
Differences of Medical Adherence on the Level I and Level II of
Hypertension Patients in Kalideres Sub-District Primary Health
Center Year of 2019
Siti Chomidah and Devi Angeliana Kusumaningtiar
Department of Public Health, Faculty of Health and Sciences, Universitas Esa Unggul, Jakarta, 11510, Indonesia
Keywords: Non Communicable Diseases, Hypertension Level I, Hypertension Level II, Medication, Medical
Adherence.
Abstract: One of the non-communicable diseases is hypertension, this disease is a health problem because we are not
aware that we are including hypertensive sufferers and because of this unconsciousness causes medical
related diseases to be excluded. Hypertension is an increase in blood pressure which will discuss target
organs such as stroke (for the brain), coronary heart disease (for heart vessels) and right ventricular
hypertrophy / left ventricular hypertrophy (for the heart muscle) with the main target is the stroke that brings
high mortality. Hypertension is a condition where systolic blood pressure ≥140 mmHg and diastolic
pressure ≥ 90 mmHg. The purpose of this study was to study the differences of medical adherence on the
Level I and Level II of hypertension patients in Kalideres Sub-district Primary Health Center Year of 2019.
This study used quantitative with cross-sectional research methods with a sample of 117 people. Source of
data analysis using Mann Whitney. Based on the result of Mann Whitney analysis was found p-value is
0,000 that means there are differences in Medical Adherence on the Level I and Level II of Hypertension
Patients.
1 PRELIMINARY
One of the non-communicable diseases is
hypertension, this disease is a health problem
because we are not aware that we are including
hypertensive sufferers and because of this
unconsciousness causes medical related diseases to
be excluded. Hypertension is an increase in blood
pressure which will discuss target organs such as
stroke (for the brain), coronary heart disease (for
heart vessels) and right ventricular hypertrophy / left
ventricular hypertrophy (for the heart muscle) with
the main target is the stroke that brings high
mortality (Bustan, 2007).
Increased blood pressure is one of the main risk
factors for global death. Increased blood pressure is
a major risk factor for coronary and ischemic heart
disease and hemorrhagic stroke. Blood pressure
levels have been proven to be positively and
continuously associated with the risk of stroke and
coronary heart disease. In some age groups, the risk
of cardiovascular disease doubles for every increase
in blood pressure of 20/10 mmHg, starting as low as
115/75 mmHg. In addition to coronary heart disease
and stroke, complications of increased blood
pressure include heart failure, peripheral vascular
disease, kidney disorders, retinal bleeding and vision
problems. Treating systolic blood pressure and
diastolic blood pressure to less than 140/90 mmHg is
associated with a reduction in cardiovascular
complications. Based on information released by
WHO, one in three adults has high bloodpressure in
the Southeast Asia region. Nearly 1.5 million people
die from high blood pressure every year making it a
major risk factor for death in the Southeast Asia
region (WHO, 2018).
No symptoms are a major obstacle in
recognizing high blood pressure and treating it. This
condition does not give notice of his arrival. The
damage caused continues so that you still feel
healthy. Many hypertensive patients do not realize
there is something wrong with them. Often, the first
sign of this problem is a stroke or heart attack that
actually can be prevented if hypertension is
recognized and treated early on (Wade, 2016).
338
Chomidah, S. and Kusumaningtiar, D.
Differences of Medical Adherence on the Level I and Level II of Hypertension Patients in Kalideres Sub-District Primary Health Center Year of 2019.
DOI: 10.5220/0009768503380345
In Proceedings of the 1st International Conference on Health (ICOH 2019), pages 338-345
ISBN: 978-989-758-454-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Globally in 2015, 1 in 4 men and 1 in 5 women.
In 2015, 28% of the population in low-income
countries had high blood pressure, compared to 18%
of the population in high-income countries. A
review of current trends shows that the number of
adults with increased blood pressure increased from
594 million in 1975 to 1.13 billion in 2015, with an
increase seen mostly in low and middle-income
countries (WHO, 2018).
The prevalence of hypertension according to the
results of measurements in the population aged ≥18
years in 2018 has increased by 8.3%. The prevalence
in 2013 was 25.8% in 2018 to 34.1%. While the
proportion of history of taking drugs and the reasons
for not taking drugs in the population of
hypertension in 2018 reached 45.6%. Reasons for
non-compliance with these drugs were 59.8%
feeling healthy, 31.3% did not routinely go to health
care facilities, 14.5% took traditional medicine,
12.5% other reasons, 11.5% often forgot, 8.1% was
not able to buy routine drugs, 4.5% cannot stand the
side effects of drugs, 2% do not exist in health care
facilities. The prevalence of DKI Jakarta for
hypertension according to the results of
measurements in the population aged ≥18 years in
2018 is above 30% (Kemenkes RI, 2018).
