
Strategy of Professional Care Provider in Package INA-CBG’s
Contribution Study Case RSU C Class Mekar Sari Bekasi
Widhi Jonathan
1
, Erlina Puspitaloka Mahadewi
2
, Ignatius Anindya Wirawan Nugrohadi
1
,
Sri Widodo
1
and Eko Suryo Nugroho
3
1
Public Health Sciences Study Program, Postgraduate Faculty, Respati Indonesia University, Jakarta, Indonesia
2
Public Health Sciences Study Program, Postgraduate Faculty, Esa Unggul University, Jakarta, Indonesia
3
Mekar Sari Hospital Bekasi, Mekar Sari Street No.1, East Bekasi, Jawa Barat, Indonesia
ekosnugroho@yahoo.co.id
Keyword: AHP, JKN, Package INA-CBG’s, Professional Care Provider or Profesional Pemberi Asuhan (PPA) Strategy.
Abstract: The application of the INA-CBG package rates requires hospital management to be able to streamline costs
and optimize hospital financial management, and carrying out quality control, cost control and access through
service cost calculations based on the unit cost calculation owned by the hospital. The purpose of this study
was to find out the PPA can strive for the optimal INA-CBG Package at Mekar Sari Hospital Bekasi. This
study uses the AHP method to determine solutions to various proposed problems. The sample of this research
is decision-makers Mekar Sari Bekasi Hospital. From the research results obtained the most dominant
problem factor data is INA-CBG’s Tariff (41.0%), then the health service behavior towards the Cost of
Treatment (35.1%), and Quality of Health Services (23.9%). Meanwhile, the most dominant solution in the
problem of the INA-CBG Package is the Improvement of INA-CBG’s Tariff of 47.1%, then the strategy of
implementing PPA in interprofessional collaboration by PPK and clinical pathway was 36.3%, and quality
and cost management strategies 16.6%. The conclusion of this study is that PPA can strive for optimally on
INA-CBG's Package at Mekar Sari Hospital Bekasi and provide quality health services that are standardized
for JKN patients.
1 INTRODUCTION
Hospital as an advanced referral health facility is one
of the important components for the providers of
health services in the implementation of Jaminan
Kesehatan Nasional (JKN) or know as the National
Health Insurance program. JKN is a part of public
policy as a result of the government's goodwill. The
success of the government's program in JKN, among
others, depends on the extent to which this policy is
implemented in the hospital (Thabrany H. 2014).
In accordance with the Regulation of the Minister
of Health, number 69 of 2016 concerning Standard
Tariffs for Health Services at First Level Health
Facilities and Advanced Level Health Facilities in the
implementation of JKN, the method of payment to the
first level health facilities is based on capitation of the
total number of participants who are registered at the
health facility. For the health services provided to the
participants by advanced level referral health
facilities, BPJS makes payments based on the
Indonesian Case-Based Groups (INA-CBG’s)
method (KemKes RI. 2016).
The tariff package of INA-CBG’s is a payment
system based on the diagnosis. In payments using this
system, both the hospital and the payer do not longer
specify the invoice based on the details of the given
services, but only submitting a patient’s diagnosis and
DRG (Disease-Related Group) code. The amount of
reimbursement of costs for the diagnosis has been
mutually agreed by providers/insurance or previously
determined by the government. The estimated length
of stay to be undertaken by the patients has also been
estimated beforehand. It is adjusted based on the type
of diagnosis and case of the disease (BPJS. 2014).
This claim payment system requires efficiency in the
implementation of health services for patients of
BPJS Kesehatan (BPJS. 2014).
One of the government's efforts to encourage
hospitals in the health services, safety, and protection
for the society is to require them to carry out
accreditation. According to Peraturan Menteri
Jonathan, W., Mahadewi, E., Nugrohadi, I., Widodo, S. and Nugroho, E.
Strategy of Professional Care Provider in Package INA-CBG’s Contribution Study Case RSU C Class Mekar Sari Bekasi.
DOI: 10.5220/0009770103510359
In Proceedings of the 1st International Conference on Health (ICOH 2019), pages 351-359
ISBN: 978-989-758-454-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
351

Kesehatan (Permenkes) or the Regulation of the
Minister of Health number 12 of 2012, accreditation
is an acknowledgment that is given to hospitals since
they have sought to continuously improve their
quality of services. This acknowledgment is given by
an independent institution that is in charge of
conducting accreditation and had received
recognition from the Minister of Health. The
independent institution which is in charge of
accrediting hospitals in Indonesia is Komisi
Akreditasi Rumah Sakit (KARS) or the Hospital
Accreditation Commission (KemKes RI. 2012).
One of the government's efforts to encourage
hospitals to prioritize services, safety, and protection
to the public is by requiring hospitals to carry out
accreditation (KemKes RI. 2012).
Accreditation is
very closely related to the quality of services provided
by hospitals. This means that if accreditation is done
well, there will be an increase in the quality of
hospital services (Lumenta N. 2003).
The implementation of Profesional Pemberi
Asuhan (PPA) or Professional Care Provider with
interprofessional collaboration by Panduan Praktek
Klinis (PPK) or Clinical Practice Guidance and
Clinical Pathway can be a means in realizing the
objectives of the hospital accreditation, namely
improving the quality of the hospital services,
increasing the patients’ safety in the hospital, and
increasing the protection of the patients, community,
and the hospital’s resources (KARS. 2017).
