
Effect of Pre-incisional Ultrasound-guided Quadratus Lumborum
Block on Perioperative Analgesia and Inflammatory Responses in
Transperitoneal Laparoscopic Nephrectomy: A Single-blinded,
Randomised Control Trial
Dita Aditianingsih
1
, Besthadi Sukmono
1
, Erika Sasha Adiwongso
1
and Chaidir Arif Mochtar
2
1
Department of Anesthesiology and Intensive Care, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
2
Department of Urology, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
Keywords: Quadratus Lumborum Block, Laparoscopic Nephrectomy, Pre-incisional.
Abstract: A Quadratus lumborum (QL) block produces an effective lower abdominal surgery perioperative analgesia,
which has been reported to improve perioperative pain intensity and inflammatory responses. This prospective
randomised-control study evaluates the efficacy of a pre-incisional ultrasound-guided QL block in providing
perioperative analgesia following a transperitoneal laparoscopic nephrectomy. Forty-four adult patients were
randomly assigned into the control group or QL block group. Intraoperative fentanyl, post-operative
Numerical Rating Scale (NRS) at rest and during movement and additional tramadol in the first 24 hours were
recorded. Blood samples for interleukin-6 (IL-6) and hemodynamic profiles were recorded after anaesthesia
induction, after two hours of surgery and two hours post-operation. The QL block group had lower
intraoperative fentanyl (P < 0.05), lower post-operative NRS at rest and during movement (P < 0.001), lower
IL-6 level (P < 0.05) and lower additional post-operative tramadol demand with a relative risk of 3.00 (1.43–
6.29, P < 0.05). The intraoperative hemodynamic profiles and after-surgery were significantly changed,
compared to the baseline in the control group (P < 0.001), while the QL block group showed more stable
profiles (P > 0.05). The pre-incisional QL block with 0.25% bupivacaine reduced the need for intraoperative
opioid, showed more stable intraoperative hemodynamic changes and lowered inflammatory response, post-
operative pain and the need for additional opioids following transperitoneal laparoscopic nephrectomy.
1 BACKGROUND
Laparoscopic living donor nephrectomy (LLDN) is
the preferred method for kidney donation that is
routinely performed under general anaesthesia
(Hayden and Cowman, 2011). Several studies have
reported that solely using general anaesthesia leads to
a risk factor of developing greater acute post-
operative pain and persistent pain one year after the
surgery. The higher doses of intravenous opioids have
the potential to increase post-operative hyperalgesia,
a higher pain score and additional opioid demands
(Barreveld et al., 2013; Richebe et al., 2013; Méleine
et al., 2012).
Pre-incisional block analgesia is administered
before surgical manipulation to provide analgesia
during and after surgery. The approach aims to
prevent intraoperative pain by activating the
excessive release of cytokines as the inflammatory
response because it is associated with post-operative
morbidity (De Oliviera et al., 2011).
Our study aimed to evaluate the efficacy of pre-
incisional bilateral Quadratus lumborum (QL) block
in reducing intraoperative opioid consumption as the
primary outcome, when compared with a non-
receiving pre-incisional QL block on patient who
underwent LLDN. Secondary outcomes were the
inflammatory response of interleukin-6 (IL-6) and
early post-operative pain intensity.
2 METHOD
2.1 Study Design
This was a single-blinded, prospective, randomised
control study that involved two groups of adult
patients who underwent transperitoneal laparoscopic
26
Aditianingsih, D., Sukmono, B., Adiwongso, E. and Mochtar, C.
Effect of Pre-incisional Ultrasound-guided Quadratus Lumborum Block on Perioperative Analgesia and Inflammatory Responses in Transperitoneal Laparoscopic Nephrectomy: A
Single-blinded, Randomised Control Trial.
DOI: 10.5220/0009387900260032
In Proceedings of the 4th Annual International Conference and Exhibition on Indonesian Medical Education and Research Institute (The 4th ICE on IMERI 2019), pages 26-32
ISBN: 978-989-758-433-6
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

donor nephrectomy under general anaesthesia and
kidney extraction via a Pfannenstiel incision. This
study was part of the clinical trial approved by the
university and hospital Ethics Committee of Medical
Research on June 19
th
, 2017 (protocol number 17-06-
0619), and registered on ClinicalTrials.gov
(identification number: NCT03879980). We
conducted the study between March 2019 and May
2019 and followed good clinical practice guidelines.
2.2 Sample Size
A preliminary study estimated intraoperative fentanyl
consumption was 305 µg (SD 79.7) on the QL block
group and 435 µg (SD 159.9) on the control group.