Hypertension is a major risk factor for coronary
heart disease, chronic kidney disease, ischemic,
hemorrhagic and stroke, if left uncontrolled,
complications due to hypertension are heart failure,
peripheral vascular disease, kidney failure, retinal
bleeding, vision problems, stroke and dementia
(WHO, 2018).
Hypertension not only damages blood vessels but
also organs such as the heart, brain, kidneys, and
eyes. The longer you suffer from hypertension the
greater the chance of organ damage. As a result,
serious conditions such as heart disease, stroke,
kidney disease and eye damage is occurring (Casey
et al., 2006)
Risk factors for hypertension can be divided into
2 (two), which are factors that cannot be changed
and factors that can be changed. Factors that cannot
be changed include genetics, age, gender and race,
while factors that can be changed include smoking,
obesity, lazy lifestyle (Less Motion), excess salt,
caffeine and alcohol use (Casey et al., 2006).
Adherence to taking medication in hypertensive
patients is very important because blood pressure
can be controlled by taking regular antihypertensive
medication so that in the long run the risk of damage
to important body organs such as the brain, heart and
kidneys can be reduced (BPOM, 2006). Compliance
with the treatment of hypertension patients is
important because hypertension is an incurable
disease but must always be controlled or controlled
so that complications do not occur that can lead to
death (Palmer & Williams, 2007).
According to a research journal entitled
Determinants of adherence to hypertension treatment
patients at first-level health facilities in Palembang
in 2017 concluded that patient compliance in
undergoing hypertension treatment is also a
determinant that influences blood pressure control
(Liberty et al., 2017)
Kalideres Sub-district Primary Health Center is
one of the working areas of the West Jakarta District
Health Office, based on interviews conducted with
one of the Kalideres District Primary Health Center
staff, one of the causes of high hypertension rates in
Kalideres Sub-District Primary Health Center is
because the Kalideres Sub-District Primar Health
Center is a referral Health Center of 12 (two twelve)
Village Office of Primary Health Center in the
Kalideres sub-district area.
Based on data found during direct observation of
the primary health center there is an increase in the
number of hypertensive patients. In 2017,
hypertension patients numbered 12,171 cases,
increasing in 2018 to 13,648 cases. From the last
two months data which is in February 2019 and
March 2019, there is an increase in the number of
cases of hypertension from 555 cases to 588, which
is an increase of 5%.
Based on the results of interviews with the
Kalideres District Primary Health Center staff one of
the causes of the increasing number of hypertension
patients with level II is due to the non-compliance of
hypertension patients with the treatment control
schedule, this causes patients not to receive
antihypertensive drugs which they should consume
until the next control schedule. One of the effects of
level II hypertension is death, from interviews with
the Kalideres District Primary Health Center staff
supported by a 2018 surveillance report, 36 cases of
patients died from hypertension in 2018.
2 THEORY REVIEW
2.1 Hypertension
Hypertension is an increase in blood pressure which
will discuss target organs such as stroke (for the
brain), coronary heart disease (for heart vessels) and
right ventricular hypertrophy / left ventricular
hypertrophy (for the heart muscle) with the main
Differences of Medical Adherence on the Level I and Level II of Hypertension Patients in Kalideres Sub-District Primary Health Center
Year of 2019
339
target is the stroke that brings high mortality
(Bustan, 2007).
Basic hypertension is a steady increase in blood
pressure specifically, diastolic pressure exceeds
95mm of mercury that cannot be connected with
other organic causes (Wade, 2016).
Hypertension is often called a silent killer
because patients with hypertension are usually
asymptomatic. The main physical discovery is an
increase in blood pressure. The average of
measurement at twice or more times in two times of
control is determined to diagnose hypertension
(Muchid, 2006). In primary health services, a
diagnosis of hypertension is made by a doctor, after
getting an increase in blood pressure in twice
measurements with a distance of one week. The
diagnosis of hypertension is made when the blood
pressure is ≥ 140/90 mmHg if one of both systolic
and diastolic increases is sufficient to establish a
diagnosis of hypertension (Departemen Kesehatan
RI, 2013).
