
Awarding Pelvic Floor Exercise in Elderly Patients with Urinary
Incontinence
Luci Riani Br Ginting
1
, Kuat Sitepu
2
, Isidorus Jehaman
2
, Miftahul Zannah
2
, and Arfia Ningsih
2
1
Faculty of Public Health, Institut Kesehatan Medistra Lubuk Pakam, Indonesia
2
Faculty of Nursing and Physiotherapy, Institut Kesehatan Medistra Lubuk Pakam, Indonesia
Keywords: Pelvic Floor Exercise, Inkontinensia Urin
Abstract: Changes and degradation in the physical, psychological, social and spiritual well-being of the elderly greatly
affects the health status of the elderly. One of the physical changes in the elderly is urinary incontinence.
The high incidence of urinary incontienence causes the need for physiotherapy with the pelvic floor
excercise method. Pelvic floor exercise method aims to determine the effect of providing pelvic floor
exercise to patients with urinary incontinence. This research is a quasi-experimental study using pre-test and
post-test one group design. Total samples of 15 people were taken by accidental sampling. Stastical analysis
using T-Test. The results obtained p value <α = (0,000 < 0.05)Which means that there is a significant
influence on pelvic floor exercise on patients with urinary incontinence in the elderly at Grandmed Hospital.
Suggestion for future researchers are expected to use a larger number of samples from this study and a
longer reasearch time from this study so that the results obtained are more optimal.
1 INTRODUCTION
According to WHO the age limit of the elderly
(elderly) population group aged 60 years is or more.
WHO data shows that life expectancy in 2000 was
66 years, increased in 2012 to 70 years, and 71 years
in 2013. And the increasing number of elderly
population in 2009 was 7.49% of the total elderly
population. world population, in 2011 became
7.69% and in 2013 increased to 8.1% of the total
population of the elderly population, according to
the WHO Age criteria is 60-74 years. (WHO, 2015).
Data in the United States is estimated that
around 10-12 million adults experience urinary
incontinence. Its severity increases with age and
parity. At the age of 15 years or more the incidence
is 10%, while at the age of 35-65 years it reaches
12%. Prevalence will increase to 16% in women
over 65 years. In multipara there is an incidence of
5%, in women with one child reaching 10% and
increasing to 20% in women with 5 children
(Collein, 2012).
Whereas in Indonesia the high life expectancy
(UHH) is an indicator of the success of achieving
national development in the health sector, since
2004-2015 life expectancy has increased from 68.6
years to 70.8 years and is projected in 2030-2035
life expectancy in Indonesia it will reach 72.2 years
which Indonesia will enter the aging period (aging),
which in 2020 will be estimated that 10% of the
population will be aged 60 years and over, according
to law No. 13 1998 criteria elderly is 60 years and
over ( KEMENKES RI, 2016 ).
Based on the results of records on the Health
Profile of the Province of West Sumatra in 2014, the
percentage of elderly in West Sumatra increased
from 5.45% to 23.9% in 2013, while an increase in
the number of elderly that continues to rise from
year to year is seen from 2007 data as many as
28,557 people, in 2010 as many as 57,625 people
and in 2011 as many as 82,784 people. In 2012-2013
the number of elderly people also increased,
reaching 91,573, in 2014 the number increased to
101,173 people, while in 2015 the number of elderly
increased to 114,305 people, or reached 9%
compared to the previous year (Padang City Health
Office, 2015 ).
Changes and decreases both physically,
psychologically, socially and spiritually which are
experienced by the elderly greatly affect the health
status of the elderly. One of the physical changes
experienced by the elderly that needs attention is the
urinary system. As a result of changes in urinary
function, the elderly experience a disruption in
Ginting, L., Sitepu, K., Jehaman, I., Zannah, M. and Ningsih, A.
Awarding Pelvic Floor Exercise in Elderly Patients with Urinary Incontinence.
DOI: 10.5220/0009471802390246
In Proceedings of the International Conference on Health Informatics and Medical Application Technology (ICHIMAT 2019), pages 239-246
ISBN: 978-989-758-460-2
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
239

controlling urine output which is commonly referred
to as urinary incontinence (Meiner, 2015).
