
Two Months of Catching Up Walking Ability in
3-Year-Old Girl with Spastic Diplegic Cerebral Palsy:
Comprehensive Rehabilitation Program Involving the Family
T. Takwarif
1
, R. K. Wardhani
1
1
Department of Physical Medicine and Rehabilitation, Cipto Mangunkusumo Hospital,
University of Indonesia, Jakarta, Indonesia
Keywords: Cerebral Palsy, Diplegic, Rehabilitation, Comprehensive, Family, Home-based, Walking Ability
Abstract: A 3-year-old girl was presented to our clinic with a chief complaint of not being able to stand and walk
unsupported. She was born prematurely on 31 weeks of gestation and was diagnosed with spastic diplegic
cerebral palsy (CP) at the age of two years. During supported standing, she still had noticeable equinus on
both of her feet. We gave comprehensive rehabilitation consisted of a hospital-based and home program.
Hospital-based management was done two times per week included dynamic neuromuscular stabilization
(DNS) technique and conventional exercise such as stretching, strengthening, and postural control exercise.
The home program was done three times per day consisted of DNS, swimming, cycling, standing in an
inclined surface, squat to stand exercise and stretching exercise. After two months of a rehabilitation
program, she was able to stand unaided and walk 2-3 steps independently. We also added botulinum toxin
injection on her gastrocnemius muscle and hinged AFO prescription to improve her walking ability.
Comprehensive rehabilitation program involving healthcare providers and family is an effective approach in
catching up walking ability in a patient with spastic diplegic cerebral palsy.
1 INTRODUCTION
Cerebral Palsy (CP) applies to a non-progressive
neurodevelopmental disorder caused by an insult to
the developing brain, in which the primary clinical
manifestation is a motor deficit. A total of 17 million
people are estimated to have cerebral palsy with
worldwide prevalence is approximately 2.11/1000
live births (Sharan et al., 2016). CP patients have a
nonprogressive brain lesion accompanied by motoric
clinical manifestation that may change over time
during their growth and development. Spastic
diplegia cerebral palsy is a form of CP, with affected
people have increased muscle tone which leads
to spasticity in the muscle (Azar et al., 2015).
In rehabilitation of children with cerebral palsy
(CP), varying approaches and techniques are used,
ranging from very conservative and conventional
techniques, such as muscle strengthening, manual
stretching, and massage, to more complex motor
learning-based theories, such as neurodevelopmental
treatment, conductive education, and several others
(Balci, 2016).
Even though the loss of brain function in CP
cannot be fully recovered, the evolving medical
intervention has been able to reduce secondary
complications and increase patient participation in
activities of daily living. However, the management
of CP is complex and must be tailored to each
specific individual due to the wide variance between
CP cases (Jan, 2006; Kolar et al., 2013). Of the
medical management strategies for CP,
rehabilitation plays a key role in managing
symptoms, preventing secondary complications, and
improving the child’s self-care abilities and
independence (Kolar et al., 2013).
Rehabilitation of CP comes in two forms: home-
based and hospital-based treatment. Several studies
have shown that home-based treatment gives a
beneficial result and a lot more cost-effective than
hospital-based treatment (Azar et al., 2015).
Comprehensive rehabilitation therapy requires a
multidisciplinary approach that includes family and
Takwarif, T. and Wardhani, R.
Two Months of Catching Up Walking Ability in 3-Year-Old Girl with Spastic Diplegic Cerebral Palsy: Comprehensive Rehabilitation Program Involving the Family.
DOI: 10.5220/0009090603470350
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 347-350
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
347
healthcare providers. Both parties are needed to
establish a suitable approach to reach a desirable
goal (İçağasıoğlu et al., 2015).
CP rehabilitation treatment is intended to reduce
or prevent secondary musculoskeletal complications
rather than the primary neurological deficit. Most
rehabilitation strategies are based on the principle of
neuroplasticity, postural control, balance, muscle
stretching and strengthening (Azar et al., 2015).