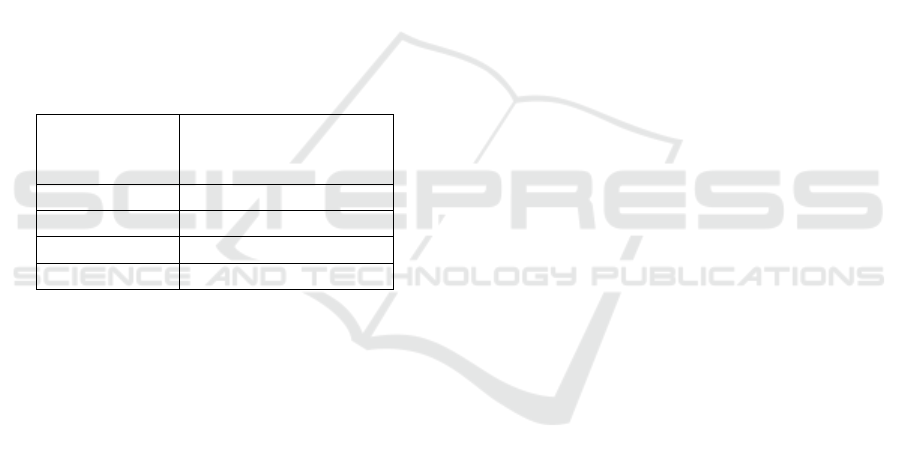
Table 1: Classification of Blood Pressure.
Classification
of Blood
Pressure
Systolic and Diastolic
Pressure (mmHg)
Normal < 120 and < 80
Pre-
hi
120 – 139 or 80 – 89
Stage I
i
140 – 159 or 90 – 99
Stage II
i
> 160 or > 100
2.2 Hypertension Risk Factors
2.2.1 Risk Factors That Cannot Be Changed
• Genetic
A close family history of suffering from
hypertension (heredity) also increases the risk
of hypertension, especially primary
(essential) hypertension. Genetic factors are
also related to metabolism of salt regulation
and cell membrane renin (Departemen
Kesehatan RI, 2013).
• Age
Age affects the occurrence of hypertension.
With increasing age, the risk of developing
hypertension becomes greater. In the elderly,
hypertension is mainly found only in the form
of an increase in systolic blood pressure. This
incident was caused by structural changes in
large blood vessels (Departemen Kesehatan
RI, 2013).
• Gender
The gender affects the occurrence of
hypertension. Men have a risk of about 2.3
times more systolic blood pressure increases
compared to women because men are
suspected of having a lifestyle that tends to
increase blood pressure. However, after
entering menopause, the prevalence of
hypertension in women increases
(Departemen Kesehatan RI, 2013).
• Race
African Americans show higher levels of
hypertension than other populations and tend
to develop more early and aggressively. They
are nearly twice as likely to have a fatal
stroke, one and a half times as likely to die of
heart disease, and four times more likely to
experience kidney failure compared to the
caucasian race. Hypertension is the number
one cause of death in African-Americans
2.2.2 Changeable Risk Factors
• Smoke
Toxic chemicals such as nicotine and carbon
monoxide inhaled through cigarettes that enter
the blood stream can cause high blood pressure.
Smoking will increase heart rate, so the oxygen
demand of the heart muscles increases
(Departemen Kesehatan RI, 2013).
• Obesity
Bodyweight and body mass index (BMI)
correlates directly with blood pressure,
especially systolic blood pressure where the
relative risk for hypertension in obese people is
5 times higher for hypertension compared to a
normal person. Meanwhile, in patients with
hypertension found about 20-30% overweight
(Departemen Kesehatan RI, 2013).
• Lifestyle (less motion)
Regular exercise can help lower blood pressure
and benefit people with mild hypertension. By
doing regular aerobic exercise your blood
pressure can drop, even if you haven't lost
weight (Departemen Kesehatan RI, 2013).
• Excess Salt
Salt causes a build up of fluid in the body
because it draws fluid outside the cell so that it
is not released, thus increasing the volume of
blood pressure (Departemen Kesehatan RI,
2013).
ICOH 2019 - 1st International Conference on Health
340
• Caffeine
Caffeine is a methylxanthine derivative found in
tea, coffee, and chocolate. Coffee is a beverage
ingredient that contains caffeine. Coffee also has
a bad impact on the heart. Caffeine can stimulate
the heart to work faster so it drains more fluid
every second. The habit of drinking coffee is
obtained from one cup of coffee containing 75-
200 mg of caffeine.