The results of research from several
universities coordinated by the center of aging
studies of Indonesian universities (CAS UI) showed
the emergence of geriatric syndrome which
sequentially in the form of disorders as follows,
among others Nutrition 41.6%, Cognitive 38.4% and
third urinary disorders / urinary incontinence by
27.8%, subsequent immobilization disorders 21.3%
and depression 17.3%.It is estimated that there are
more than 200 million people in the world
experiencing problems in controlling urine
(Elizabeth, 2014).
According to research (Onat, 2014) it is
estimated that 25-35% of all late adults will
experience urinary incontinence during their
lifetime. A survey conducted in various Asian
countries found that the prevalence in several Asian
countries was on average 21.6% (14.8% in women
and 6.8% in men). Compared to the age of
production, in the elderly the prevalence of urinary
incontinence is higher. The prevalence of urinary
incontinence in elderly women is 38% and in men
19%. Urinary incontinence affects individuals of all
ages, although it is most often found among the
elderly, the condition is not a normal consequence of
aging and is often not treatable.
Urinary incontinence was carried out by the
Urology Department of the FK-Airlangga University
Dr. Soetomo on 793 patients, the results of the
incidence of urinary incontinence in men were
3.02% while in women it was 6.79% (Angelita,
2012). In Gorontalo Province, based on data from
the Provincial Health Office in 2013, 2,371 elderly
had been treated at a hospital with urinary
incontinence problems.
Data from epidemiological studies from five
countries shows the incidence of urinary
incontinence in men aged <39 years by 2.4%, and
10.4% in men aged> 60 years, whereas in women
aged <39 years by 7.3% and 19.3 % In women. > 60
years old. The impact of urinary incontinence is
estimated to be 15-35% in the population aged 60
years and over who live in the community with a
female prevalence twice as large as that of men
(Jahromi, 2015).
Continentia conducted a study of the profile of
urinary incontinence in Indonesia in 2008 involving
six teaching hospitals, namely: Jakarta, Surabaya,
Bandung, Semarang, Makassar and Medan.
Obtained the results of the prevalence of urinary
incontinence as much as 13% of 2,765 respondents
with a total population of geriatric (age over 60
years) of 22.2% more than the total adult population
(aged 18-59 years) of 12.0% with the conclusion of
prevalence Urinary incontinence is found to increase
with age (PERKINA, 2012).
Urinary incontinence is a condition in which a
person unconsciously experiences urine leakage both
in small amounts and in large amounts. This can be
experienced by everyone no exception. But
generally the prevalence increases with age,
especially in women.
Another problem related to urinary
incontinence is that sufferers rarely report their
condition to health workers. With reasons of shame
and it is taboo to discuss with others. As a result, this
problem is rarely overcome properly (Potter, 2013).
In general, urinary incontinence is caused by
changes in the anatomy and function of the elderly
urinary organs, obesity (obesity), menopause, old
age, lack of activity and vaginal surgery, decreased
levels of the hormone estrogen in women at
menopause (50 years and over).
Increasing weight and pressure during
pregnancy can cause pelvic floor muscle weakness
due to pressure for nine months. The delivery
process can also make pelvic floor muscles damaged
by muscle stretches and supporting tissues and tear
of the birth canal, thereby increasing the risk of
urinary incontinence (Sankarganesh, Kumar, 2018).
Gender factors play a role in urinary incontinence,
especially in women due to decreased levels of the
hormone estrogen at menopause, there will be a
decrease in vaginal muscle tone and urinary tract
(urethral) muscle, causing urinary incontinence. The
risk of urinary incontinence increases in women with
greater body mass index values, a history of
hysterectomy, urinary infection, and perineal
trauma. Symptoms of incontinence that usually
occurs is urinating when coughing, straining,
laughing, sneezing, running and feeling a sudden
urge to urinate, repeatedly urinating and urinating at
night (Setiati, 2014).
The results of Galih Adhi Isak Setiawan's
research, About the effect of adding faradik
stimulation on pelvic floor exercise to decrease
urinary incontinence frequency on urinary
incontinence stress in Muhammadiyah Yogyakarta
hospital, obtained 0.05 (p <0.05) there was an
influence in decreasing urinary incontinence
frequency from before and after treatment.
Based on a survey conducted at Grandmed
Lubuk Pakam Hospital, the elderly population in the
inpatient room at Grandmed Lubuk Pakam Hospital
in 4 inpatient rooms were 40 elderlyand there are 18
elderly who experience urinary incontinence for 1
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
240
month so the results obtained are the prevalence of
urinary incontinence as much as 45% of 40 elderly
people.