The
implementation of INA-CBG's package tariffs
requires the hospital management to be able to
streamline costs and optimize the hospital financial
management, as well as carry out quality control, and
cost and access control through the calculation of
service costs (cost of care) based on the calculation of
unit cost owned by the hospital (KemKes. 2013).
Based on observational data conducted at Mekar
Sari General Hospital Bekasi, there are several
problems in the service of JKN patients in which its
financing has not been found to be effective and
efficient. Hence, the hospital has not known the profit
or loss of the health service financing and the quality
of health services at Mekar Sari General Hospital
Bekasi namely the patients’ satisfaction with the
health services and readmissions of JKN patients
which can cause additional treatment costs that
cannot be claimed to BPJS Kesehatan.
Based on the background and some findings
concerning the implementation of the INA-CBG’s
package at the C Class Mekar Sari General Hospital,
it is very essential to formulate a study to arrange a
policy strategy in implementing the INA-CBG's
package for JKN patients at this hospital by using
Professional Care Provider through interprofessional
collaboration by PPK and Clinical Pathway to seek
optimal INA-CBG's package with good quality health
services.
2 LITERATURE REVIEW
JKN is not health insurance that prioritizes profit,
JKN is national health insurance that is socially
provided by the government to all Indonesian citizen
equally. The implementation of this social health
insurance is considered vital to be implemented in
Indonesia because it has several advantages. First, it
provides comprehensive benefits at affordable rates.
Second, it applies the principles of cost control and
quality control, so that the participants can get quality
services with controlled costs, not "up to the doctor"
or "up to the hospital". Third, this social health
insurance guarantees sustainable financing for health
services. Fourth, social health insurance can be used
throughout all areas of Indonesia. Therefore, to
protect all citizens, the membership of JKN is
mandatory (KemKes. 2012b).
Health facilities are required to provide the
service of medicines, medical devices, and
consumable medical materials. The service of
medicines, medical devices, and consumable medical
materials needed by the patients participating in JKN
are provided in accordance with the medical
indications. The service of medicines, medical
devices, and consumable medical materials at
advanced referral health facilities are some
components paid in the INA-CBG’s package.
Medicine services that are included in the INA-
CBG’s package and refer to the National Formulary
cannot be billed separately to BPJS and cannot be
charged to the participants. If the medications needed
in accordance with the medical indications at
advanced level referral health facilities are not listed
in the National Formulary, other medicines can be
used based on the approval of the Medical Committee
and the Head/Director of the Hospital (KemKes RI.
2016).
The determination of tariffs for JKN is regulated
in the Regulation of the Minister of Health of the
Republic of Indonesia number 64 of 2016 concerning
Health Service Tariff Standards in Implementing
Health Insurance Program. The regulation regulates
standard tariffs for Fasilitas Kesehatan Tingkat
Pertama (FKTP) or First Level Health Facilities and
Fasilitas Kesehatan Rujukan Tingkat Lanjutan
(FKRTL) or Advanced Level Referral Health
Facilities. For FTP, the applicable standard tariffs are
ICOH 2019 - 1st International Conference on Health
352
the Capitation Tariff and Non-Capitation Tariff.
Capitation tariffs are the amount of monthly payment
paid in advance by BPJS Kesehatan to FKTP based
on the number of registered participants regardless of
the type and number of the health services provided.
A non-capitation tariff is the amount of claim
payment by BPJS to FKTP based on the type and
number of health services provided. For FKRTL, the
applicable tariff is the INA-CBG's rate, which is the
amount of claim payments by BPJS for a service
package based on a disease diagnosis and procedure
grouping according to regional classifications and the
class of the hospital (KemKes RI. 2016).
The quality of health services refers to the level of
completeness of health services which on the one
hand can lead to each patient’s satisfaction in
accordance with the citizen average level of
satisfaction, as well as its implementation procedures
that are in accordance with the established ethical
codes and professional service standards (Azrul
Azwar. 1996).
Quality is a comprehensive and multi-facet
phenomenon. According to Lori Di Prete Brown in
his book “Quality Assurance of Health Care in
Developing Countries” quoted by Djoko Wijono,
several activities to maintain the quality may involve
the following dimensions (Djoko Wijono. 1999):
a.
Technical Competence, concerning the skills,
abilities, and appearance of officers, managers and
support staff. Technical competence relates to how
the officers follow the established service standards
in terms of accountability or dependability, accuracy,
reliability, and consistency.
b.
Access to Services, health services are not
impeded by geographical, social, economic, cultural,
organizational condition, or language barriers.
c.
Effectiveness, the quality of health services
depends on the effectiveness that is related to health
service norms and clinical guidelines according to the
existing standards.
d.
Good Human Relations instill trust and
credibility by appreciating, keeping confidentiality,
respecting, responsive, and giving attention. Poor
human relations will decrease the effectiveness of
technical competence in health services.
e.
Efficiency, efficient services will provide
optimal attention by maximizing the best service with
the owned resources. Poor service due to ineffective
norms or incorrect services must be reduced or
eliminated. In this way, the quality can be improved
while the costs are reduced.
f.
The Continuity of Service, clients will receive
the complete services needed (including referral)
without interruption, stopping, or repeating
unnecessary diagnostic and therapeutic procedures.
The clients
must have access to routine and preventive services
provided by the health workers who know the history
of their disease. They also have access to referrals for
specialized services and complete the needed follow-
up services.
g.
Safety, reducing the risk of injury, infection,
side effects, or other hazards associated with the
service.
h.