• Alcohol Use
The effect of alcohol on rising blood pressure has
been proven. Allegedly increased cortisol levels,
increased red blood cell volume and increased
blood viscosity play a role in raising blood
pressure (Departemen Kesehatan RI, 2013).
2.3 Management of Hypertension
Disease
2.3.1 Primary Stage
Primary prevention is an effort to modify risk factors
or prevent the development of risk factors, before the
start of pathological changes with the aim of
preventing or delaying the occurrence of new cases of
disease. The primary stage of managing hypertension
is an initial prevention effort before a person suffers
from hypertension through a counseling program and
controlling risk factors to the wider community by
prioritizing high-risk groups.
2.3.2 Secondary Stage
Early detection of disease is often called screening.
Early detection in the preclinical stage allows
immediate treatment (prompt treatment) which is
expected to provide a better prognosis about the end
of the disease than given late. In the prevention of
this secondary stage, blood pressure checks are
carried out regularly as a form of screening and also
compliance with treatment for people who have
suffered from hypertension.
2.3.3 Tertiary Stage
Management of the tertiary stage is an effort to
prevent more severe complications or death. Tertiary
prevention is an effort to prevent diseases that lead
to worse diseases, with the aim of improving the
quality of life of patients. Tertiary prevention is
focused on rehabilitation and recovery after illness to
minimize morbidity, disability and improve quality
of life.
3 RESEARCH METHODS
The sampling technique in this study is by accidental
sampling. Accidental sampling is a sampling
technique based on coincidence, i.e. consumers who
incidentally meet with researchers can be used as
samples if viewed by people who happen to be found
suitable as sources of data (Sugiyono, 2016).
The research instrument using medical and
medication adherence was obtained from a
questionnaire. The compliance questionnaire is the
standard Morisky Medication Adherence Scale
(MMAS) questionnaire consisting of 8 questions that
have been translated into Indonesian.
4 RESULTS AND DISCUSSION
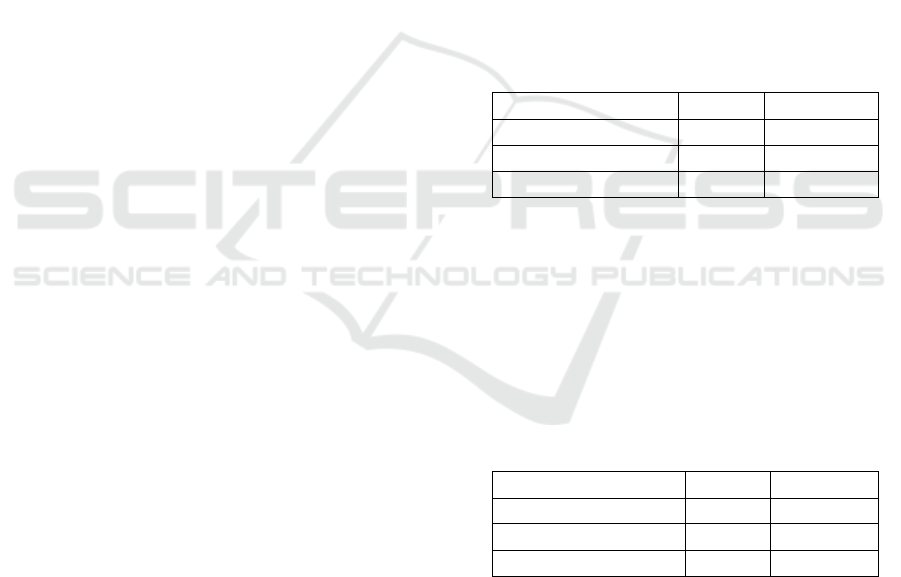
Table 2: Overview of the Distribution of Hypertension
Frequencies in the Kalideres District Primary Health
Center in 2019.
Hypertension Amount Percentage
Hypertension Level II 22 18,8%
Hypertension Level I 95 81,2%
Total 117 100
Based on the results of the study in table 4.1 above,
it shows that the proportion of respondents with
hypertension level I was 95 people (81.2%) and the
proportion of respondents who had hypertension
level II was 22 (18.8%) with a total number of
respondents of 117 people.
Table 3: Descriptions of Frequency Distribution of
Treatment Compliance in Patients with Hypertension
Disease in Kalideres District Primary Health Center in
2019.
