2 - 2.5 children per 1,000
population. At least 5,000 new cases of cerebral palsy
occur each year. From these cases 10% to 15% of
cerebral palsy found a brain disorder that is usually
caused by infection or trauma after the first month of
life (Surakarta,2013).
The incidence of cerebral palsy patients in
Indonesia based on data from the Ministry of Health
in 2011 is estimated to be around 1 - 5 per 1,000 live
births and the number of people with disabilities is
around 7-10% of Indonesia's population. More men
than women. Generally found in the first child. The
incidence rate is higher in babies born prematurely,
twin births and mothers who are over 40 years old.
Almost half this disability is experienced in children
Bintang, S., Zannah, M., Jehaman, I., Sembiring, E., Ginting, R. and Berampu, S.
Combination of Trunk Mobilization and Neuro Development Treatment against Spasticity Reduction of Spastic Type Cerebral Palsy.
DOI: 10.5220/0009840304830490
In Proceedings of the International Conference on Health Informatics and Medical Application Technology (ICHIMAT 2019), pages 483-490
ISBN: 978-989-758-460-2
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
483
born prematurely and children born normal (Depkes,
2011).
Pathogenesis of CP occurs from the first
gestational age to 24 weeks. Cortical neurogenesis
occurs characterized by poliferation, migration, and
neuronal processes of neuron precursor cells (Dutt,
2015). Genetic deficits or disorders such as viruses or
toxicity result in malformations such as issencephaly
or agyria-pachygria, nodular heterotopias,
polymicrogyria, schizencephaly, and cortical
dysplasia. Growth and differentiation events (axonal
and dendritic growth, synapse formation and
myelination) as well as the process of neural
apoptosis, neuron regression, redundant synapse
elimination. Environmental factors also affect such as
hypoxia ischemia. In addition, the process of forming
an immature brain structure will change a series of
developmental events, therefore CP is the result of
destructive and developmental mechanisms
(Stephaniie,2013).
The etiology of CP is very diverse and
multifactorial the causes are congenital, genetic,
inflammatory, contagious, anoxic, traumatic and
metabolic. Injury tothe brain can occur in the
prenatal, or postnatal period of CP is more common
in children born very premature or full term. Even
though term babies have a relatively low absolute
risk, the term birth represents the majority of all
births, like as well as about half of all child births with
cerebral palsy. Prenatal risk factors include
intrauterine infection, teratogenic exposure, placental
complications, multiple birth, and motherly
conditions like mentality retardation, seizures, or
hyperthyroidism. The incident CP is higher among
twins and triplets than singles bleeding, seizures,
hypoglycemia, hyperbilirubinemia, and significant
birth asphyxia. Perinatal arterial ischemia stroke has
been identified as another possible cause which
causes CP hemiplegia in many babies (Sankar, 2005).
To aid in confirming the diagnosis and ruling out
neoplastic or progressive causes for motor disability
such as metabolic and neurodegenerative disorders,
magnetic resonance imaging (MRI) is usually
indicated. The imaging can usually wait until a child
can undergo the study without sedation or done in
conjunction with another procedure. Other diagnostic
testing may include cultures, immune status,
metabolic screening, karyotyping, genetic probes or
confirmatory tests for other specific disorders
(Bosanquet, 2013).
Impaired oxygen supply to the fetus and brain
Asphyxia is classically considered as the main cause
of explaining CP later. But clinically defined birth
injury or birth asphyxia accounts for a small
proportion of CP cases (Ferluga, 2013). CP is rarely
due to brain malformations due to a unique genetic
deficit or perinatal damage that is obtained due to a
unique acute asphyxic event. Generally CP, the
causative factors do not act separately, but in synergy
to create interference (Stephaniie,2013).
CP is classified into topographic-based subtypes,
diplegia, hemiplegia, or extrapyramidic disorders.