Comfort and Enjoyment, in the dimension of
comfort and enjoyment, it is related to the health
services that are not directly related to the clinical
effectiveness but can decrease the patients’
satisfaction and the willingness to return to the health
facilities to obtain the next services.
3 RESEARCH METHODOLOGY
This research is qualitative research based on the date
of the decision-makers’ ideas in reviewing the health
regulation at the C Class Mekar Sari General Hospital
Bekasi. The experts consist of the stakeholder group,
namely the Managing Director, Medical Manager, and
Financial Manager of the hospital who were
respondents according to the basis of problem and
solution in the AHP hierarchy that was formed.
Research design with Analytic Hierarchy Process
(AHP) model based on hierarchy was implemented
according to the agreement of decision-makers and
secondary data obtained from the literature. The
research was carried out for ± 3 months (May - July
2019) at this hospital.
The data collection technique through interviews
with experts were carried out in one place, namely: C
Class Mekar Sari General Hospital Bekasi. Literature
review (i.e., studies of relevant previous research
results, books, journals, and mass media).
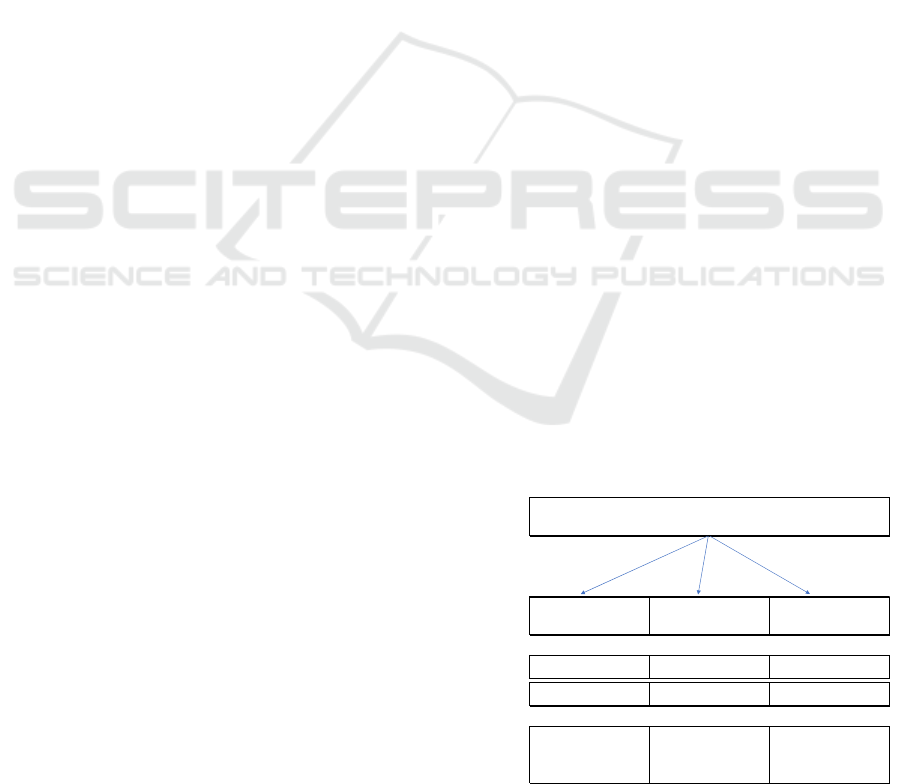
Figure 1: Analytic Hierarchy Process (AHP) Method.
level 1
Target
Level 2
Problem
Facto
r
A. THE QUALITY OF HEALTH
SERVICES
B. BEHAVIOR OF HEALTH
SERVICES TOWARDS
COST of TREATMENT
C. REGULATION MINISTRY of
HEALTH No. 64 of 2016 / INA-
CBG's TARIFF
A.1. PATIENT SATISFACTION /
PATIEN T EXPERIEN CE
B.1. HEALTH PLANNER C.1. INCENTIVE
A.2. READMISSION B.2. COST PLANNER
C.2. THE INCREAS E O F INA-
CBG's TARIFFS
Level 3
Solution
Policy
1.IMPLEMENTATION OF
PROFESSIONAL CARE
PROVIDER interprofessional
collaboration by PPK & Clinical
Pathway
2. QUALITY AND COST
MANAGEMENT
3. REVISION OF REGULATION
MINISTRY of HEALTH No. 64
of 2016
STRATEGY OF PROFESSIONAL CARE PROVIDER (PPA) IN CONTRIBUTION
OF INA-CBG PACKAGE'S CASE STUDY IN C CLASS OF GENERAL HOSPITAL
MEKAR SARI BEKASI
Strategy of Professional Care Provider in Package INA-CBG’s Contribution Study Case RSU C Class Mekar Sari Bekasi
353

4 RESEARCH RESULTS AND
DISCUSSION
4.1
Research Results
Based on the research results, it is known that among
the three problem factors, the most dominant are
Permenkes number 64 of 2016 / INA-CBG's Tariffs
(41.0%), the Health Service Behaviour towards the
Cost of Treatment (35.1%), and the Quality of Health
Services (23.9%). Further, based on the results of this
research, it is known that from the solution or
strategy, the most dominant is the revision of
Permenkes number 64 of 2016 / INA -CBG's tariffs of
47.1%, the implementation strategy of Professional
Care Provider through interprofessional collaboration
by PPK and clinical pathway of 36.3%, and a quality
and cost management strategy of 16.6%.
Figure 2: Result Analytic Hierarchy Process (AHP)
Method.