Based on opioid consumption that was lower in QL
block with a combined SD of 97.6, we calculated a
sample size of 20 in each group could be given 90%
power to detect a difference of 100 µg fentanyl
between the groups with ⍺ = 0.05. We recruited a total
of 44 patients to anticipate missing data or dropouts.
2.3 Research Protocol
Forty-four healthy patients with American Society of
Anesthesiologists (ASA) classification I or II gave
written consent to participate and were randomly
allocated into either a QL block group or a control
(non-QL block) group. Randomisation used blocks of
4 into 2 groups using a list of random numbers and
was performed by sealed envelopes. The surgeries
were performed by 3 urology surgeon consultants
with comparable distributions. Patients and principal
investigators were blinded to group allocation.
Patients who had a body mass index (BMI) >30, age
<18 or >65 years old, chronic use of analgesics or
anti-inflammatory drugs, neuropathy, allergy to local
anaesthetic, surgery <4 or >6 hours and/or duration of
anaesthesia <5 or >7 hours were excluded. All
patients received midazolam 2 mg IV and ranitidine
50 mg IV as premedication. Monitoring of heart rate,
electrocardiography, non-invasive blood pressure,
pulse oxygen saturation and end-tidal carbon dioxide
was conducted. Anesthesia was induced with propofol
1–2 mg/kg IV and fentanyl 1 µg/kg IV, and intubation
was facilitated with atracurium 0.5 mg/kg IV.
For the QL block group, after anaesthesia
induction, the anaesthesiologist consultant performed
the ultrasound-guided lateral QL block (type I) before
the surgical incision. The patients were in the semi-
lateral supine position to present the side to be
blocked. Using GE LOGIQ
P7 (GE Healthcare,
Chicago, Illinois), and 1–6 MHz convex transducer
placed in the transverse plane above the iliac crest at
the level of the umbilicus, a Stimuplex
®
(BBraun,
Germany) 20G 100-mm needle was advanced in the
anteroposterior direction toward the junction of the
tapered abdominal muscle layer and QL muscle, and
20 mL of 0.25% bupivacaine was deposited in the
anterolateral border of QL muscle at the junction
where the transversalis fascia reaches outside the
anterior layer of transversalis fascia. The lateral
approach QL blocks were performed on both sides of
patients, and the total amount of bupivacaine was 100
mg for each patient (Figure 1).
Figure 1: QL type I block technique. The arrow represents
the needle tip on lateral border of the QL muscle. TAP,
transversus abdominis plane; QL quadratus lumborum.
General anaesthesia was maintained using
sevoflurane with end-tidal sevoflurane (ETS) target of
1.5–2% using the Aisys C2 monitor (GE Healthcare,
Chicago, Illinois) to keep the bispectral index (BIS
,
Covidien, Minneapolis) in the range between 40 and
50, and maintenance of atracurium 0.005 mg/kg/min
IV to achieve train of four (TOF) between 0.15 and
0.25 (TOF-Watch, Organon, Ireland) intraoperatively.
Both groups received fentanyl boluses 1 µg/kg IV if
their heart rate or blood pressure increased ≥ 20%
while BIS was 40–50, and the TOF range was 0.15–
0.25; this was assessed by the anaesthesiologist as the
pain response during the surgical stimulations. Venous
blood samples were collected from brachial veins at the
time: before the anaesthesia induction as the baseline,
two hours of surgical stimulation and gas insufflation
intraoperatively and two hours after recovery from
anaesthesia. Inflammatory response IL-6 was analysed
by the ELISA method (Quantikine, R&D system,
USA) following the manufacturer’s instructions, and
every sample was run in duplicates. Perioperative
hemodynamic profiles were represented by heart rate,
systolic pressure, diastolic pressure and mean arterial
pressure and were recorded using the Philips IntelliVue
MP70 monitor (Philips Healthcare, Amsterdam,
Netherlands) at the same time as blood samples were
collected.
All patients received combination neostigmine
1.5–2.5 mg IV (0.03–0.04 mg/kg) and atropine 0.5
mg IV when the TOF ratio was 0.4–0.9 to reverse
neuromuscular blockade post-operatively, and they
were extubated after confirming recovery of
Effect of Pre-incisional Ultrasound-guided Quadratus Lumborum Block on Perioperative Analgesia and Inflammatory Responses in
Transperitoneal Laparoscopic Nephrectomy: A Single-blinded, Randomised Control Trial
27
awareness. Both groups immediately received basic
post-operative analgesia regimen paracetamol 1 gr IV
8
th
hourly. A combination of omeprazole 20 mg IV
and ondansetron 4 mg IV 8
th
hourly was given to
prevent post-operative nausea and vomiting (PONV).