Adherence Amount Percentage
Not Adhere 47 40,2
Adhere 70 59,8
Total 117 100
Based on the results of table 4.2 above shows
that the proportion of patients with hypertension
who adhered to medication as many as 70 people
(59.8%) and the proportion of patients
withhypertension who did not adhere with
medication as many as 47 people (40.2%) with a
total of 117 respondents person.
Differences of Medical Adherence on the Level I and Level II of Hypertension Patients in Kalideres Sub-District Primary Health Center
Year of 2019
341
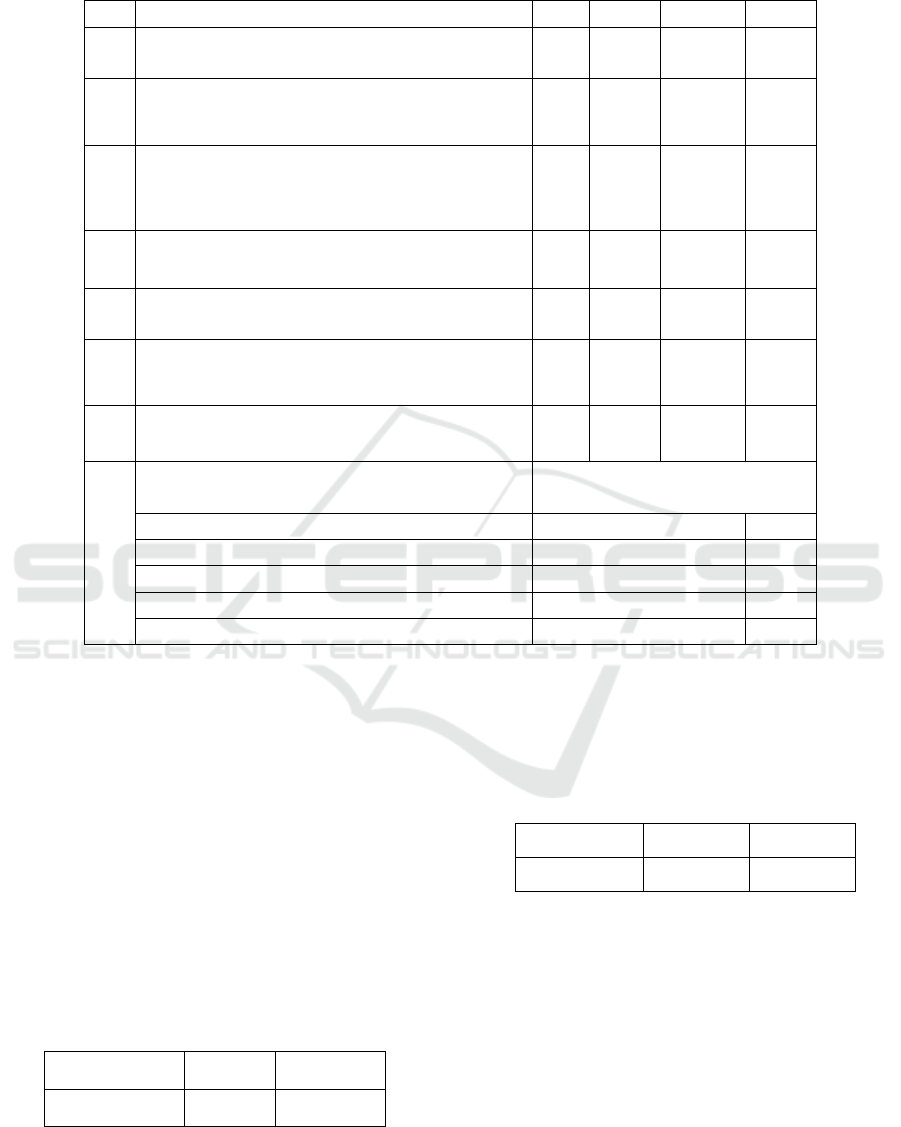
Table 4: Normality Test Compliance Score Taking Medicines in the Group I Patients with Level I and Level II
Hypertension in the Kalideres District Primary Health Center in 2019.
No MMAS – 8 Items Yes % No %
1
Do you sometimes forget to take
antihypertensive medicine?
38 32,5 79 67,5
2
Think about the last 2 weeks, is there a day when you did
not take antihypertensive medication?
26
22,2
91
77,8
3
Have you ever reduced or stopped treatment without
telling your doctor because when you took the medicine
you felt more unwell?
26
22,2
91
77,8
4
When traveling, do you sometimes forget to bring
antihypertensive medicine?