This classification arises in various areas of the
nervous system that develop during the process of
fetal development in the womb, during labor and after
birth during the first 2 years of life. Gestational age
also influences the development of brain structure and
the type of disability associated with CP (Ryan and
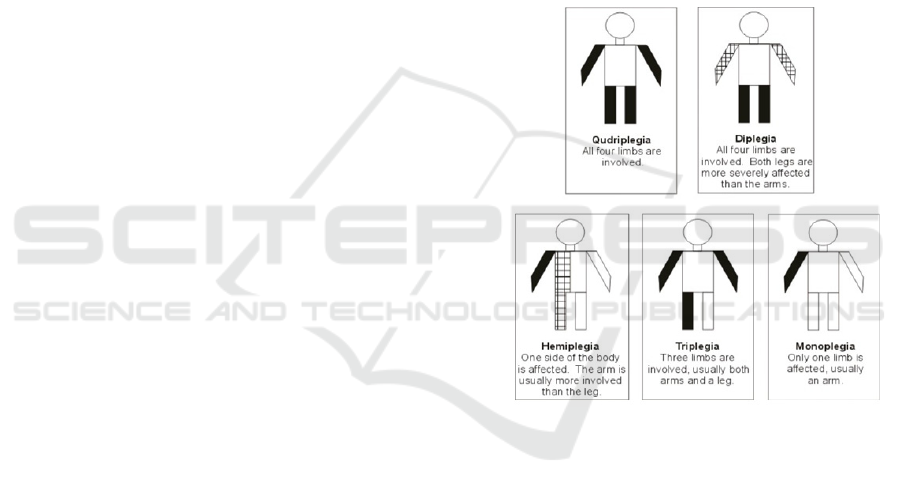
Sandra, 2011). Topographic of Cerebral Palsy can be
seen in the picture below in Figure 1.
Figure 1: Topographic of Cerebral Palsy.
There are three types of cerebral palsy that can be
distinguished by their symptoms and management
approaches. The types of CP men are Spastic, Ataxic
and Athetoid brain paralysis (Hartono, 2004). Spastic
CP type is CP that has spasms characterized by
unique muscle tightness the patient has muscle
flexibility. This type of CP occurs in at least 70% of
all CP cases in the world. In the case of CP seizures,
this disorder can be more easily managed compared
to other types since treatment through treatment can
be taken in a number of neurological and orthopedic
approaches. Muscle spasticity causes other symptoms
of muscle stress that may include tendinitis and
arthritis in individuals aged 20-30 years. This type of
CP can be managed using occupational and physical
therapy where it can strengthen, stretch, exercise and
the other. Physical activity is used to manage daily
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
484
disruptions. The disorder can also be overcome using
drugs that eliminate flexibility by killing the nerves
that cause the disorder (Kumar and Parveen, 2018).
Pain is a common problem in the brains of
children of all ages. Many children are very patient
and don't need to ask about pain. That pai most often
felt due to musculoskeletal disorders, spasms and
spasticity or digestive problems like as reflux and
constipation. It is important for children with cerebral
palsy to look for and eliminate the causes of pain and
to treat pain passionately without complaining.
Muscle cramps due to fatigue (Bosanquet, 2013).
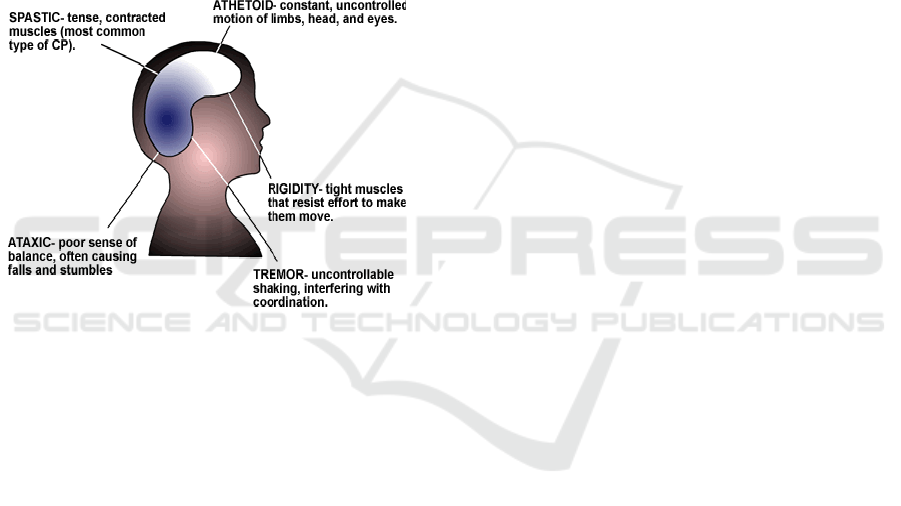
Type of Cerebral Palsy can be seen in the picture
below in Figure 2.