The Numerical Rating Scale (NRS) was observed
between two and 24 hours after the surgery. During
the observation, when the NRS began to increase to
>3 at rest, the intermittent tramadol 50 mg IV boluses
were given 8
th
hourly. If the NRS persisted >3, the
intermittent tramadol 50 mg IV boluses were
administered more frequently up to 4
th
hourly. If the
pain relief was still inadequate after increasing
tramadol boluses, the extra fentanyl 1 µg/kg IV boluses
were given every 15 to 30 minutes until the NRS ≤3.
The analgesic effect of the intraoperative QL
block and control groups was evaluated by measuring
intraoperative fentanyl consumption as the primary
outcome. Intraoperative fentanyl consumption was
recorded as total consumption in µg and calculated
into mean consumption per hour in µg/kg/h, based on
the influence of the patients’ body weight and the
duration of surgery to the given dose of fentanyl
boluses. Secondary outcomes were hemodynamic
profiles, perioperative inflammation response of IL-
6, immediate pain level at rest and during movement
(coughing) by measuring NRS from 0 = no pain to
10 = worst pain at two hours and 24 hours after
anaesthesia recovery. All patients received the NRS
information during their preoperative visits and
repeated explanations during the pain service team
visit after their surgery. The additional opioid
administration during the first 24 hours after surgery
was also recorded.
The research assistant was not involved in the
patient care that was randomly assigned to the
patients. The anaesthesiologist consultant who
performed the QL block was aware of the
randomisation. Each patient, the intraoperative
anaesthesiologist, the pain service team and the
nurses were blind to group allocation. The primary
investigator received the randomisation numbers
after all measurements and calculations of the patients
had been entered into the database collections.
Statistical analyses were performed using the
Statistical Package for the Social Sciences (SPSS)
version 20 (IBM Corp, Armonk, NY) application.
Patient characteristics were presented in tabular form
to assess data distribution. Numerical data were
analysed using the Mann-Whitney U test or estimated
as log-normal distributed, then the comparison
between the groups were analysed with an unpaired t-
test and post hoc analysis with the generalised linear
model (GLM) in log-transformed data. A comparison
with the baseline in each group was analysed with
repeated ANOVA. Categorical data were tested with
the Chi-square test. Data were presented as means ±
standard deviation (SD), or median (range), or mean
of log-transformed data (minimum–maximum) and
95% confidence intervals.
3 RESULTS
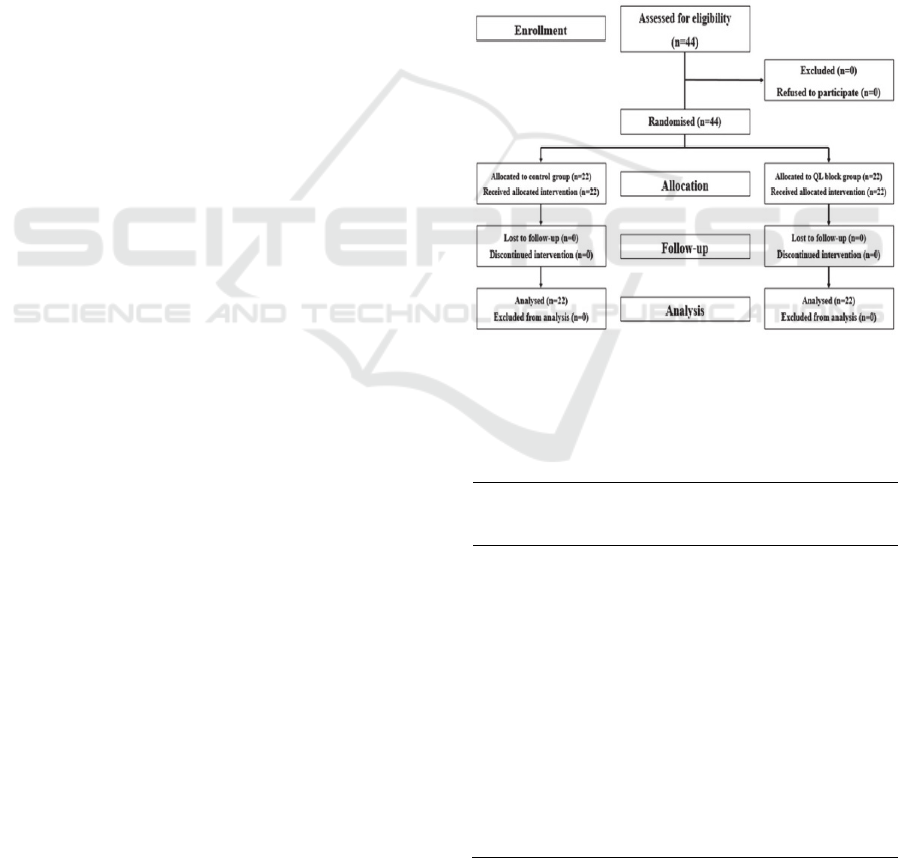
The study CONSORT flowchart shows 44 patients
were enrolled, randomly allocated into QL block group
(22 patients) and control group (22 patients) and
analysed (Figure 2). The baseline characteristics of
both groups were comparable, except that there were
more male subjects in the control group (Table 1).