Pelvic floor musculature is composed of several
layers with bony attachments to the pubic bone and
coccyx. The anterior-posterior fibers are oriented
almost horizontally and form the inferior support for
the trunk. Laterally, the tissues blend into a fascial
layer overlying the obturator internus. Both right and
left sides of the muscles contribute fibers to the
perineal body located between the vagina and
rectum. The Structure and action of the muscles of
each layer. That fibers run from anterior-posterior
create a superior force toward the heart while the
more superficial fibers surround the sphincters and
procedure a puckering motion (Kisner, 2016).
Urinary incontinence results from a decrease in
pelvic floor muscle strength that can be caused by
aging. Another cause by extreme stretching of the
pelvic floor tissues in inherent in the process of
labour and vaginal delivery. The pelvic floor
musculature may also be torn or incised during the
birth process. An episiotomy is an incision made in
the perineal body. It is automatically considered a
second-degree laceration according to the following
classification of perineal lacerations (Kisner, 2016).
Episotomy is common occurred in 33% to 51%
of vaginal delivers there is no strong medical
evidence suppoting its use. In fact outcomes with
episotomy are worse in some cases including pain
with intercourse and extension of the episotomy in
particular, the physiotherapy is able to provide
education and support for the patient as she explores
her options.
The physiotherapy intervention used to handle
cases of urinary incontinence is pelvic floor exercise
that aims to increase the strength of the pelvic floor
muscles. This exercise is done in series with the type
of contraction exercises to increase the strength of
the pelvic floor muscles so that it can strengthen the
function of the external sphincter in the bladder, and
make the urethra tightly closed by contracting
relaxes that are carried out continuously or
repeatedly. This exercise is also very effective for
controlling urinary without drugs or surgery (Ma,
Liu, 2019).
Visual aids are critical in teaching patients about
pelvic floor function. Emphasis should be on both
slin/ hammock fibers and orientation of the
musculature. To visualize the fibers that run
anterior-posterior as well as the circumferential
fibers (Kisner, 2016).
From the above background the researcher is
interested in conducting research on the Effect of
Giving pelvic floor exercise to patients with urinary
incontinence in the elderly at Grandmed Lubuk
Pakam Hospital in 2019.
2 RESEARCH METHODS
This research was conducted at the Grandmed
Poly Physiotherapy Hospital, located at Jl Raya
Medan, No.66, Lubuk Pakam. The research was
conducted in February - July 2018. This type of
research is quasi-experimental.
In this study observations and measurements
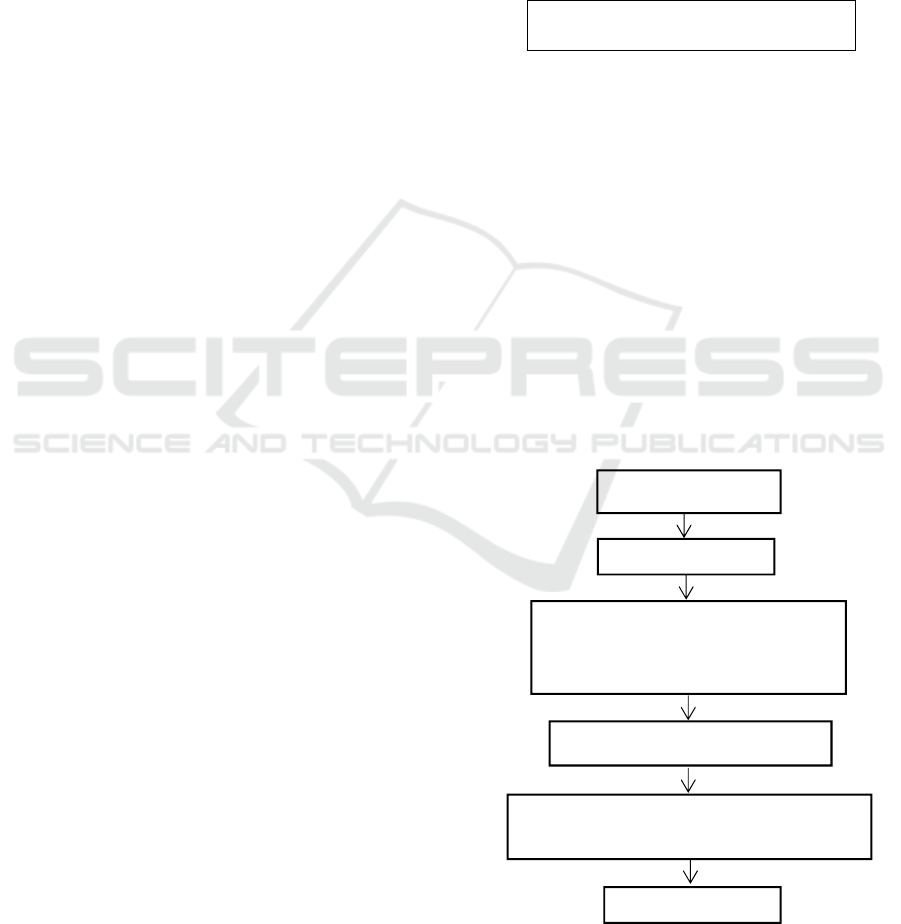
were made before and after treatment to see the
effect of pelvic floor exercise on urinary
incontinence that can be seen on Figure 1.