Figure 2: Type of Cerebral Palsy
Spasticity is an increase in stretch reflexes and tendon
reflexes that originate from excessive excitability of
stretch reflexes in limb abnormalities. Postural tone
abnormalities will result in impaired coordination and
poor balance. So that spasticity becomes a problem
solving that must be considered. Rhines and Magoun
said the emergence of spasticity is a result of an
imbalance between alpha and gamma motor neurons
which is a consequence of the imbalance between the
facilitation center and the inhibition center (Susanto,
2014).
The physiotherapy approach that is commonly
used for handling disorders in Cerebral Palsy children
such as Neurostructure, Brain gym, (Neuro
Development Treatment) NDT, Trunk mobilization.
In this study the methods used are two of the above
interventions and then combined to reduce spasticity
in children with Cerebral Palsy.
Trunk mobilization is a passive stretching
technique that extends soft tissue. Passive stretching
is expected to provide a relaxing effect on spastic
muscle groups, increase postural mobility and control
abnormal movements that arise, thereby reducing
stiffness or spasticity in the trunk region towards
lower extremity (Kisner, 2013).
Trunk mobilization is a passive stretching
technique that extends soft tissue. Passive stretching
is expected to provide a relaxing effect on spastic
muscle groups, increase postural mobility and control
abnormal movements that arise, thereby reducing
stiffness or spasticity in the trunk region towards
lower extremity (Kisner, 2013).
NDT (Neuro Development Treatment) or Bobath
Method. The concept of this method is to affect
muscle tone and increase postural balance. This
method is able to treat motor control disorders of
cerebral palsy spectrum (Kavlak et al., 2018).
NDT is
a training method to stimulate the response of
neuromuscular mechanisms through proprioceptor
stimulation. NDT (Neuro Development Treatment)
techniques include: inhibition of spasticity,
facilitation and stimulation to improve abnormal
movement patterns, normalizing tone and optimizing
postural control functions. Before implementing the
NDT (Neuro Development Treatment) method, it is
first performed proper examination, determination of
physiotherapy diagnoses and plan of therapeutic
program for sufferers of spastic type cerebral palsy
(Surakarta,2013).
In a state of normal activity needed background
movement which is normal and functional skills.
Normal Postural Reflexology Mechanisms are
dynamic response in every answer activity changes.
The reactions are Encourage NPRM: Righting
reaction Consists of: labyrintine righting, neck
righting, body on body righting reaction, body on
head righting reaction and optical righting reaction.
Equilibrium reaction and Protective reaction.
The nature of the Trunk Mobilization method and
NDT (Neuro Development Treatment) is suppressing
pathological abnormal / postural reflexes which
causes normal movements to be inhibited and
stimulation in the form of touch, exercises shown to
stimulate neurons in children in normal growth and
development. But the process requires quite a long
time. Early and intensive treatment will provide
optimal results, because it will continuously improve
abnormal patterns in children (Surakarta,2013).
Ashworth scale is a degree or scale used to
measure the level of muscle spasticity / tone. The
Ashworth scale is one of the physiotherapy measuring
devices, part of the Bobath concept. Initially used to
see the reaction of antispastic drugs in
multipleschelosis. In 1987 developed by Bohannon
and Smith, so this measurement was used to measure
Combination of Trunk Mobilization and Neuro Development Treatment against Spasticity Reduction of Spastic Type Cerebral Palsy
485
the spastic value of the problem of the central nervous
system (Surakarta,2013).
2 RESEARCH METHOD
The research was carried out in the Physiotherapy
room at Deli Serdang Lubuk Pakam Distric Hospital
right on Thamrin street number 1 Lubuk Pakam for
1 month starting on june 6, 2016 until june 30, 2016.