Rehabilitation is aimed to reach optimal physical,
sensory, intellectual, psychological, and social
function (Balci, 2016). There is no scientific
evidence to compare the benefit of one strategy to
another. The duration and frequency of each therapy
have not yet been established. This study aims to
investigate the result of comprehensive rehabilitation
therapy consisted of home-based and hospital-based
rehabilitation, combined with orthotic use and
botulinum toxin injection to improve walking ability
in children with cerebral palsy.
2 CASE PRESENTATION
A 3-year-old female child was presented to pediatric
rehabilitation outpatient in November 2018 with a
chief complaint of walking difficulty. She was
already able to stand up on her toes, with her hand
grasping the surroundings to stabilize her body.
However, she could not yet walk independently and
still needed aid or support to transfer herself from
sitting to standing position.
She was born at 31 weeks gestation and later
diagnosed with spastic diplegic CP since birth due to
preterm delivery. From history-taking, we found that
the patient had delayed motor development as
summarized in Table 1. She had undergone
physiotherapy at her previous hospital since she was
1,5 years old. Nevertheless, by the age of 3 years,
she still required assistance in standing up from a
seated position and was unable to ambulate unaided.
Thus, her parents wanted to seek a second opinion
and for re-evaluation from our department. She had
a previous history of congenital talipes equinovarus
(CTEV), which was successfully treated by casting.
Spina bifida was not found in this patient. Currently,
she uses bilateral solid ankle-foot orthoses (AFO) to
walk.
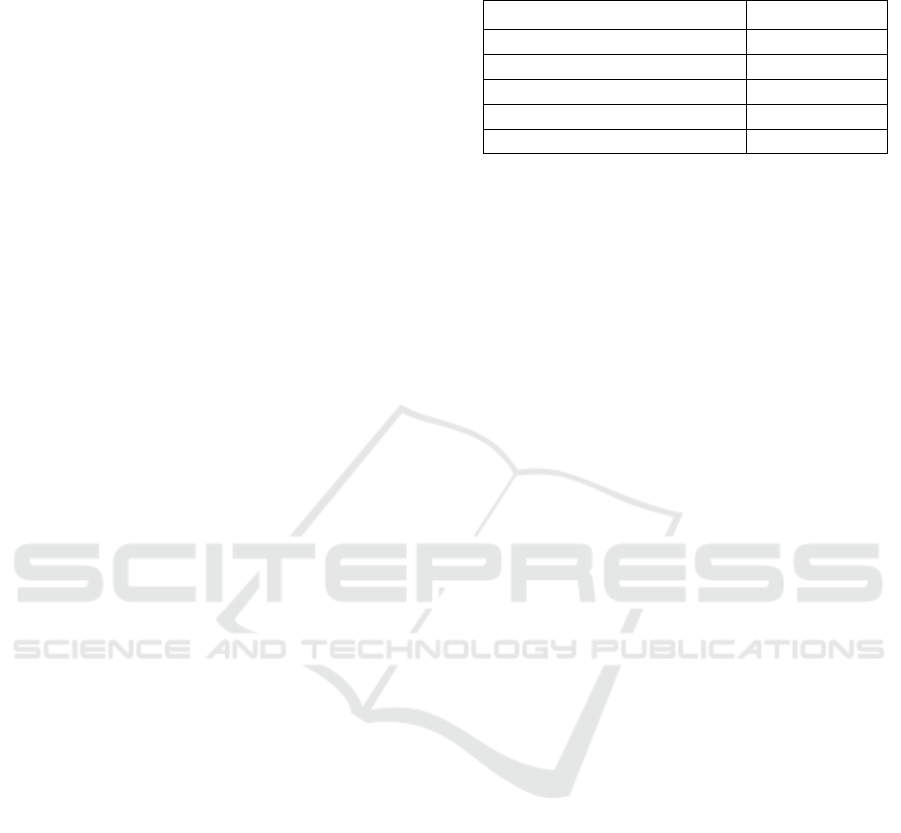
Table 1. Patient’s initial gross motor development
milestones
Milestone Age
Rolling 6 months
Sitting unaided 10 months
Standing up by holding the hand 1 year
Standing up unaided Unable
Walking Unable
On physical examination, her general status was
found to be normal. She had full ROM in all the
lower extremity muscle groups. Motor strength
examination revealed apparent Manual Muscle
Testing (MMT) of 4 on her bilateral hip extensors,
hip flexors, knee extensors, and knee flexors; MMT
of 1 on her bilateral ankle dorsoflexors. Spasticity
was found in both gastrocnemius muscles
(Australian Spasticity Assessment Scale / ASAS 3
for her right gastrocnemius and ASAS 2 for her left
gastrocnemius) with positive Silfverskiöld test.