P1
X P2
Figure 1: Implementation of research activities.
Where P1 is first observation (Pretest) to see
urinary incontinence before pelvic floor exercise in
the elderly, X is the treatment given pelvic floor
exercise and P2 is the second obsevation (posttes) to
determine urinaty incontience after pelvic floor
exercise according to Figure 2 the number of
samples in the study were 15 people who took based
on the inclusion criteria and exclusion criteria.
Inclusion criteria in the study are elderly who
experience urinary incontinence, respondents are
aware and can be actively invited to communicate,
patients use catheters and pampers. While the
Exclusion Criteria are, respondents with impaired
consciousness, respondents resign before pelvic
floor exercise and elderly with heart disease.
Figure 2: Reaserch Implemtation Flow.
Population
Sam
p
el: n=15
Urinary incontinence
measureament with SSI before
pelvic floor exercise
Interventionpelvic floor
i
Urinary incontinence measureament
with SSI after pelvic floor exercise
Data anal
y
sis
Awarding Pelvic Floor Exercise in Elderly Patients with Urinary Incontinence
241

Procedure for implementing the Pelvic Floor
Exercise method
Pelvic floor exercise is a method of exercise on
the pelvic floor muscles that is useful for
strengthening pelvic floor muscles, increasing tone
of pelvic floor muscles, and making the urethra
tightly closed by contracting relaxes that are carried
out continuously or repeatedly. This exercise is also
very effective for controlling urinary incontinence
without drugs or surgery (Rocha, Carvalho, Natal,
2018). Objectives 1) strengthen the muscles that
support the bladder and urethra, 2) help maintain
muscle control for urination. The therapy starts
from:
Patient preparation, explain to the patient
the procedures and goals of Pelvic Floor
Exercise intervention, position the patient
as comfortable as possible.
Equipment preparation place or bad must
not be too low or high, and must not be too
soft, there is a place for training (clean and
safe walls).
Therapy management perform a bridge.
bridge (bridge). Start by lying down
supine and bend both knees, and give a fist-
sized gap between the legs. After that,
tighten the lower abdominal muscles and
raise the pelvis from the floor. Stop when
the shoulders and knees form a straight
line. Hold for 8 seconds and slowly return
your pelvis to the floor. Try not to turn your
head when the pelvis is lifted because it can
strain your neck. 2) Practice wall squats.
Lean against the wall, and open your feet
hip-width apart. Take a deep breath and
tighten your pelvic floor muscles. Then,
lower your back to rub against the wall into
a squat position (like sitting in a chair).
Hold for 10 seconds, then stand back up, 3)
Do a "dead bug crunch" Lie on your back
on the floor, bend your knees and soles of
your feet at knee height. Extend both arms
firmly to the ceiling. Breathe deeply,
tighten muscles pelvic floor, and straighten
your left hand and left leg in the opposite
direction, return to the starting position, and
repeat with the right side of your body.
Pelvic Duration applied: 1) Intensity:
Perform 3 repetitions, Duration 15 minutes,
Frequency 2 times a week for 1 month of
research.
Measurement Method, using structured
measurements that defines what will be
observed through a careful planning (Nursalam,
2011). Observations were made before (pre-test)
and after (post-test) pelvic floor exercise for
patients suffering from urinary incontinence.