The sample of study consisted of 12 people obtained
from the calculation of the Pocock formula (Pocock,
2014).
Spasticity measurements are carried out using
the Asworth scale. The Asworth scale has been
widely used in the population of children with
cerebral palsy. Asworth scale is an instrument used
to assess the intensity of spasticity. Asworth scale
value:
Value 0: There is no increase in tone.
Value 1: An increase in muscle tone is marked
by the feeling of minimal resistance at the end of
ROM when the joint is moved flexion and
extension.
Value 2: There is a slight increase in tone
marked by the cessation of movement and the
appearance of a minimum resistance along the
rest of theROM.
Value 3: There is an increase in muscle tone
more pronounced along most of the ROM.
Explain to sufferers that right angle means no
pain, middle means moderate pain and left angle
means very painful (front VAS).
Value 4: Increased tone is very real, passive
motion is difficult tomove.
Value 5: Stiff joints and extremities for flexion
and extension
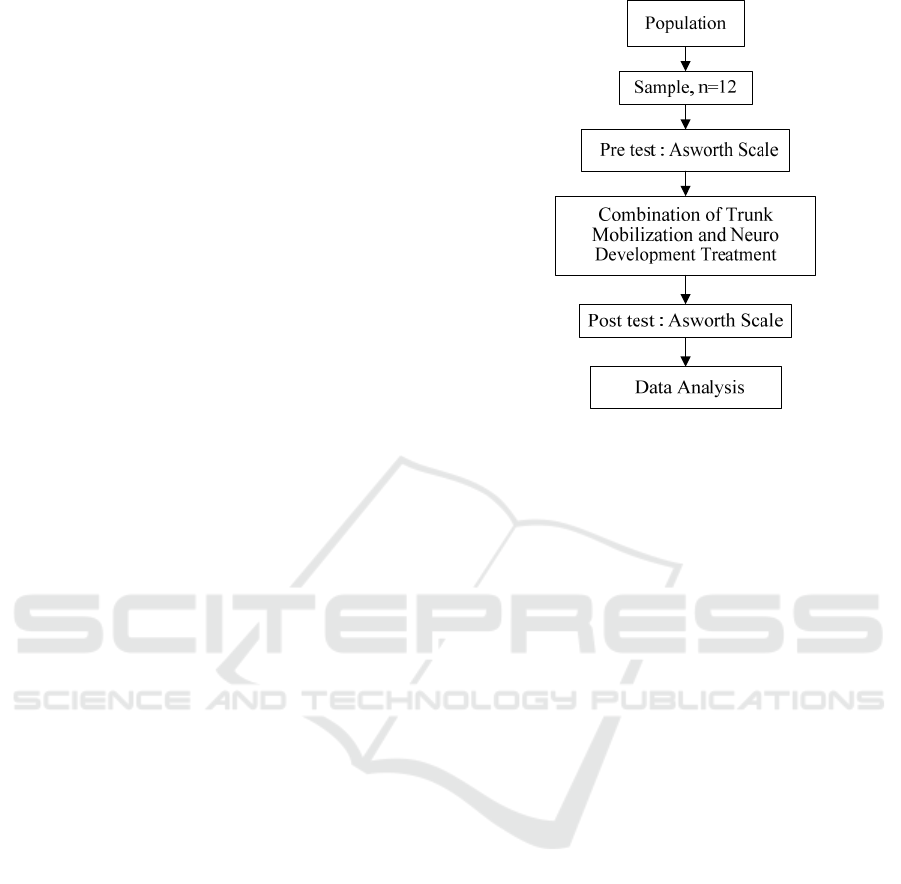
Research flow can be seen in the picture below in
Figure 3.
Figure 3: Research flow.
Trunk mobilization is a passive stretching technique
that extends soft tissue. Passive stretching is expected
to provide a relaxing effect on spastic muscle groups,
increase postural mobility and control abnormal
movements that arise, thereby reducing stiffness or
spasticity in the trunk region towards lower extremity
(Kisner and Colby,2007).