Figure 2: CONSORT flowchart.
Table 1: Baseline characteristics: Categorical data are
presented as percentage, numerical data are presented as
mean ± SD, median (minimum–maximum). QL, quadratus
lumborum.
Variable
Control group
(n=22)
QL block
group
(n=22)
Gender
Male (%) 17 (77) 11(50)
Female (%) 5 (28) 11(50)
Age (years) 31 (25–54) 32 (21–63)
Weight (kg) 65.46 ± 9.40 62.79 ± 13.34
Height (cm) 162.68 ± 7.82 161.66 ± 9.34
Body mass index
(kg/m
2
)
24.51 ± 3.20 24.20 ± 2.90
Duration of
surgery (minutes)
273 (258–288) 270 (210–360)
Pneumoperitoneum
pressure (mmHg)
10.00 (8–14) 12.00 (10–14)
Duration of
anaesthesia
(minutes)
295 (245–385) 300 (230–390)
The 4th ICE on IMERI 2019 - The annual International Conference and Exhibition on Indonesian Medical Education and Research Institute
28
The mean and total intraoperative fentanyl
consumption of the QL block group were
significantly less than the control group (Table 2).
The NRS scores at two hours after recovery, at rest
and during movement were significantly lower in the
QL block group (P < 0.001), compared to the control
group. The NRS scores at 24 hours after QL block
were performed at rest and during movement and
were significantly lower (P < 0.001), compared to the
control group. The additional intravenous tramadol
IV was needed less in the QL block group, as
compared to the control group (P < 0.05) (Table 2).
The control group needed more additional
intravenous tramadol within 24 hours, with the
relative risk of this being three times higher than the
QL block group [RR 3.00 (1.43–6.29), P < 0.05].
None of the patients needed additional fentanyl
boluses during the observation.
The trends of perioperative hemodynamic profiles
and IL-6 levels as the inflammatory response during
and after surgery showed significant group
differences (Table 3). The QL block group showed
significantly higher systolic (P < 0.001), diastolic
(P = 0.002), mean arterial pressure (P < 0.001) and
heart rate (P = 0.037) intraoperatively, but lower
values after surgery, compared to the control group.
The perioperative hemodynamic profiles were
significantly changing during and after surgery,
compared to the baseline (P < 0.001) in the control
group, while the QL block group showed more stable
profiles (P > 0.05), except in terms of the heart rate.
In addition, we analysed the hemodynamic
difference between time points (Table 4). The control
group showed significant higher systolic (P < 0.001),
diastolic (P = 0.005) and mean arterial pressure
(P = 0.001) changes between intraoperative and post-
operative time points, compared to QL block group;
while the QL block group showed significant higher
Table 2: Patient’s perioperative data: Numerical data were analysed with unpaired t-test and presented as mean ± SD or with
Mann-Whitney U test and presented as median (maximum–minimum); categorical data were analysed with the Chi-square
test and presented as a number of patients (percentage), P < 0.05 is significant.
Control group
(n=22)
QL Block group
(n=22)
P-value
Mean intraoperative fentanyl consumption (µg/kg/h) 1.46 ± 0.28 1.16 ± 0.36 0.002
Total intraoperative fentanyl consumption (µg) 430 ± 105.08 322 ± 89.36 0.016
Numerical Rating Scale (NRS)
2 hours after recovery at rest 1.00 (0.00 – 3.00) 0.00 (0.00 – 2.00) < 0.001
2 hours after recovery in movement 2.00 (1.00 – 4.00) 1.00 (0.00 – 3.00) < 0.001
24 hours at rest 2.00 (1.00 – 4.00) 1.00 (0.00 – 3.00) < 0.001
24 hours in movement 4.00 (2.00 – 5.00) 2.00 (1.00 – 4.00) < 0.001
Additional intravenous tramadol in 24 hours (n%)
Yes 15 (34) 9 (20) 0.001
No 7 (15) 13 (30)
Table 3: Perioperative hemodynamic response.