Further, the factor of health service quality is
23.9% which includes the strategy to improve
Permenkes number 64 of 2016 / INA-CBG's tariff by
0.471, the implementation strategy of Professional
Care Provider through interprofessional collaboration
by PPK and clinical pathway by 0.354, and the quality
and cost management strategies by 0.175.
Next, the problem factor of health service
behavior towards the cost of treatment is 35.1%
which includes the implementation strategy of
Professional Care Provider through interprofessional
collaboration by PPK and clinical pathway at 0.417,
the strategy to improve Permenkes number 64 of
2016 / INA-CBG's tariff of 0.408, and the quality and
cost management strategies of 0.174.
Further, the problem factor of Permenkes number
64 of 2016/ INA-CBG's tariff is 41.0% which
includes the improvement strategy of Permenkes
number 64 of 2016 / INA-CBG's tariff of 0.536, the
implementation strategy of Professional Care
Provider in interprofessional collaboration by PPK
and clinical pathway of 0.313, and the strategy of
quality and cost management of 0.151.
4.2
Discussion
4.2.1 Factors of Quality Problems in Health
Services
Tariff control is essential for health service providers
to maintain financial sustainability in economic
competition (Cleverly WO. 2002).
In addition to
tariffs, improving the quality of health services is also
a concern that must be considered by health service
providers and policymakers (Anderson GF. 2000).
If
the claim is too low, it cannot fund the treatment costs
that have been incurred. Hence, the health care
provider will try to reduce expenses by reducing
quality. If the claim is too high, the health service
provider has no effort to achieve efficiency and this
definitely will waste the available resources (Quentin
W. 2012).
It has been widely shown in various studies
that tariffs and the quality of health services are two
interrelated aspects (Younis M. 2005),
although often
policymakers consider that the tariffs and the quality
of health services are two separate aspects (Jiang HJ.
2006).
Hence, there are problems regarding the tariffs
and the quality of health services since it is difficult
to achieve both objectives simultaneously: affordable
tariffs with optimal quality of health services (Chang
L dan Lan YW. 2010)
.
4.2.2 Problem Factors of Healthcare
Further, the factor of health service quality is 23.9%
which includes the strategy to improve Permenkes
number 64 of 2016 / INA-CBG's tariff by 0.471, the
implementation strategy of Professional Care
Provider through interprofessional collaboration by
PPK and clinical pathway by 0.354, and the quality
and cost management strategies by 0.175.
Next, the problem factor of health service
behavior towards the cost of treatment is 35.1%
which includes the implementation strategy of
Professional Care Provider through interprofessional
collaboration by PPK and clinical pathway at 0.417,
the strategy to improve Permenkes number 64 of
2016 / INA-CBG's tariff of 0.408, and the quality and
cost management strategies of 0.174.
Further, the problem factor of Permenkes number
64 of 2016/ INA-CBG's tariff is 41.0% which
includes the improvement strategy of Permenkes
number 64 of 2016 / INA-CBG's tariff of 0.536, the
level 1
Target
Level 2
Problem
Factor
A. THE QUALITY OF HEALTH
SERVICES
(25%)
B. BEHAVIOR OF HEALTH
SERVICES TOWARDS COST of
TREATMENT
(25%)
C. REGULATION MINISTRY of
HEALTH No. 64 of 2016 / INA-
CBG's TARIFF
(25%)
A.1. PATIENT SATISFACTION /
PATIENT EXPERIENCE
B.1. HEALTH PLANNER C.1. INCENTIVE
A.2. READMISSION B.2. COST PLANNER
C.2. THE INC REASE O F INA-
CBG's TARIFFS
Level 3
Solution
Policy
1.IMPLEMENTATION OF
PROFESSIONAL CARE
PROVIDER interprofessional
collaboration by PPK & Clinical
Pathway
(30%)
2. QUALITY AND COST
MANAGEMENT
(21.1%)
3. REVISION OF REGULATION
MINISTRY of HEALTH No. 64
of 2016
(48.9%)
STRATEGY OF PROFESSIONAL CARE PROVIDER (PPA) IN CONTRIBUTION
OF INA-CBG PACKAGE'S CASE STUDY IN C CLASS OF GENERAL HOSPITAL
MEKAR SARI BEKASI
ICOH 2019 - 1st International Conference on Health
354
implementation strategy of Professional Care
Provider in interprofessional collaboration by PPK
and clinical pathway of 0.313, and the strategy of
quality and cost management of 0.151.
4.2.3 Workers’ Behaviours toward Cost of
Treatment
Changes in financing from Fee for Service (FFS) to
INA-CBG’s make the hospital facing a condition that
could be a threat or an opportunity. It is an opportunity
if the hospital can utilize the JKN program well, so that
the claim difference is positive since it is able to adjust
to INA-CBG’s tariffs. Meanwhile, it can be a threat to
hospital financial management because it has not been
able to provide effective and efficient services. Patients
who pay directly (Out of Pocket) feel they get a high
level of service compared to that from the insurance
payments. It affects the attitudes and behaviors of the
providers toward the patients’ expectations in which it
will decrease on the capitation system and will increase
in the system of fee for service, and this at the end will
affect the quality dimension of the provided services
(Sulistyo. 2010). Problem Factors of Permenkes
number 64 of 2016 (INA-CBG’s Tariffs)
Hospital fee is an aspect that is highly considered
by both private hospital and government hospital.
Government hospital fees are determined based on
local regulations, while private hospital fees are
determined based on the Minister of Health's
Regulation (Laksono. 2004).