The mechanism of exercise in trunk mobilization
is to improve the co-contraction of trunk muscles and
to gain flexibility from the trunk. At the end of the
passive movement can be accompanied by stretching
(stretching soft tissue) and elongation (trunk
lengthening towards the top) (Humaira, 2014).
Extending carried out passively will be able to
lengthen the soft tissue so that it decreases stiffness or
spasticity. Passive stretching is expected to provide a
relaxing effect on spastic muscle groups.
Neuro Development Treatment was developed by
Dr. Kr Bobath and Mrs. Berta 1997. This method is
specifically used to deal with central nervous
disorders in infants and children. The main principle
that underlies this method is the normalization of
muscle tone, facilitating normal movement patterns in
daily activities.
The mechanism of neuro development treatment
(NDT) is the inhibition of abnormal reflex activity
patterns and the facilitation of normal motor patterns.
Physiologically spasticity results from excess
abnormal tonic reflexes due to UMN lesions
(Richard, 2008). The provision of continuous therapy
provides direct inhibition of spastic muscles. By
doing the inhibition technique, it will stretch both the
extrafusal muscle and the muscle spindle of the
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
486

muscle. Then the muscle spindle responds by sending
a series of spindle impulses to the spinal cord.
Afferent fibers in the dorsal radix that carry
impulses form synapses with motoneuron which are
then excited and cause muscle contraction. This
occurs when afferent fibers from the spindle muscle
give a collateral branch to a group of intermediary
neurons in the grisea substrate (Koman, 2014). These
neurons are inhibitors and send their axons to the
motor neurons that innervate the antagonistic
muscles. Explanation of the example above illustrates
the muscle spindle by means of afferent impulses
monosympathetically activating motorneuron which
invests extrafusal muscle causing contraction of the
muscle and causes relaxation of the antagonist, which
means reduced spasticity (Pariera,2011).
3 RESULT AND DISCUSSION
3.1 Characteristics of Respondents
The study was conducted on subjects, namely
children with a diagnosis of Cerebral palsy in Lubuk
Pakam District Hospital and from those selected as a
whole (total sampling) aged between 1-6 years. From
the results of the study can be described as the
following analysis.
The gender of men is 6 people or 50%, women are
6 people or 50%. While the respondents based on
gender the majority of women are 9 people or 75% of
the total 12 respondents from the two intervention
groups. Characteristics of Respondents by sex can be
seen the below in able 1.
Table 1: Characteristics of Respondents by sex.
Sex n Persentation (%)
Male 6 50 %
Female 6 50 %
Based on the table below it appears that the
majority of research subjects at the RSUD are ages 1-
2, as many as 4 people with 33.3 presentations, then
at the age of 3-4 years, as many as 7 people with a
percentage of 58.3 and children aged 5-6 years, as
many as 1 person with a percentage of 8.3, the mean
results obtained are 1.75 and SD are 0,622.
Characteristics of Respondents by age can be seen the
below in Table 2.
Table 2: Characteristics of Respondents by age
Age n Persentation
(%)
1-2 th 4 30 %
3-4 th 7 50 %
5-6 th 1 7 %
Based on the table above, it appears that most of the
research subjects at the Lubuk Pakam Regional
Hospital based on body weight, namely 10 kg body
weight by 3 people with a percentage of 25.0 and then
followed by each different body weight ie 8 kg body
weight by 1 person with a percentage of 8 , 3%, 9 kg
body weight 2 people with a percentage of 16.7%, 12
kg body weight 2 people with a percentage of 16.7,
body weight 16 kg 2 people with a percentage of
16.7%, body weight 20 kg 1 person with a percentage
of 8.3%, 14 kg body weight of 1 person with a
percentage of 8.3 with a mean of 12.17 and an
elementary school of 3.639. Characteristics of
Respondents based on body weight can be seen in
Table 3.
Table 3: Characteristics of Respondents based on body
weight.