There was no spasticity on her upper extremities.
Both Thomas and Ely’s test results were negative,
indicating no tightness or spasticity in the hip
flexors. She required assistance in standing up.
While standing up, ankle valgus and slight pronated
foot were observed along with pes equinus posture
and a forward shift of the trunk. She had poor hip
control and was unable to ambulate independently.
The patient scored 0 on the standing dimension and
3 on walking dimensions of the Gross Motor
Function Measure (GMFM) at the initial
examination.
A comprehensive medical rehabilitation program
consisted of hospital-based and home-based
rehabilitation was given to the patient. The hospital-
based rehabilitation program was done twice weekly
involved Dynamic Neuromuscular Stabilisation
(DNS) technique and also a conventional exercise
included stretching exercise, strengthening exercise,
and postural control exercise. DNS technique for
this patient included trigger zone activation started
with trigger zone stimulation in the 5th-6th
intercostal space and the anterior superior iliac
spine. As a part of this technique, we also gave the
developmental position in 5 months old child
position (patient in the supine position, raising and
flexing both hips and knees). DNS lasted for 20
minutes each session. Home-based rehabilitation
program including bicycle training, swimming, squat
to stand exercise, manual stretching, standing with
backslab. DNS was also prescribed as a home
program, which was done by her mother for 20
minutes, three times daily. The patient went
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
348

swimming twice weekly for 30 minutes since the
start of the program. Her mother also manually
stretched her muscles especially gastrocnemius
muscle twice daily with 30 repetitions per session.
Two months in the program, she could move
from sit to stand independently. She could stand
unsupported for 5 minutes without backslab, and
more than 15 minutes when using backslab. She was
able to walk independently for 2–3 steps unaided
using solid AFO she got from the previous hospital.
At that time, she scored 10 in standing and 9 in
walking dimensions of GMFM.
We continue all of the programs. For the DNS
technique, we added stimulation on her lateral
calcaneus. We also added walking exercise
unsupported or supported with the chair as a home
program exercise.
Re-evaluation at six months after the
rehabilitation started showed improvement in
postural control and walking function. She could
stand unaided for 30 minutes. She was able to walk
for 100 meters unaided and able to cycle her tricycle
unaided. To optimize her gait, we changed her
previous solid AFO to hinged AFO. We gave her
botulinum toxin injection on her bilateral
gastrocnemius muscles to reduce her spasticity. Her
scores on the GMFM standing and walking
dimensions also improved to 27 and 20,
respectively.
This case report showed walking ability
improvement that was achieved two months after the
rehabilitation program started. The better function
was remarkable after 6 months of rehabilitation.
3 DISCUSSION
Spastic diplegic CP in our patient was confirmed
with existing movement and postural control
disturbance that caused gross motor development
delay since her early life. Prematurity was suspected
as a risk factor of cerebral palsy in this patient.
The patient came to our clinic in non-ambulatory
conditions despite having already received
rehabilitation treatment from another hospital since
the age of 1,5 years old. She could only stand up
aided at the time of the first presentation. After she
came to our clinic, comprehensive rehabilitation
treatment consisted of a hospital-based and home-
based program that was given to the patient. We
choose to collaborate with family members to
establish family-centered models to improve her
walking ability. A successful collaboration between
health care professionals and family members has
been reported to give a good result in pediatric
rehabilitation settings. This method needs good
communication between both parties which include
effective information exchange, competency of
health care professionals in identifying both the
patient and family's needs and potentials, and the
determination of family members to be involved in
the program. This approach allows us to deliver an
effective rehabilitation service that suits each family
because every family is different (Balci, 2016).