Each hospital will set
tariffs according to their respective missions. Hospital
fee calculations are generally based on retrospective
cost calculations, meaning that the costs are billed
after the service has been carried out. Hence, it does
not encourage the team of health service providers to
achieve efficiency (Thabrany H. 1998).
Meanwhile,
as widely known, the INA- CBG's tariffs are arranged
based on prospective methods, so that in the future,
according to researchers, hospital fee calculations are
no longer based on retrospective cost calculations.
Hence, it is essential for hospitals to determine
standard procedures for dealing with diseases with
PPK and clinical pathways. As a result, in the era of
national health insurance, hospital teams can provide
optimal, efficient, and effective services.
Various problems that arise in the JKN
implementation, especially several aspects related to
the money that has been and will be paid by BPJS
Kesehatan, financial sufficiency, and the amount of
payment to health facilities. The amount of capitation
and most of the case base group that are not in
accordance with the average market cost cause many
cases (Thabrany H. 2014).
4.2.4 Solutions for the Implementation of
Professional Care Provider in
Interprofessional Collaboration by
PPK & Clinical Pathway
The quality of health services refers to the level of
completeness of their implementation which on the one
hand can lead to each patient’s satisfaction in
accordance with the citizen average level of
satisfaction, as well as its implementation procedures
that are in accordance with the established ethical
profession and standard. For the patients, good quality
is associated with recovery from disease or reduced
pain, speed of service, hospitality, and low service
tariff. On the other hand, the patients consider the
service quality is poor if the disease is not cured, the
queue is long, and the health workers are unfriendly
despite being professional. Hence, the quality of health
services is related to patient satisfaction. The patient
satisfaction is an important key to improve quality care
in the health services. Health care providers need to
realize that the main advantage of the health care
system is the patient. The satisfied patients will always
feel comfortable in the hospital for a long time, always
return to the hospital, and recommend the hospital to
other people. These 3 things are a part of the indicators
to measure patient satisfaction in assessing the health
care providers. With the increasing growth of hospital
which is directly proportional to the increase of the
patients’ knowledge about what should be obtained,
then they need hospitals that provide everything they
need (Azrul Azwar. 1996).
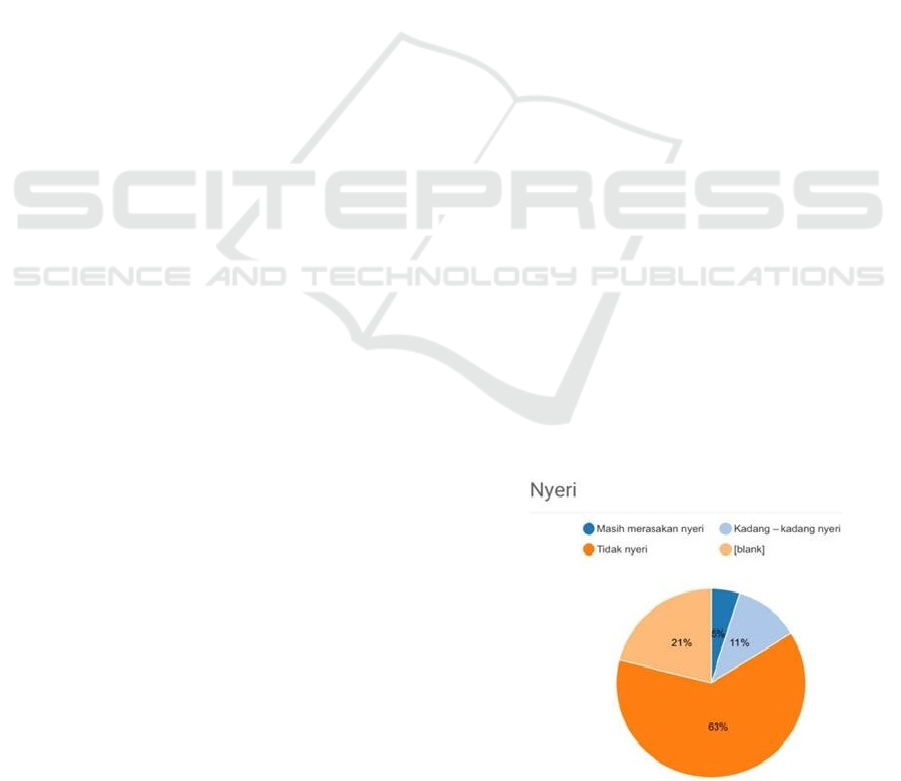
In Mekar Sari General Hospital, the patients’
satisfaction is achieved by the implementation of
Professional Care Provider that surveys their satis-
faction by providing questionnaires which are input to
the Mekar Sari General Hospital application, namely
patient experience. The following are the results of the
patient experience in the period of May-June 2019.
Figure 3: Results of the Patient Experience (ex. patient
complaints).