Parameters Control group (n=22) P value† QL block group (n=22) P
value†
P
value*
CI 95%
Systolic blood pressure (mmHg)
baseline 100.72 (94.49–106.95) 112.16 (106.07–118.24) 0.05 11.44 (2.79–20.09)
intraoperative 106.76 (102.09–111.43) <0.001 115.89 (109.70–122.09) 0.326 0.016 9.13 (1.77–16.50)
post-operative 118.84 (112.91–124.77)
111.42 (105.30–117.54) 0.082 -7.42 (-15.82–0.98)
Diastolic blood pressure (mmHg)
baseline 59.84 (54.83–64.85) 70.26 (66.53–73.99) 0.05 10.42 (3.98–16.86)
intraoperative 63.00 (59.40–66.60) <0.001 70.89 (65.69–76.10) 0.437 0.010 2.94 (1.96–13.83)
post-operative 70.40 (65.68–75.12)
66.68 (61.69–71.68) 0.273 -3.72 (-10.46–3.03)
Mean arterial pressure (mmHg)
baseline 73.47 (68.34–78.59) 84.23 (80.48–87.98) 0.05 10.76 (4.20–17.32)
intraoperative 77.59 (73.97–81.20) <0.001 85.89 (81.02–90.76) 0.410 0.006 8.31 (2.56–14.06)
post-operative 86.55 (81.82–91.27)
81.60 (77.05–86.15) 0.134 3.24 (-11.48–1.58)
Heart rate (beats/min)
baseline 69.50 (64.12–75.51) 71.12 (66.99–75.68) 0.658 1.02 (0.92–1.13)
intraoperative 75.16 (69.66–81.10)
<0.001 84.33 (80.72–88.10) <0.001 0.009 1.12 (1.03–1.22)
post-operative 82.03 (74.47–90.16)
88.31 (83.18–93.97) 0.179 1.08 (0.96–1.20)
*Data were analysed with unpaired t-test, are presented as mean of log-transformed data (maximum–minimum), P < 0.05 is significant.
†Data were analysed with repeated ANOVA, post hoc analysis, P < 0.05 is significant.
QL = quadratus lumborum.
Effect of Pre-incisional Ultrasound-guided Quadratus Lumborum Block on Perioperative Analgesia and Inflammatory Responses in
Transperitoneal Laparoscopic Nephrectomy: A Single-blinded, Randomised Control Trial
29

Table 4: Hemodynamic changes between time points comparison.
Parameters Control group (n=22) QL block group (n=22) P
value*
CI 95%
Systolic blood pressure changes (mmHg)
Baseline–intraoperative 6.04 ± 16.12 3.74 ± 13.56 0.618 -2.30 (-11.56–6.96)
Intraoperative–post-operative 12.08 ± 14.23 -4.47 ± 13.35 <0.001 -16.55 (-25.07– -8.04)
Diastolic blood pressure changes (mmHg)
Baseline–intraoperative 3.16 ± 12.26 0.63 ± 14.82 0.539 -2.53 (-10.77–5.71)
Intraoperative–post-operative 7.40 ± 10.48 -4.21 ± 15.37 0.005 -11.61 (-19.48–-3.74)
Mean arterial pressure changes (mmHg)
Baseline–intraoperative 4.12 ± 13.09 1.67 ± 12.99 0.540 -2.46 (-10.47–5.56)
Intraoperative–post-operative 8.96 ± 11.12 -4.30 ± 13.62 0.001 -13.26 (-20.78–-5.73)
Heart rate changes (beats/min)
Baseline–intraoperative 5.56 ± 9.23 13.05 ± 6.96 0.005 7.49 (2.37–12.61)
Intraoperative–post-operative 7.84 ± 12.67
4.26 ± 11.20 0.335 -3.58 (-10.87–3.71)
*Data were analysed with unpaired t-test, are presented as mean ± SD, P < 0.05 is significant.
QL = quadratus lumborum.
heart rate changes (P = 0.005) between the baseline
and intraoperative, compared to the control group.