Measurement using the Sandvix Saverity Index
(SSI) Scale. SSI consists of two questions where
the results of the study regarding urinary
incontinence are obtained by multiplying the
score of the first question answer by the score of
the second question,
Skor 1-2 : mild incontinence
Skor 3-5 :moderate incontinence
Skor 6-8 :severe incontinence
Skor 12 :very heavy
3 RESULT
Respondents in this study amounted to 15
people who suffer from urinary incontinence who
have fulfilled the requirements to become
respondents with the provisions that have been
made. Characteristics of respondents in this study
based on age and gender.
The number of respondents based on age, aged
60-65 as many as 10 people (66.7%), aged 66-70
amounted to 3 people (20.0%) while in 71-74 aged 2
people (13.3%). While based on gender, there are 7
men (46.7%), while there are 8 women (53.3%).
Based on the measurement results of urinary
incontinence with SSI Before being given Pelvic
Floor Exercise Interventions an average value of 5.8
(severe incontinence) was obtained, while the results
of measuring urinary incontinence with SSI after
being given Pelvic Floor Exercise obtained an
average value of 2.5 (incontinence) is) Statistical test
results obtained p value α < (0,000 <0.005), it can be
concluded that there is a significant influence
between urinary incontinence before and after being
treated with pelvic floor exercise for patients with
urinary incontinence in the elderly at Grandmed
Lubuk Pakam Hospital.
4 DISCUSSION
Based on the results of research conducted on 15
patients aged at most aged 60-65 years, as many as
10 people (66.7%), while at the age of 66-70 years
as many as 3 people (20.0%), and at least at the age
of 71-65 74 years as many as 2 people (13.3%). This
is consistent with the existing theory that the
problem of urinary incontinence from changes that
occur at that age, changes in the urinary system or
the urinary system potentially have a significant
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
242

level of importance. Urinary incontinence problems
are not caused directly by the aging process, triggers
urinary incontinence in the elderly is a condition that
often occurs in old age combined with age-related
changes in the urinary system (Stanley, 2010).
Patients often consume certain drugs because of
their illness. These medications can be one of the
causes of loss of bladder control in older people. If
this condition occurs, the discontinuation or
replacement of the drug if possible, a decrease in the
dose or modification of the drug administration
schedule (Setiati, 2007)
Based on the results of research conducted on 15
patients the majority of female sex characteristics
are 8 people (53.3%) and 7 people (46.7%) men.
Urinary incontinence can be caused by
complications from urinary tract infections, loss of
sphincter control or sudden changes in abdominal
pressure. Incontinence can be permanent for
example in spinal cord trauma or temporary in
pregnant women with a pelvic floor
structureweakness can result in urinary incontinence.
Although urine incontinence can occur in patients of
various ages, loss of urinary control is a problem for
the elderly (Engla, 2017).
Weight gain and pressure during pregnancy can
cause pelvic floor muscle weakness due to pressure
for nine months. The growing fetus places added
stress on postural muscles as the center of gravity
shifts forward and upward and the spine shifts to
compensate and maintain stability. In addition, after
delivery, activities involving holding and caring for
the baby stress postural muscles. Muscles that
require emphasis for strengthening and stretching
are listed. General exercise descriptions are listed in
respective. Subsequent sections describe adaptations
of exercises specific for the pregnant woman. The
delivery process can also make pelvic floor muscles
damaged due to muscle strain and supporting tissues
and tear of the birth canal so that it can increase the
risk of urinary incontinence. With a decrease in
estrogen levels in women at the age of menopause
(50 years and over), there will be a decrease in the
tone of vaginal muscles and urinary tract muscles
(urethra) (Setiati, 2007)
Urinary incontinence problems are not caused
directly by the aging process, triggers urinary
incontinence in the elderly is a condition that often
occurs in old age combined with age-related changes
in the urinary system. Flexibility and stretching
exercises are implemented with caution. Remember
that connective tissues and supporting joint
structures are at increased risk of injury from
forceful stresses during pregnancy and the
immediate postpartum period because of hormonal
changes (Stanley, 2010).
Based on the results of research conducted on
15 people on the measurement of the value of the
SSI before giving pelvic floor exercise which has a
value of = 5.53 and SD = 2.031.