Strategy of Professional Care Provider in Package INA-CBG’s Contribution Study Case RSU C Class Mekar Sari Bekasi
355
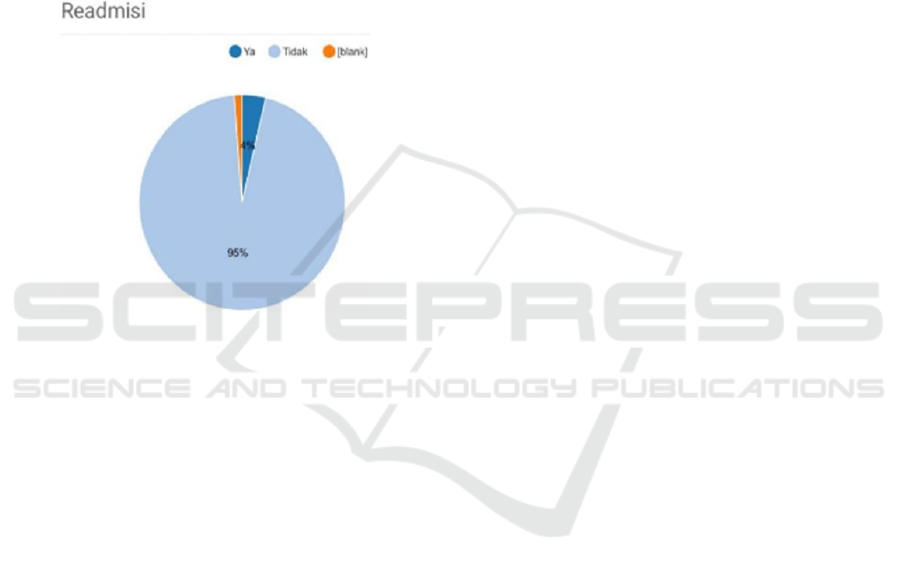
In addition, Mekar Sari General Hospital conducts
an assessment of patient readmissions in which these
readmissions relate to verification of claim
administration in BPJS Kesehatan with the diagnosis
of the same disease. If the patient enters with the same
diagnosis, a cross-check with the history of hospital
care in the previous episode is done to know whether
the patient comes home healed or in a state of forced
return, or referred in the previous nursing episode. If
the patient is discharged in a state of forced discharge,
then the episode of care in the readmission will be the
continuation of financing the same disease (BPJS.
2014).
Figure 4: Results of the Patient Experience (ex. disease
recurrence).
4.2.5 The Solution of Quality and Cost
Management
From the results of the research at Mekar Sari General
Hospital, in accordance with the statement of Dr. Evi
Andriwinarsih as the respondent "Professional Care
Provider as the health planner refers to Pedoman
Nasional Pelayanan Kedokteran (PNPK) or the
National Guidelines for Medical Services, Panduan
Praktek Klinis (PPK) or Clinical Practice Guidelines,
clinical pathways in accordance with the patients’
conditions, and the INA-CBG's package." Health
planner and cost planner in Professional Care
Provider at Mekar Sari General Hospital, namely
integrated service planning performed by doctors,
nurses, and all hospital components make a procedure
and diagnosis by minimizing the length of treatment,
the use of equipment and therapy while still
maximizing the quality of service based on the
patients’ condition and INA-CBG's tariffs (Mekar
Sari General Hospital Team) and Dr. Evi
Andriwinarsih stated that "Mindset of doctors’
habit/behavior for fee for service from medical and
pharmaceutical support is no longer a revenue center
and this must be changed according to INA-CBG’s
tariffs (package base).”
For the successful implementation of Professional
Care Provider, the doctors’ commitment is very
important because Professional Care Provider will be
a reference for the information of unit cost calculation
in order to achieve cost control and quality control.
This is in accordance with the health planner and cost
planner, which is to make examination plans and care
of patients who have a certain pattern, as an input for
the calculation of INA-CBG's funding, so that both
quality control and cost control can be achieved. All
service activities such as visits, actions, medicines,
medical devices and others that have been carried out
are informed to Dokter Penanggung Jawab Pelayanan
(DPJP) or the Doctor in Charge of Services to
complete the Professional Care Provider application
in accordance with the tariffs applied in hospitals, to
compare the total costs with the INA-CBG’s tariffs.
The system for calculating costs based on activity
is better known as the Activity Based Costing (ABC)
method (Semiarty dkk. 2011). In calculating the costs
incurred, ABC method will produce accurate cost
information because it uses more than one cost driver.
In this method, the activity is the focal point of the
action, so that each hospital has to develop an
Integrated Clinical Pathway as outlined in the form of
Standard Operating Procedures (SPO), so that the
flow of patient services is clearer (KemKes. 2013).
Information about the health planner contained in
the Professional Care Provider through
interprofessional collaboration by PPK and clinical
pathways will be the basic data. The ABC method
does not only pay attention to the calculation of the
unit cost of services or products but has a broader
scope including the reduction of costs obtained from
the management of activities that will be in line with
the cost control. Cost reduction in this method can be
implemented for all costs incurred, including at the
beginning of the activity, the production process, and
at the final stage of a series of activities. Hence, the
use of this method is able to accurately measure the
costs incurred from each activity to produce
appropriate tariffs.
4.2.6 The Solution of the Revision of
Permenkes Number 64 of 2016/
INA- CBG’s Tariffs
In accordance with the statement of the interviewee,
Ms. Tany Hilda "Based on the analysis, doctors use
INA-CBG's funds for one diagnosis of a maximum of
65% for hospitalization, for example in the case of
DHF. Moreover, currently, Mekar Sari General
ICOH 2019 - 1st International Conference on Health
356

Hospital is trying to save 35% of INA-CBG's budget
that will be used for indirect costs, namely salary
costs, other operational costs, maintenance
(infrastructure & facilities), electricity, and profits
that must be saved". Further, the statement from Dr.
Eko S. Nugroho, MPH "Mekar Sari General Hospital
is unable to develop the service capacity by
conducting research, but only able to pay for routine
operations and facility maintenance (not new
investment). Therefore, Mekar Sari General Hospital
hopes that there is an improvement in Permenkes
number 64 of 2016 that takes into account the
external costs, such as inflation and others.