The variability of the IL-6 levels from the baseline
to the post-operative level was significantly different
between the control and the QL block groups. In each
group, the IL-6 level was significantly increased
intra- and post-operatively, compared to the baseline
level (P < 0.001). The trend of inflammatory response
IL-6 plasma level from baseline to after surgery
increased significantly higher (P = 0.002) in the
control group, compared to the QL block group
(Figure 3).
Figure 3: Inflammatory response of interleukin-6. Data are
presented in log transform data (minimum–maximum); the
horizontal lines indicate the medians; boxes indicate
interquartile ranges; whiskers indicate ranges; P < 0.05 is
significant. GLM = general linear model. QL = quadratus
lumborum block. Non-QL, control group.
4 DISCUSSION
Laparoscopy surgery is increasingly performed
because it promotes early mobilisation, minimises
post-operative complications and reduces hospital
stay, compared to open surgery. Therefore, efforts to
optimise the safety of the procedure, peri-operative
pain management and early daily functioning are
important (Hayden and Cowman, 2011).
In 2007, Blanco first introduced the US-guided
QL block technique as a posterior extension of the
TAP block. It represents a more extensive abdominal
analgesia by placing a curvilinear transducer in a
transverse orientation slightly above the iliac crest in
the posterior axillary line and uses the QL muscle as
its basic sonographic landmark (Chakraborty et al.,
2016; Anders et al., 2018).
The lateral QL (type I) block refers to the injection
of a local anaesthetic at the lateral border of QL
muscle with the spread of local anaesthetic at the
junction of QL and transversalis fascia plane; QL
block produces effective post-operative analgesia in
lower abdominal surgery due to its spread to the
thoracic paravertebral space and thoracolumbar fascia
nerves. The QL block is the extension of the posterior
transversus abdominis plane (TAP) block deep in the
transversus abdominis aponeurosis and generates
sensory blockade from T7–L1 (Ueshima et al., 2017).
We performed the lateral QL (type I) block prior to
the surgical incision. Although the QL (type I) block
produces the local anaesthetic spread and has no
visceral pain relief L1 (Ueshima et al., 2017), our
findings showed that it reduced intraoperative
fentanyl consumption up to 25%, which was
significantly less than without the QL block.
The laparoscopy technique is sometimes
associated with longer operation time, and the peak
level of pain in a laparoscopy procedure is mostly
during trocar port insertion, gas insufflation and the
first two hours after surgery (Warle et al., 2013).
Administering the pre-incisional QL block before the
surgery produced a sufficient intraoperative opioid-
sparing effect and reduced pain intensity 24 hours
The 4th ICE on IMERI 2019 - The annual International Conference and Exhibition on Indonesian Medical Education and Research Institute
30

post-operative in our study. The result was similar to
the previous pre-incisional TAP-block studies in
reducing intraoperative fentanyl requirements
(Bhattacharjee et al., 2014). This is in line with
animal studies, which have strongly suggested that
peripheral nerve block reduced post-operative
hyperalgesia and exposure to a higher dose of opioids
during general anaesthesia and enhanced central pain
sensitisation that led to reducing the effect of
peripheral nerve block in preventing post-operative
pain (Méleine et al., 2012).
Reducing catheter-related bladder discomfort
(CRBD) incidence could also reduce a bias that
obscures post-operative pain assessment. Post-
operative CRBD is common, due to voluntary or
involuntary detrusor muscle contraction of the
bladder stimulated by acetylcholine on the muscarinic
receptor. Pain during bladder catheterisation needs a
sensory blockade of S3 that is outside of the QL block
coverage. Tramadol is a synthetic opioid analgesic
that inhibits detrusor muscle activity through
inhibition of type-1 muscarinic (M1) and type-3
muscarinic (M3) receptors. Rather than using
morphine, we used tramadol, because it produces an
adequate analgesic effect with less urinary retention
and has no impact on voiding function despite an
increase in compliance of the bladder (Agarwal et al.,
2008). From the urologist’s perspective, it is
important to have satisfactory post-operative
analgesia with less of an effect on urinary retention
and reduced CRBD to promote early mobilisation in
LLDN patients.
The QL block group showed lower plasma IL-6
levels two hours after surgery, compared to the
control group. During laparoscopy surgery,
pneumoperitoneum by gas insufflation and surgical
procedure produces visceral pain and somatic pain.