Body Weight n Persentation
(%)
8 1 8 %
9 2 16 %
10 3 25 %
12 2 16 %
14 1 8 %
16 2 16 %
20 1 8 %
3.2 Spasticity Measurement Results
Based on the table above, it appears that the research
subjects at Deli Serdang Lubuk Pakam Hospital with
their severity based on the Asworth scale obtained the
results that with a spasticity (pre test) the maximum
value is 5 while the minimum value is 2 with a Mean
of 2.58 and a Standard Deviation (SD) 0.996, while
after the intervention (post test) it is known that the
value of spasticity in cerebral palsy children with a
maximum value of 4 while the minimum value of 2
with a mean of 2.42 and a standard deviation (SD)
0,793. Spasticity measurement results can be seen in
Table 4.
Combination of Trunk Mobilization and Neuro Development Treatment against Spasticity Reduction of Spastic Type Cerebral Palsy
487

Table 4: Asworth scale values before and after the
intervention
Asworth scale
n
Before After
1
4
4
2
2
5
3
2
3
4
3
4
5
2
2
6
2
2
7
2
2
8
5
3
9
2
2
10
3
3
11
2
3
12
2
3
Mean 2,58 2,42
3.3 The Effect of Trunk Mobilization
and Neuro Development Treatment
on Decreasing Spasticity
The results of data processing using paired t- test,
before and after the administration of the
intervention. the results of data analysis found that
there was no effect of the intervention so that the
intervention did not affect the reduction of spasticity
in children with cerebral palsy with indicated p value
= 0.157 which means p value greater than 0,05
(p>0,05). Results can be seen in the Table 5.
Table 5: Pre test and Post Test
Group n x
̄
± SD
p
*
Pre-tes
t
12 2,58 ± 0,28 0,15
Pos
t
-tes
t
12 2,42 ± 0,22
This shows that the results obtained are not in
accordance with the theory and purpose of the
combination method of Trunk Mobilization and NDT
which have a role to reduce Spasticity. In this study,
researchers have not yet gotten the results from
providing a combination of Trunk Mobilization and
NDT in reducing spasticity in spastic-type Cerebral
palsy children, for their spasticity the patient did not
change due to the nature of the Trunk Mobilization
and NDT (Neuro Development Treatment) methods.
The mechanism of intervention is suppressing
pathological abnormal / postural reflexes which
causes normal movements to be inhibited and
stimulation in the form of touch, exercises shown to
stimulate neurons in children in normal growth and
development (Kisner, 2013). But the process requires
quite a long time. Early and intensive treatment will
provide optimal results, because it will continuously
improve abnormal patterns in children (Pickles, Altun
and Yurdalan, 2016).
In a study by Tri Sarjono Waluyo, statistical tests
showed that there was an effect of trunk mobilization
on decreasing spasticity in spastic cerebral palsy in
sample 12 according to the largest age group between
ages 3-4 years with results (p = 0.046)) (Waluyo,
2010). Research by Bar-Haim et al., 2006 with the
title "comparison of efficacy of adeli suit and
neurodevelopment mental treatment in children with
cerebral palsy" influence on reducing spasticity in
Spastic type Cerebral Palsy children, with a sample of
12 cerebral palsy children (9 boys and 3 girls) with an
age range of 5-13 years, for brackets of 4 weeks or 1
month (2 hours per day, 5 days a week, in 20 sessions)
with significant results p <0.05. The researchers'
assumption that the giving of an intervention needs to
be given attention to the accuracy of the intervention
(Stevness,2009).
4 CONCLUSION
Based on the results of the statistical tests and the
discussion above, it can be concluded that there is no
effect of reducing spasticity onspastic-type Cerebral
Palsy children in the administration of a combination
method of the combination of Trunk Mobilization and
NDT.
5 SUGGESTION
To find out whether the therapy is successful or not,
as a physiotherapist should use a measuring tool to
measure the results before and after being given an
intervention so that it always gets an evaluation.
Adjusting the patient's exact position when doing
activities or at rest against the spasticity pattern so
that the spastic muscles can elongate and can prevent
contractures. The length of time given.
ACKNOWLEDGEMENTS
Researchers thank all those who have helped during
the research process and all the staff of the Institute
for Health Medistra Lubuk Pakam.