Currently, BPJS patients in Mekar Sari General
Hospital reach 85%. The possible maintenance costs
are subsidized from 15% of private patients”.
Unit cost is the cost that needs to be incurred to
produce a product (goods or services) or cost that is
calculated for each product (services or goods) and is
also called as average cost (Horngren. 2006 &
Wonderling, D. R. 2005).
Hence, the amount (scope)
or type of service produced needs to be known to do
the calculation of the unit cost of services in the
hospital.
Tariff is the value of a service that is determined
by a measure of the amount of money based on the
consideration that with the value of that money, a
hospital is willing to provide services to patients
(Laksono. 2009).
Determining the hospital tariffs, it
must always be guided by the costs incurred to create
its services, because if the hospital sets the tariffs
below the costs, the hospital will suffer losses. Hence,
the survival of the hospital is not guaranteed. The
development of services at this time does not have to
always be at the determination of the cost of the
services provided and not merely on the competition
(Primadinta. 2009).
The tariffs are reviewed at least every two years.
The effort to review the tariffs is intended to
encourage the tariffs to reflect the actual cost of
services provided by the hospital. In addition, the
tariff review serves to improve the sustainability of
the prevailing tariff system, capable to support
medical needs needed and can provide rewards to
hospitals that provide services with good outcomes.
Another important thing is for hospitals to be able to
provide services that are in accordance with justice
and effectivity and to control the costs of health
services well (Peraturan Presiden RI. 2016).
5 CONCLUSIONS AND
SUGGESTIONS
5.1
Conclusions
The most dominant problem factors in Mekar Sari
General Hospital Bekasi are Permenkes number 64 of
2016 / INA-CBG's Tariffs (41.0%), the Health Care
Behaviour towards the Cost of Treatment (35.1%)
and the Quality of Health Services (23.9%). The most
dominant solutions or strategies are the improvement
of Permenkes number 64 of 2016 / INA-CBG's tariff
of 47.1%, the implementation strategy of Professional
Care Provider collaborating interprofessionally by
PPK and clinical pathway by 36.3%, and the strategy
of quality and cost management of 16.6%.
Professional Care Provider can work optimally on
the INA-CBG's package at the hospital to JKN
patients in accordance with the Regulation of the
Minister of Health number 64 of 2016 concerning
Health Service Tariff Standards in Providing Health
Insurance Program. Professional Care Providers can
provide quality health services that are standardized
to JKN patients in C Class Mekar Sari General
Hospital Bekasi, namely the presence of Patient
Experience indicators and patient readmissions.
Professional Care Providers can provide solutions in
the workload to obtain unit costs by diagnosis with a
considerably long process. Based on the interviews
with the Financial Manager of Mekar Sari General
Hospital (respondent), patients who are referred back
to FKTP can influence hospital revenue.
Professional Care Provider provides step by step of
the changes of the health service behaviors toward the
cost of treatment by means of the health planner and
cost planner contained in the application of Value
Base Care (VBC) 19 version 1.5. 8. Professional Care
Provider can provide information of positive
difference towards the INA-CBG’s package for JKN
patients in the C Class. Mekar Sari General Hospital
Bekasi cannot develop health service capacity (new
investment), but can survive with the existence of
JKN.
5.2
Suggestions
5.2.1 Hospital
1.
It is suggested that Mekar Sari General Hospital
Bekasi commits to implement Professional Care
providers to improve the quality of its health services,
namely the Patient Experience.
2.
It is suggested that the hospital change the habits or
behaviors of the health workers from volume-based
Strategy of Professional Care Provider in Package INA-CBG’s Contribution Study Case RSU C Class Mekar Sari Bekasi
357

to value-based on health services, so that the decrease
in the number of patient readmissions that can cause
hospital loss can be avoided. It is because when
patients return to the hospital in less than 30 days with
the same coding, BPJS Kesehatan cannot accept the
claim.
3.
Mekar Sari General Hospital can also review the
regulation of INA-CBG's package budget saving of
35% which is used as indirect cost.
5.2.2 Government (The Ministry of Health)
1.
It is suggested that there is an improvement of
Permenkes number 64 of 2016 / INA-CBG's tariffs in
accordance with the Presidential Regulation number
28 of 2016 which mandates that the tariffs be
reviewed at least every two years so that the
business of private hospitals can be sustainable
by simultaneously increasing the quality and the
capacity of the health services.
2.
It is suggested that there is an improvement in INA-
CBG’s tariffs, which is a minimum of 25% difference
between the INA-CBG's tariffs for government
hospitals and that for private hospitals. This study
shows that there is 35% for indirect costs where the
government hospitals are not burdened, for example
for employee salary costs.
3.
The government can give rewards or incentives for
the hospitals that provide services with good
outcomes in accordance with the targeted indicators,
namely the national readmission rates, and increasing
referral patients (PRB).
5.2.3 The Next Researchers
It is suggested that the next researchers conduct
further quantitative research on INA-CBG’s tariffs
and the quality of health services at Mekar Sari
General Hospital, Bekasi.
REFERENCES
Thabrany H. 2014. Jaminan Kesehatan Nasional. Jakarta:
Raja Grafindo Persada.
Kementrian Kesehatan Republik Indonesia. 2016.