Changes that occur in the urinary system are a
decrease in vaginal muscle tone and urinary tract
(urethral) muscle caused by a decrease in the
hormone estrogen, causing urinary incontinence, the
muscles become weak, the capacity decreases to 200
ml or causes the frequency of BAK to increase.
Impaired sphincter function causes the bladder to
leak when coughing or sneezing, it can also be
caused by abnormalities in the area around the
urinary tract, disturbed cerebral function and
resulting in bladder contractions, urinary discharge
occurs with dilation of the bladder, a lot of urine in
the bladder to excessive capacity (Brunner, 2010,).
As we get older, there are some changes in the
anatomy and function of the urinary organs, namely:
weakening of the pelvic floor muscles due to
multiple pregnancies, vaginal delivery (especially
long process), heavy lifting, obesity, lack of
hormone replacement at menopause, habits incorrect
straining, stroke, enlarged prostate gland, etc. (Ellen,
2017).
From research conducted by Arnold, et al
(2009) based on the type of urinary incontinence, the
incidence of Urinary Stress Incontinence was
58.82%, Urge Incontinence Urine was 11.77% and
Mixed Urinary Incontinence was 29.41%. There are
three most types of urinary incontinence in women,
namely stress urinary incontinence, urge urinary
incontinence and urinary mixed incontinence. These
three types can be evaluated through history taking
and simple clinical judgment.
Urinary incontinence can be caused by
complications from urinary tract infections, loss of
sphincter control or occurrence abdominal pressure
changes suddenly. Incontinence can be permanent,
for example in spinal cord trauma or temporary in
pregnant women with weak pelvic floor structures
can result in urinary incontinence. (Engla, 2017).
Successful strengthening is unlikely without this
educational component in fact intructing women in
pelvic floor exrecises by verbal of written instruction
alone caused increased pressure to the appropriate
superiorly directed force. Women who have never
been pregnant may also present with pelvic floor
dysfunction. Excessive straining because of chronic
constipation, smoking, chronic cough, obesity, and
hysterectomy can contribute to these impairments in
any woman. The role of estrogen in the development
of incontinence is still unclear, with some studies
citing estrogen depletion as a risk factor and others
that found a connection between incontinence and
Awarding Pelvic Floor Exercise in Elderly Patients with Urinary Incontinence
243

estrogen replacement therapy. High caffeine intake
(more than 400 mg/day) is a specific risk factor for
urge incontinence (Kisner, 2016).
The use of exercise and biofeedback, including
surface musculosceletal for treatment of pelvic floor
dysfunction in a female population is well
supported. Musculo can show by electromyography
allows for immediate visual and/or auditory
feedback to the patient, enhancing motor learning
and proprioceptive improvements. It is particularly
invaluable for pelvic floor re-education owing to
lack of knowledge of the muscles’existence, let
alone their function and importance. Specific
exercises to address pelvic floor impairments are
listed in the exercise (Kisner, 2016).
This is in line with a study conducted by Galih in
2015 in his research on the Effect of Pelvic Floor
Exercise with a decrease in Urinary Continuation
conducted 5 repetitions, 3 times a week in the result
of statistical test p-value = 0.005 (p <0.05) which it
means that there is an effect of giving Pelvic Floor
Exercise on Patients with Urinary Incontinence.
Based on the results of research conducted on 15
people on the measurement of the value of SSI after
giving pelvic floor exercise which has a value of
Mean = 3.60 and SD = 1.882.
Sacroiliac pain is localized to the posterior pelvis
and is described as stabbing deep into the buttocks
distal and lateral to L5/S1. Pain may radiate into the
posterior thigh or knee but not into the foot.
Symptoms include pain with prolonged sitting,
standing or walking, climbing stairs, turning in bed,
unilateral standing, or torsion activities. Symptoms
may not be relieved by rest and frequently worsen
with activity. Pubic symphysis dysfunction may
occur alone or in combination with sacroiliac
symptoms, and includes significant tenderness to
palpation at the symphysis, radiating pain into the
groin and medial thigh, and pain with weight
bearing. In addition, excessive separation and
translation of the bone may occur. One study
reported a four times greater incidence of posterior
pelvic pain than low back pain in pregnant women.
Pelvic floor exercise is one of a variety of therapies
used in the management of urinary incontinence.