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
488

REFERENCES
Acar, G., Altun, G. P. and Yurdalan, S. 2016 ‘Efficacy of
neurodevelopmental treatment combined with the
Nintendo ® Wii in patients with cerebral palsy’, pp.
774–780.
Bajraszewski E, et al. 2008; Cerebral palsy an information
guide for parents. The Royal Children’s Hospital,
Melbourne.
Bosanquet M, Copeland L, Ware R, et al. A systematic
review of tests to predict cerebral palsy in young
children. Dev Med Child Neurol. 2013;55:418-426.
Dutt R,et al.2015; Sleep and Children with Cerebral Palsy:
A review of current evidence and environmental non-
pharmacological intervention. Children, 2, 78-88;
doi:10.3390/children2010078.
Ferluga, Elizabeth.D., MD., Archer, Kristin R., PhD., DPT.,
Sathe, Nila A., MA., MLIS., Krishnaswami, S.,
MBBS., MPH., Klint, A., RD., Lindegren Mary L.,
MD., Melissa L., McPheeters., PhD., MPH. 2013.
Interventions For Feeding And Nutrition Cerebral Palsy
Type Spastic.
Hartono, Bambang.2004. Perbedaan faktor resiko dan
berbagai fungsi dasar antara Cerebral Palsy tipe
hemiplegic dengan tipe diplagia spatica. Media medica
Indonesia.
Humaira, 2014. Pelatihan Fisioterapis Anak. Semarang.
Undip.
Kavlak, E. et al. (2018) ‘Effectiveness of Bobath therapy
on balance in cerebral palsy Bobath terapisinin serebral
palside denge üzerindeki etkisi’, 43(4), pp. 975–981.
doi:10.17826/cumj.375565
Kisner, C., Colby, L. A. and Company, F. A. D. (2013)
Therapeutic Exercise Foundations and Techniques.
Kisner, Carolyn and Allen Colby, Lynn. 2007. Exercise
Theraphy 5th Edition. USA: F.A. Davis Company,
Philadelphia.
Koman LA, Mooney et al. 2014. Management of Spasticity
in Cerebral Palsy with botulinum. J Pediatri Orthop.
Kumar, K. S. and Parveen, S. (2018) ‘Management and
Treatment for Cerebral Palsy in’, 11(2). doi:
10.5530/ijopp.11.2.23.
Kuperminc M & Richard D Stevenson. 2008; Growth and
Nutrition Disorders In Children with Cerebral Palsy.
Dev Disabil Res Rev. 2008; 14(2): 137–146.
doi:10.1002/ddrr.14
Mardiani, Elita.2006. Faktor-faktor resiko prenatal dan
perinatal kejadian cerebral palsy (studi kasus di YPAC
Semarang). Universitas Diponegoro. Kota Semarang.
Magutova, S.2008. Masgutova method of reflex integration
for children with cerebral palsy.edited:Susan Wenberg
and Mary Retschler
(USA);http://www.brianesti.com/pdfs/article¬_valier
i-cp.pdf. Diakses:12/07/16
Mutlu, A., Livanelioglu, A., Gunel, Mintaze K. 2008.
Reliability of Ashworth and Modified Ashworth Scales
in Children with Spastic Cerebral Palsy.
https://bmcmusculoskeletdisord.biomedcentral.com/a
rticles/10.1186/1471-2474-9-44. Diakses:12/07/16
Myoung-OK, Park, MPH. (2017) ‘Effects of gross motor
function and manual function levels on performance-
based ADL motor skills of children with spastic
cerebral palsy’, J. Phys. Ther. Sci. 29: 345–348, 2017
Novak, I., Mcintyre, S., Morgan, C., Campbell, L., Dark,
L., Morton, N., Morton, E., Wilson, Salli-A.,
Goldsmith, S. 2013. A Systematic Review of
Intervention For Children With Cerebral Palsy: State
Op The Evidence Basep. URL: onlinelibery. Niley.
Com
Nursalam.2003. Konsep dan penerapan metodologi
penelitian ilmu keperawatan: pedoman skripsi, tesis dan
instrumen penelitian keperawatan edisi pertama.