IL-6 is one of the earliest pro-inflammatory responses
induced during pain stimuli and injury, such as in
surgery. Surgical stress enhances the pro-nociceptive
effects of a pro-inflammatory cytokine such as IL-6,
a potential mediator of stress-induced effects on
nociception that is involved in the modulation of pain
and contributes to hyperalgesia. In healthy
volunteers, there is a correlation between pain and
systemic IL-6 in response to stress and injury
(Moeller-Bertram et al., 2012).
Pre-incisional analgesia is a pre-emptive
treatment strategy that focuses on the prevention of
central sensitisation by administering analgesia
before the surgical incision to improve perioperative
pain control. It becomes a part of multimodal
analgesics before the stimulus arises and appears to
be effective in reducing pain and consumption of
analgesics during and after the surgery (De Oliviera
et al., 2011; Vadivelu et al., 2014). Surgical stress
induces the release of inflammatory cytokines and
proteins. Patients taking a pre-emptive oral analgesic
regimen one hour before surgical incision
demonstrated a suppressed plasma hs-CRP level as
the inflammatory mediator response in nociceptive
pain (Jianda et al., 2016). However, there are various
factors that influence the pre-emptive analgesia
effect, such as type and duration of surgery, analgesic
agents used, individual inflammation and physical
responses to the extent of the injury (Farouk, 2008).
A pre-incisional TAP block could demonstrate its
efficacy in reducing the hemodynamic response to a
surgical stimulus (Bhattacharjee et al., 2014). We
expected that the QL block would blunt the
hemodynamic response during surgical procedures.
However, the QL block group showed higher
intraoperative hemodynamic systolic pressure,
diastolic pressure, mean arterial pressure and heart
rate, compared to the control group. These
hemodynamic responses between the groups could be
the result of higher consumption of intraoperative
fentanyl in the control group. However, we found that
the control group had higher perioperative
hemodynamic changes in systolic, diastolic and mean
arterial pressure, compared to the QL block group;
while the QL block group showed a more stable
perioperative hemodynamic variability, compared to
the control group. While we ensured adequate muscle
relaxation and monitored the depth of anaesthesia
with BIS and ETS monitoring, it was difficult to
define the level of intraoperative analgesia based on
hemodynamic parameters (Bhattacharjee et al.,
2014).
There are a few limitations to this study. The
control group may have been more appropriate to
perform QL block using normal saline to improve
blinding, but our institution ethic board recommended
that we avoid invasive intervention using the placebo.
When the NRS started to increase >3, the tramadol
was given by intermittent boluses 8
th
hourly by ward
nurses, but not by PCA based on patient need. The
level of sedation due to tramadol consumption was
not assessed. We could not assess nausea and
vomiting between the groups because antiemetics
were routinely given post-operative, but we were able
to eliminate bias in evaluating post-operative pain by
reducing nausea and vomiting. We excluded patients
with BMI >30; therefore further research of the QL
block on obese patients is needed. Additional
research in pre-emptive analgesia is warranted to
optimise perioperative pain management following
transabdominal laparoscopic surgery.
Effect of Pre-incisional Ultrasound-guided Quadratus Lumborum Block on Perioperative Analgesia and Inflammatory Responses in
Transperitoneal Laparoscopic Nephrectomy: A Single-blinded, Randomised Control Trial
31

5 CONCLUSIONS
The pre-incisional bilateral QL block using 100 mg
of 0.25% bupivacaine resulted in less intraoperative
opioid consumption and a lower post-operative
inflammatory response. It reduced the 24-hour post-
operative pain intensity and additional opioid
consumption following transperitoneal laparoscopic
nephrectomy.
REFERENCES
Agarwal, A., Yadav, G., Gupta, D., Singh, P. K., and Singh,
U. (2008). Evaluation of intra-operative tramadol for
prevention of catheter-related bladder discomfort: A
prospective, randomized, double-blind study. BJA:
British Journal of Anaesthesia, 101(4), 506–510.
http://doi.org/10.1093/bja/aen217.
Barreveld, A., Witte, J., Chahal, H., Durieux, M. E., and
Strichartz, G. (2013). Preventive analgesia by local
anesthetics: The reduction of postoperative pain by
peripheral nerve blocks and intravenous drugs.
Anesthesia and Analgesia, 116(5), 1141–1161.
http://doi.org/10.1213/ANE.0b013e318277a270.
Bhattacharjee, S., Ray, M., Ghose, T., Maitra, S., and
Layek, A. (2014). Analgesic efficacy of transversus
abdominis plane block in providing effective
perioperative analgesia in patients undergoing total
abdominal hysterectomy: A randomized controlled
trial. Journal of Anaesthesiology Clinical
Pharmacology, 30(3), 391–396. http://doi.org/10.4103/
0970-9185.137274
Chakraborty, A., Khemka, R., and Datta, T. (2016).