13 11,1 104 88,9
5
Did you take your antihypertensive medication yesterday?
106 90,6 11 9,4
6
When you feel your blood pressure is in control, have you
ever stopped your medication?
18
15,4
99
84,6
7
Have you ever felt disturbed/fed up with your routine
medication schedule?
35 29,9 82 70,1
8
How difficult do you remember taking your
medicine?
a. Never 83 70,9
b. Once in a while 17 14,5
c. Somestimes 12 10,3
d. Usually 5 4,3
e. Always 0 0
Based on the results of the distribution of the
MMAS-8 questionnaire, it showed that the highest
proportion of questions related to adherence to
taking hypertension patients was the question "did
you take antihypertensive medication yesterday?"
106 respondents answered, "Yes" (90.6%). While
the highest proportion of non-compliance with
taking medication is obtained from the question "do
you sometimes forget to take antihypertensive
medicine?" 38 respondents answered, "Yes"
(32.5%).
Table 5: Normality Test Compliance Score Taking
Medicines in the Group I Patients with Level I and Level
II Hypertension in the Kalideres District Primary Health
Center in 2019.
Variable
P-value
Remarks
Adherence 0,000 Abnormal
Based on table 4.4 it is found that the compliance
score is 0,000 less than the significant value
(<0.05) which means that the data is not normally
distributed.
Table 6: Differences in Medication Compliance in the
Level I and Level II Hypertension Patients in the
Kalideres District Primary Health Center in 2019.
Variable
P-value
Remarks
Adherence 0,000 Abnormal
Based on the results of the statistical tests
performed using the Mann Whitney test in table 4.5,
the sig or p-value of 0,000 is obtained, which means
the value <significant value is 0.05. So it can be
concluded that refusing Ho, which means there is a
significant difference between adherence to taking
medication in the group of patients with
hypertension level I and hypertension level II.
Based on the results of observations in the
Kalideres District Primary Health Center,
hypertension entered into the 10 biggest diseases.
From interviews with one of the health workers,
ICOH 2019 - 1st International Conference on Health
342

when hypertension patients are found to be
medically in need of more serious help where the
primary health center feels that patients need to get
treatment from specialists or subspecialists, these
patients will be given a referral letter to the hospital
or health facility level 2.
Based on interviews with several respondents the
reasons for their non-compliance with the above
questions are due to forgetting about taking
medication schedules, fear of the effects caused by
antihypertensive medicine such as dry cough, nausea
and dizziness and there are those who prefer to treat
hypertension by using herbal medicines.
In regards to the results of interviews that show
non-compliance, it is advisable to include family
members in the treatment of patients, especially for
elderly patients in order to increase the participation
of family members in the treatment of hypertension,
so that there are reminders of the schedule of taking
antihypertensive medication according to the
treatment suggested by health workers.
Based on the results of the statistical tests
performed using the Mann Whitney test in table 4.5,
the sig or p-value of 0,000 is obtained, which means
the value <significant value is 0.05. So it can be
concluded that refusing Ho, which means there is a
significant difference between adherence to taking
medication in the group of patients with
hypertensive level I and hypertension level II.
The results of this study are in line with research
conducted by Baiq Leny Nopitasari, Wirawan
Adikusuma, Nurul Qiyaam and Ayu Fatmala who
stated that there was a significant influence or
difference in medication adherence to blood pressure
with a p-value of 0,000 (Nopitasari, et al., 2018).
Adherence to taking the medication in
hypertensive patients is very important because
blood pressure can be controlled by taking regular
antihypertensive medication so that in the long run
the risk of damage to important organs of the body
such as the brain, heart and kidneys can be reduced
(BPOM, 2006).
Medical adherence of hypertension patients is
important because hypertension is an incurable
disease but must always be controlled or controlled
so that complications do not occur that can lead to
death (Palmer &Williams, 2007). Based on
interviews with several respondents the reason for
their non-compliance with taking antihypertensive
medicine is because patients forget about taking
medication schedules, fear of the effects caused by
antihypertensive drugs such as dry cough, nausea
and dizziness and there are those who prefer to treat
hypertension by using herbal medicines.
Efforts have been made by the primary health
center related to medical adherence on patients with
hypertension, which is by reminding and educating
patients to control in accordance with the time that
has been scheduled or agreed, other than that the
primary health center will send reminders to patients
through WhatsApp group, where this activities is
part of the Prolanis Program (Program Pengelolaan
Penyakit Kronis).