Pelvic floor exercise is a pelvic floor exercises or
exercises that are useful to strengthen the pelvic
floor muscles, increase the tone of the pelvic floor
muscles, and make the urethra closed tightly by
contracting relaxes that are carried out continuously
or repeatedly (Klausner, 2003).
This exercise is also very effective for
controlling urinary incontinence without drugs or
surgery. Pelvic floor exercise is an easy exercise to
help increase muscle strength and bladder. If done
properly and regularly, this exercise can build and
strengthen pelvic floor muscles to help hold urine
and feces (Jahromi, Talebizadeh, Mirzaei, 2015.
Indications Men and women who have
incontinence problems (unable to resist urination),
Women who have experienced menopause to
maintain pelvic muscle strength from decreased
estrogen levels, Women who experience uterine
prolapse (uterine descent) due to weakening of the
pelvic floor muscles, also to women who experience
sexual problems.
There are various exercises that you can try, and
one of them is a bridge. Start by lying on your back
and bend your knees, and give a fist-sized gap
between your legs. After that, tighten the lower
abdominal muscles and rise the pelvis from the
floor. Stop when the shoulders and knees form a
straight line. Hold for 8 seconds and slowly return
your pelvis to the floor. Try not to turn your head
when the pelvis is lifted because it can strain your
neck. Exercise must be modified so as not to
aggravate the condition. Avoid exercises that require
single-leg weight bearing and excessive hip
abduction or hyperextension. Teach the patient to
activate the pelvic floor and transverse abdominals
when transitioning from one position to another in
order to stabilize the pelvis.
Based on the analysis of the Paired T-Test Test,
the results obtained are Pretest and Posttes Mean =
1.933, with a standard deviation = 0.594. The
analysis results obtained p value = 0,000 (p <0.05)
which means there is
Significant influence between the value of SSI
before and after pelvic floor exercise is given to
patients with urinary incontinence and this
intervention is good to be applied by
physiotherapists in patients with urinary
incontinence for the development of physiotherapy
interventions.
Assumptions according to the authors of this
study that pelvic floor exercise is very effective in
patients with urinary incontinence because this
technique can strengthen pelvic floor muscles by
exercising pelvic floor muscles by contracting and
relaxing that is done repeatedly so that it can reduce
urinary incontinence caused by pelvic floor muscle
weakness. Daily activities should be adapted to
minimize asymmetrical forces acting on the trunk
and pelvis. For example, getting into a car is done by
sitting down first, then pivoting both legs and the
trunk into the car, keeping the knees together; side-
lying is made more symmetrical by placing a pillow
between the knees and under the abdomen, and
sexual positions are altered to avoid full range of hip
abduction. Single-leg weight bearing, excessive
abduction and sitting on very soft surfaces should be
avoided. In addition, caution patients to avoid
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
244

climbing more than one step at a time, swinging one
leg out of bed at a time when getting up, or crossing
the legs when sitting.
When doing Pelvic floor exercise neurological
adaptation, structural adaptation and metabolic
adaptation will occur. Neurological adaptations
occur by activating motor units that innervate
nerves. Structural Adaptation is associated with
muscle hypertension or an increase in muscle size.
As you know, muscle strength is directly
proportional to an increase in muscle size. Muscle
hypertrophy results in an increase in the number and
size of myofibrils, each of which is formed by
contractile units, the sarcomer. Sarcomere
hypertrophy results in density in myofibrils. The
parallel growth of myofibril causes a tension level
(increased tension). This is what causes muscle
strength. Whereas in metabolic adaptation there are
three complex enzymes, namely: phosphocreatine
ATP complex, glycolysis / glycogenolosis complex
and lypolysis complex. This enzyme is very
influential during training. At the time of exercise
these three enzymes have increased so as to increase
muscle strength. All of these have an impact on the
strength of increasing pelvic floor muscle strength
(Radzimińska, Strączyńska, Weber-Rajek, 2018)
Pelvic floor exercise interventions are very
effective to help patients with urinary incontinence.
From an economic point of view this exercise can
also help because pelvic floor exercise training can
not only be done in hospitals but exercises can be
done at home as a home program. Developing the
ability to relax requires awareness of stress and
muscle tension. Techniques of conscious relaxation
allow the individual to control and cope with a
variety of imposed stresses by being mentally alert
to the task at hand while relaxing tense muscles that
are superfluous to the activity. This is particularly
important during labor and delivery when there are
times that the woman should relax and allow the
physiologic processes to occur without excessive
tension in unrelated muscles. Additional relaxation
techniques for managing stress. The following
guidelines are most effective for the pregnant
woman if consistently practiced in preparation for
labor and delivery.