Ultrasound-guided truncal blocks: A new frontier in
regional anaesthesia. Indian Journal of Anaesthesia,
60(10), 703–711. http://doi.org/10.4103/0019-5049.
191665.
de Oliveira, C. M., Sakata, R. K., Issy, A. M., Gerola, L. R.,
and Salomão, R. (2011). Cytokines and pain. Revista
Brasileira De Anestesiologia, 61(2), 255–259.
http://doi.org/10.1016/S0034-7094(11)70029-0.
Farouk, S. (2008). Pre-incisional epidural magnesium
provides pre-emptive and preventive analgesia in
patients undergoing abdominal hysterectomy. BJA:
British Journal of Anaesthesia, 101(5), 694–699.
http://doi.org/10.1093/bja/aen274.
Hayden, P., and Cowman, S. (2011). Anaesthesia for
laparoscopic surgery. Continuing Education in
Anaesthesia Critical Care & Pain, 11(5), 177–180.
http://doi.org/10.1093/bjaceaccp/mkr027.
Jianda, X., Yuxing, Q., Yi, G., Hong, Z., Libo, P., and
Jianning, Z. (2016). Impact of Preemptive Analgesia on
inflammatory responses and Rehabilitation after
Primary Total Knee Arthroplasty: A Controlled
Clinical Study. Scientific Reports, 6(1), 1–7.
http://doi.org/10.1038/srep30354.
Krohg, A., Ullensvang, K., Rosseland, L. A., Langesæter,
E., and Sauter, A. R. (2018). The Analgesic Effect of
Ultrasound-Guided Quadratus Lumborum Block After
Cesarean Delivery: A Randomized Clinical Trial.
Anesthesia and Analgesia, 126(2), 559–565.
http://doi.org/10.1213/ANE.0000000000002648.
Méleine, M., Rivat, C., Laboureyras, E., Cahana, A., and
Richebé, P. (2012). Sciatic nerve block fails in
preventing the development of late stress-induced
hyperalgesia when high-dose fentanyl is administered
perioperatively in rats. Regional Anesthesia and Pain
Medicine, 37(4), 448–454. http://doi.org/10.1097/
AAP.0b013e318257a87a.
Moeller-Bertram, T., Ky, L., Coe, C., Strigo, I., Kincaid,
M., Keltner, J., … Backonja, M. (2012). Correlation of
pain ratings and systemic interleukin-6 release in
response to intramuscular capsaicin in healthy humans.
The Journal of Pain: Official Journal of the American
Pain Society, 13(4), S52. http://doi.org/10.1016/
j.jpain.2012.01.219.
Mukhtar, K., and Khattak, I. (2010). Transversus abdominis
plane block for renal transplant recipients. BJA:
British Journal of Anaesthesia, 104(5), 663–664.
http://doi.org/10.1093/bja/aeq077.
Richebé, P., Rivat, C., and Liu, S. S. (2013). Perioperative
or postoperative nerve block for preventive analgesia:
should we care about the timing of our regional
anaesthesia? Anesthesia and Analgesia, 116(5), 969–
970. http://doi.org/10.1213/ANE.0b013e31828843c9.
Ueshima, H., Otake, H., and Lin, J.-A. (2017). Ultrasound-
Guided Quadratus Lumborum Block: An Updated
Review of Anatomy and Techniques. BioMed Research
International, 2017, 1–7. http://doi.org/10.1155/2017/
2752876.
Vadivelu, N., Mitra, S., Schermer, E., Kodumudi, V., Kaye,
A. D., and Urman, R. (2014). Preventive analgesia
for postoperative pain control: A broader concept.
Local and Regional Anesthesia, 7(1), 17–22.
http://doi.org/10.2147/LRA.S62160
Warlé, M. C., Berkers, A. W., Langenhuijsen, J. F., van der
Jagt, M. F., Dooper, P. M., Kloke, H. J., … D'Ancona,
F. C. (2013). Low-pressure pneumoperitoneum during
laparoscopic donor nephrectomy to optimize live
donors' comfort. Clinical Transplantation, 27(4),
E478–E483. http://doi.org/10.1111/ctr.12143.
The 4th ICE on IMERI 2019 - The annual International Conference and Exhibition on Indonesian Medical Education and Research Institute
32