In regards to not adherence to patients with
hypertension on taking medication, it is suggested to
primary health center to make a form of adherence
to take anti-hypertensive medication. The form
contains information and instructions about
antihypertensive medicine such as drug dosages to
be taken, the time to take the medication which
includes the day, date and how many times the drug
must be taken in a day. From the information
contained in the form, we will get information
related to the patient's medication adherence while
the patient is outside the primary health center
without asking the patient so that this activity will
not interfere with consultation time and does not
hamper health services. This advice is given because
patients can be routinely controlled according to a
predetermined time but to prevent the increased risk
of hypertension, patients must also be obedient to
take antihypertensive medication.
5 CONCLUSION
1. The description of hypertension in the
Kalideres District Primary Health Center
shows that the highest proportion in
patients with hypertension level I, as
many as 95 people(81.2%).
2. The description of medical adherence on
patients with hypertension in the
Kalideres District Primary Health Center
shows that the proportion of patients with
hypertension who adhered to taking
medicine as many as 70 people (59.8%)
and the proportion of those who did not
adhere to take medication as many as 47
people (40.2%).
3. There is a difference between adherence
to taking medication in the group of
patients with hypertension level I and
hypertension level II
.
Differences of Medical Adherence on the Level I and Level II of Hypertension Patients in Kalideres Sub-District Primary Health Center
Year of 2019
343

6 SUGGESTION
1. It is suggested to primary health center to
make a form of adherence to take
antihypertensive medication. The form
contains information and instructions
about antihypertensive medicine such as
drug dosages to be taken, the time to take
the medication which includes the day,
date and how many times the drug must
be taken in a day. From the information
contained in the form, we will get
information related to the patient's
medication adherence while the patient is
outside the primary health center without
asking the patient so that this activity will
not interfere with consultation time and
does not hamper health services. This
advice is given because patients can be
routinely controlled according to a
predetermined time but to prevent the
increased risk of hypertension, patients
must also be obedient to take anti-
hypertensive medication
2. It is advisable to include family members
in the treatment of patients, especially for
elderly patients in order to increase the
participation of family members in the
treatment of hypertension, so that there
are reminders of the schedule of taking
antihypertensive medication according to
the treatment suggested by health
workers.
3. It is hoped that further researchers will be
able to further develop research on
medication adherence in patients with
hypertension by using other variables
such as knowledge, patient cholesterol
levels, lifestyle or others with different
research methods such as qualitative.
REFERENCES
Adib, M. (2009). Cara Mudah Memahami & Menghindari
Hipertensi, Jantung & Stroke. Yogyakarta: Dianloka
Printika.
Agustina, S., Sari, S. M., & Savita, R. (2014). Faktor-
faktor Yang Berhubungan Dengan Hipertensi Pada
Lansia diatas Umur 65 Tahun. Jurnal Kesehatan
Komunitas, 2.
Aryatiningsih, D. S., & Silaen, J. B. (2016). Hipertensi
Padda Masyarakat di Wilayah Kerja Puskesmas
Harapan Raya Pekanbaru. Jurnal Ipteks Terapan.
Research of Applied Science and Education, 12.
Beata Jankowska-PolańskaIzabella, U., Krzysztof, D., &
Grzegorz, M. (2016). Relationship between patients’
knowledge and medication adherence among patients
with hypertension. Journal Patient Preference and
Adherence.
BPOM. (2006). Pedoman Cara Pembuatan Obat yang
Baik. Jakarta: BPOM.
Bustan, M. . (2007). Epidemiologi Penyakit Tidak
Menular. Jakarta: PT Rineka Cipta.
Carpenito, L. . (2013). Diagnosa Keperawatan : Aplikasi
Pada Praktek Klinik (Terjemahan). Jakarta: EGC.
Casey, A., Benson, H., & O’Neill, B. (2006). Menurunkan
Tekanan Darah. Jakarta: PT Bhuana Ilmu Populer.
Dahlan, S. M. (2013). Besar Sampel dan Cara
Pengambilan Sampel. Jakarta: Salemba Medika.
Departemen Kesehatan RI. (2013). Pedoman Teknis
Penemuan dan Tatalaksana Penyakit Hipertensi.
Jakarta: Direktorat pengendalian penyakit tidak
menular.
Elfindri, Hanita, E., Abidin, Z., Machmud, R., &
Elmiyasna. (2004). Metodologi Penelitian Kesehatan.
Jakarta: Baduose Media.