Peraturan Menteri Kesehatan Republik Indonesia
Nomor 64 Tahun 2016 Tentang Standar Tarif
Pelayanan Kesehatan Dalam Penyelenggaraan
Program Jaminan Kesehatan. Jakarta: Kementerian
Kesehatan RI.
Badan Penyelenggara Jaminan Sosial Kesehatan. 2014.
Peraturan BPJS No 1 tentang Penyelenggaraan
Jaminan Kesehatan. Jakarta: BPJS
Kementrian Kesehatan Republik Indonesia, 2012. Tahun
2012 KARS Fokus Standar Akreditasi Baru Rumah
Sakit. URL: http://buk.kemkes.go.id/index.php?
option=com_content&view=article&id=192:tahun-
2012-kars-fokus-standar-akreditasi-barurumah-sakit,
diakses 17 september 2014.
Lumenta N. 2003. Akreditasi rumah sakit di luar negeri.
Makalah dalam pelatihan akreditasi RS di Dinkes.
Jakarta: Dinas Kesehatan DKI Jakarta
Komisi Akreditasi Rumah Sakit, 2017. Standar Nasional
Akreditasi Rumah Sakit Edisi 1. Jakarta: Kementerian
Kesehatan RI.
Kementerian Kesehatan Republik Indonesia. 2013.
Peraturan Menteri Kesehatan Republik Indonesia
Nomor 12 Tahun 2013 Tentang Pola Tarif Badan
Layanan Umum Rumah Sakit Di Lingkungan
Kementerian Kesehatan. Jakarta: Kementerian
Kesehatan RI.
Kementrian Kesehatan Republik Indonesia. 2012b. Buku
Pegangan Sosialisasi Jaminan Kesehatan Nasional
(JKN) Dalam Sistem Jaminan Sosial Nasional. Jakarta:
Kementrian Kesehatan RI.
Azrul Azwar. Menuju Pelayanan Kesehatan yang Bermutu.
Jakarta: Yayasan Penerbitan IDI. 1996. hal. 48
Djoko Wijono. Manajemen Mutu Pelayanan Kesehatan
Vol. I. Surabaya: Airlangga University Press, 1999. Cet.
Ke-1. hal. 3
Cleverly WO. 2002. The hospital cost index: a new way to
asses relative cost-efficiency. Healthcare Financial
Manajement. Vol 56(7): 36-42
Anderson GF, Hurst J, Hussey PS dan Jee- Hughes M.
2000. Health spending and outcomes: trends in OECD
countries. Health Affairs. Vol 19(3): 150-157
Quentin W, Scheller-Kreinsen D, Blumel M, Geissler A
dan Busse R. 2012. Hospital payment based on
diagnosis related groups differs in europe and holds
lessons for the united states. Health Affairs. Vol 32(4):
713-723
Younis M, Rivers PA dan Fottler MD. 2005. The impact of
HMO and hospital competition on hospital costs.
Journal healthcare finance. Vol 31(4): 60-74
Jiang HJ, friedman B dan Begun JW. 2006. Factors
assiciated with high quality/ low cost hospital
performance. Journal Healthcare Finance. Vol 32(3):
39-52
Chang L dan Lan YW. 2010. Has the national insurance
scheme improved hospital efficiency in taiwan?
identifying factors that affects its efficiency. African
Journal of Business Management Vol 4 (17): 3752-
3760
Sulistyo. 2010. Hubungan antara sistem pembiayaan
dengan kualitas pelayanan Dipuskesmas Slogohimo
Wonogiri. Surakarta: Program Pasca Sarjana
Universitas Sebelas Maret.
Trisnantoro, Laksono. 2004. Memahami Penggunaan Ilmu
Ekonomi Dalam Manajemen Rumah Sakit. Yogyakarta:
Gadjah Mada University Press.
Thabrany H. 1998. Penetapan dan simulasi tarif rumah
sakit. Pelatihan RSPAD 2-5 Nopember 1999
ICOH 2019 - 1st International Conference on Health
358

Semiarty dkk. 2011. Metode Activity Based Costing Sebagai
Penentuan Tarif Rawat Inap Di RSJ Puti Bungsu.
Padang: Program Pascasarjana Universitas Andalas.
Horngren, Charles T., Srikant M. Datar, dan George Foster.
(2006). Cost Accounting: A Managerial Emphasis. 12th
edition. New Jersey: Pearson Prentice Hall.
Wonderling, D. R. Gruen and N. Black. 2005. Introduction
to Health Economics, Open University Press, United
Kingdom: Mc Graw - Hill Education.
Trisnantoro. Laksono. 2009. Pedoman Operasional Sistem
Pembiayaan dan Jaminan Kesehatan. Central of
Health Service Management. Yogyakarta: Fakultas
Kedokteran Universitas Gadjah Mada.
Primadinta 2009, Analisa Cost Sharing Perhitungan Tarif
Hemodialisis (HD) Masyarakat Miskin di Rumah Sakit
Umum PKU Muhammadiyah Unit 1 Yogyakarta.
Yogyakarta: Program Studi Sarjana Ilmu Kesehatan
Masyarakat UAD.
Peraturan Presiden Republik Indonesia Nomor 28 tahun
2016. Tentang Perubahan Ketiga Atas Peraturan
Presiden Nomor 12 Tahun 2013 tentang Jaminan
Kesehatan. Jakarta: Kementrian Hukum dan Hak Asasi
Manusia Republik Indonesia.
Strategy of Professional Care Provider in Package INA-CBG’s Contribution Study Case RSU C Class Mekar Sari Bekasi
359