Jakarta : Salemba Medica.
Parkers, J., Donnelly, D. dan Hill N. 2005. Further
Information about Cerebral
Palsy. Scope Library and Information Unit. April
2005.http:/www.scope.org.uk/publications/index.sht
ml. Diakses:12/07/1
Palasari, Wina & Dewi Ika Sari Hari Purnomo. 2012.
Keterampilan Ibu Dalam Deteksi Dini Tumbuh
Kembang Terhadap Tumbuh Kembang Bayi. Jurnal
stikkes.
Pariera, F. N.2011. Pengaruh Neuro Developmental
Treatment Terhadap Penurunan Spatisitas Knee Joint
Pada Penderita Cerebral Palsy Spastic Diplegia.
Skripsi. Surakarta: Universitas Muhammadiyah
Surakarta.
Pratiwi, Gusti. 2011. Karakteristik Penderita Cerebral Palsy
yang mendapatkan pelayanan Fisioterapi di Makassar.
Makassar
Pin, T., Dyke, P., Chan, M. 2007. Effectiveness Of Passive
Stretching In Children With Cerebral Palsy.
URL:onlinelibery.wiley.com
Pocock. S.J.2008.clinical Trials, A Practical
approach.Chichestes, Jhon Willey and Sons.
Raine, Sue, et al. 2009. Bobath Consept : teory and clinical
practice in neurological rehabilitation. Willey-Blacwel.
A Jhon Wiley & Son, Ltd.,Publication.
Rumajugee, P., Bregman, T., Miler, Steven P., Yager,
Jerome Y., Fehling, Michael G. 2016. Rudent Hipoxsia
– Iskemic Models For Cerebral Palsy Research: A
Systematic Review. URL: www.mcbi.nlm.nih. Gov.
Diakses:12/07/16
Saputri, Marjuliana. 2013. Pengaruh NDT dan Mobilisasi
Trunk Terhadap penurunan Spatisitas pada Cerebral
Palsy Spastic Diplegi. Skripsi. Surakarta: Universitas
Muhammadiyah Surakarta.
Ryan M. McAdams, MD,*Sandra E. Juul, MD ‘Cerebral
Palsy: Prevalence, Predictability,and Parental
Counseling’, Vol.12 No.10 October 2011.
Saputri, Oktaviari Dwi. 2015. Penatalaksanaan Fisioterapi
Untuk Penderita Cerebral Palsy Spastik Diplegi Di
PNTC Karanganyar. Universitas Muhammadiyah
Surakarta. Surakarta.
Sankar Chitra and Nandini Mundkur (2005). Cerebral
Palsy–Definition, Classification, Etiology and Early
Diagnosis. India, [Indian J Pediatr 2005; 72 (10) :865-
868.
Combination of Trunk Mobilization and Neuro Development Treatment against Spasticity Reduction of Spastic Type Cerebral Palsy
489

Stephaniie, M. (2013) ‘Pathophysiology of cerebral palsy’,
111. doi: 10.1016/B978-0-444-52891-9.00016-6.
Surakarta, M. (2013) ‘CEREBRAL PALSY SPASTIC
DIPLEGI’.
Susanto (2014) ‘No Title’. Cerebral Palsy of Etiology, The
Danish society for CP, Jakarta.
Susanto, 2014, Penyebab Palsy Cerebral, diakses Tanggal
15/11/2014, dari http://www.pediatric.com/ISI 03.
Diakses:12/07/16.
Stevness, C. 2009. The Effect Of Positioning For Children
With Cerebral Palsy On Upper – Extremity Function.
URL: www. Tandfoonline.com. Diakses:12/07/16.
U. S. Departement of healh and human sence. 2013.
Intervention For Feeding And Nutrition For Cerebral
Palsy. URL: effective heathcare. Ahrg. Gov.
Waluyo, T.S.2010. Pengaruh Mobilisasi Trunk Terhadap
Penurunan Spastisitas Pada Cerebral Palsy Spastik
Diplegi. Skripsi, Surakarta : Universitas
Muhammadiyah Surakarta.
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
490