K Intan, Try; Ernalia, Yanti; Haslinda, L. (2016).
Gambaran Status Gizi Pasien Hipertensi Di Puskesmas
Melur Pekanbaru. Kesehatan, 3 No. 1.
Kemenkes RI. (2018). Hasil Utama Riset Kesehatan
Dasar. Departemen Kesehatan.
Komaling, J. K., Suba, B., & Wongkar, D. (2013).
Hubungan Mengkonsumsi Alkohol dengan Kejadian
Hipertensi Pada Laki-laki di Desa Tompasobaru II
Kecamatan Tompasobaru Kabupaten Minahasa
Selatan. 1.
Kozier. (2010). Buku Ajar Keperawatan Klinis. Jakarta:
EGC.
Liberty, che A., Pariyana, E. R., & Lukman, W. (2017).
No TitlDeterminan Kepatuhan Berobat Pasien
Hipertensi pada Fasilitas Kesehatan Tingkat I. Jurnal
Penelitian Dan Pengembangan Pelayanan Kesehatan,
1.
Masriadi. (2016).
Epidemiologi Penyakit Tidak Menular.
Jakarta: CV Trans Info Media.
McGowan, M. P., & Castelli, W. T. (2001). Menjaga
Kebugaran Jantung. Jakarta: Raja Grafindo.
Morisky, D. . A., Krousel-Wood, A., & M.A. Ward, H.
(2008). Predictive Validity of A Medication Adherence
Measure in an Outpatient Setting. J. Health-Syst.
Pharm.
Muchid, A. (2006). Buku Saku Hipertensi:
Pharmacheutical Care Penyakit Hipertensi. Jakarta:
Depkes RI Ditjen Bina Farmasi Komunitas dan Klinik.
Ningsih, D. L. R. (2017). Faktor-faktor yang
Berhubungan Dengan Kejadian Hipertensi Pada
Pekerja Sektor Informal di Pasar Beringharjo Kota
Yogyakarta.
ICOH 2019 - 1st International Conference on Health
344

Nopitasari, Baiq Leny; Adikusuma, Wirawan; Qiyaam,
Nurul; Fatmala, A. (2018). Pengaruh Kepatuhan dan
Ketepatan Waktu Minum Obat Terhadap Tekanan
Darah Pasien Hipertensi Primer. Ulul Albab, 23, 28–
32.
Palmer, A., & Williams, B. (2007). Tekanan Darah
Tinggi. Jakarta: Erlangga.
Rahmawati, R., & Daniyati, D. (2016). Hubungan
Kebiasan Minum Kopi Terhadap Tingkat Hipertensi.
07, 149–161.
Ramadhan, Adam M; Ibrahim, Arsyik; Utami, A. I.
(2015). Evaluasi Penggunaan Obat Antihipertensi
Pada Pasien Hipertensi Rawat Jalan Di Puskesmas
Sempaja Samarinda. Sains Dan Kesehatan, 1 No. 2.
Sartik, Tjekyan, R. S., & Zulkarnain, M. (2017). Faktor-
faktor Risiko Dan Angka Kejadian Hipertensi Pada
Penduduk Palembang. Jurnal Ilmu Kesehatan
Masyarakat.
Setyanda, Y. O. G., Sulastri, D., & Lestari, Y. (2015).
Hubungan Merokok dengan Kejadian Hipertensi pada
Laki-laki Usia 35-65 Tahun di Kota Padang. Jurnal
Kesehatan Andalas.
Soekidjo, N. (2010). Ilmu Perilaku Kesehatan. Jakarta: PT
Rineka Cipta.
Sugiyono. (2016). Metdologi Penelitian Kesehatan.
Bandung: Alfabeta.
Sutanto. (2010). Cekal (Cegah dan Tangkal) Penyakit
Modern. Yogyakarta: CV Andi Offset.
Taylor, S. . (2006). Health Psychology. Singapore: Mc
Graw Hill Book Company.
Triyanto, E. (2014). Pelayanan Keperawatan Bagi
Penderita Hipertensi Secara Terpadu (I). Yogyakarta:
Graha Ilmu.
Wade, C. (2016). Mengatasi Hipertensi. Bandung: Nuansa
Cendekia.
WHO, W. H. O. (2018). Noncommunicable Disease –
Country Profile 2018.
Differences of Medical Adherence on the Level I and Level II of Hypertension Patients in Kalideres Sub-District Primary Health Center
Year of 2019
345