5 CONCLUSION
Urinary incontinence in the elderly at Gransmed
Hospital before most muscle trainingin the moderate
category, after pelvic floor exercise is in the light
category, so there is
influence of pelvic floor exercise methods in
decreasing urinary incontinence on. Incontinence is
a condition in which there is accidental loss of urine
through the urethral meatus which can result in
social problems and observable hygiene. Pelvic floor
exercises with pelvic floor exercise can improve
urination with less risk. Health workers have an
important role in helping clients with urinary
incontinence to restore the function of the urinary
system. In addition, health workers can control the
activities and eating patterns of respondents.
REFERENCES
Dinas Kesehatan Kota Padang. Profil Kesehatan Kota
Padang Tahun 2015. Padang: Dinas Kesehatan Kota
Padang; 2016
Elizabeth. (2014). Analisis Praktek Klinik Keperawatan
Gerontik Kesehatan Masyarakat Perkotaan pada
Kakek D dengan Inkontinensia Urine di PTWS Budi
Mulia 01 Cipayung. FIK UI: Karya Ilmiah Akhir Ners
Ellen. (2017). Intisari Fisioterapi Buku Praktik Klinik.
Jakarta: EGC.
Engla. (2017). Efektivitas Inisiasi Bladder Training
Terhadap Inkontinensia Urin pada Pasien Stroke non
Hemoragik yang Terpasang Kateter di ruang
Neurologi RSUD Raden Mattaher Jambi, diakses
tanggal 20 januari 2018.
Foxman. (2014). Urinary Tract Infection Syndromes:
Occurrence, Recurrence, Bacteriology, Risk Factors,
and Disease Burden. Epidemiology of UTI
Syndromes, 1, 1-13. doi:10.1016/j.idc.2013.09.003.
Jahromi, Talebizadeh, Mirzaei, 2015. The Effect of Pelvic
Muscle Exercises on Urinary Incontinency and Self-
Esteem of Elderly FemalesWithStress Urinary
Incontinency. Global Journal of Health Science.Vol. 7,
No. 2; 2015.
Jahromi. (2015). The Effect of Pelvic Muscle Exercises on
Urineary Incontinence and Self-Esteem of Elderly
Females With Stress Urineary Incontinency, 2013.
Global Journal of Health Science, Vol 7. No.2.
Kementerian Kesehatan Republik Indonesia. Profil
Kesehatan Indonesia (2015). Jakarta: Kementrian
Kesehatan Indonesia; 2016.
Ma, Liu, 2019. Effectiveness of electrical stimulation
combined with pelvic floor muscle training on
postpartum urinary incontinence. Study Protocol
Systematic Review.
Meiner. (2015). Gerontologic Nursing 5th edition. USA:
Elsevier.
Onat, dkk. (2014). Relationship Between Urinary
Incontinence and Quality of Life in Elderl.
Radzimińska, Strączyńska , Weber-Rajek, 2018. The
impact of pelvic floor muscle training on the quality of
life of women with urinary incontinence: a systematic
literature review. Clinical Interventions in Aging
Awarding Pelvic Floor Exercise in Elderly Patients with Urinary Incontinence
245

Rocha, Carvalho, Natal, 2018. Evaluation of the pelvic
floor muscles training in older women with urinary
incontinence: a systematic review.
Sankarganesh, Kumar, 2018. Interferential Therapy
Versus Pelvic Floor Exercise for the Management
ofStress Urinary Incontinence in Women. Journal of
Physiotherapy Research.
Setiati (2014). Buku ajar ilmu penyakit dalam jilid I. VI.
Jakarta: InternaPublishing; 2014:1132-53.
World Health Organization, 2015. Global life expectancy
reaches new heights but 21 million face premature
death this year, warns WHO. Available at
http://www.who.int/whr/1998/media_centre/press_rele
ase/en/index3.html diakses pada tanggal 20 juli 2015
pukul 11.00 WIBSuhardjo, 2005. Perencanaan Pangan
dan Gizi. Bumi Aksara, Jakarta.
.
ICHIMAT 2019 - International Conference on Health Informatics and Medical Application Technology
246