For the hospital-based program, we prescribed
two times weekly DNS treatment lasted for 20
minutes each session. Her DNS program mainly
involved stimulation by activating specific trigger
zones. Trigger zone stimulation involves the
activation of various muscle groups that contributes
to postural control. It stimulates the brain to learn to
use the appropriate muscles in a specific postural
task and strengthen the muscles involved, which can
potentially improve postural control. A study
investigating the effect of DNS in CP patients
showed significant improvement in activation of the
transverse abdominal muscle and the internal
oblique muscle, both of which play a central role as
core stabilizers, thus contributed to improved
postural control in our patient (Kolar et al., 2013).
We also gave the conventional exercise to reduce
equinus, strengthen the muscles, and reach good
postural control.
The home program consisted of DNS,
swimming, cycling, standing in an inclined surface,
squat to stand exercise and stretching exercise.
These exercises increased her overall
cardiorespiratory endurance, coordination, sensory
input, and strength. Research on home-based
physical exercises for muscle strengthening had
shown improvement in gait pattern for children with
cerebral palsy when was done daily for 6 weeks in
young CP patients between eight and eighteen years
old (Patrícia et al., 2012). Swimming is a type of
aerobic exercise also contributed to ameliorating
overall walking ability, accounted for the
improvement in cardiorespiratory endurance. Even
though limited evidence was found on how manual
stretching could improve walking ability, research
has shown that stretching could reduce spasticity.
For this reason, we still prescribed stretching
exercises to the patient (Pin, Dyke, and Chan, 2006;
Novak et al., 2013).
She demonstrated type 3 gait deviation according
to Amsterdam Gait Classification (Becher, 2002),
shown by knee hyperextension and heel rise during
the midstance phase. We chose to change his
orthotic treatment using hinged AFO. Hinged AFO
Two Months of Catching Up Walking Ability in 3-Year-Old Girl with Spastic Diplegic Cerebral Palsy: Comprehensive Rehabilitation
Program Involving the Family
349

is indicated for ambulatory, active children which
we hope to be able to walk up the stairs. This type of
orthosis increases stance stability, normalize the first
contact, and control knee stability. It increases
dorsoflexion which in turn decreases genu
recurvatum and increases toe clearance. Hinged
AFO corrects equinus and provides energy-efficient
gait (Miller, 2005; Ofluo, 2009).
We gave a botulinum toxin injection to decrease
her spasticity in bilateral gastrocnemius muscles.
Botulinum toxin has been proved to be an effective
drug to relieve spasticity by multiple trials (Kaushik
et al., 2018). A systematic review involving several
good quality Randomized Controlled Trials have
investigated the outcome of injection of botulinum
toxin for equinus with positive results utilizing
objective outcome measures (Love et al., 2010).
Improvement in walking and postural control
was shown after two months of rehabilitation. A
remarkable improvement was noticed after six
months of rehabilitation; she could stand for 30
minutes unaided, cycle her tricycle independently,
and able to walk for 100 meters unaided. These
improvements were achieved from a comprehensive
hospital rehabilitation program and support from the
family to comply with the home program.
There was no adverse effect identified during the
study.
4 CONCLUSIONS
A hospital-based and home-based rehabilitation
program is an effective approach for patients with
CP. We gave DNS technique, hinged AFO,
botulinum toxin injection, and conventional
exercise. We also encouraged the family to do the
home program. DNS is a new method that can be
applied as hospital-based and home-based treatment.
Family support is an important aspect of a successful
rehabilitation program. This case report shows the
result of comprehensive rehabilitation treatment
involving both healthcare providers in hospital-
based setting and family as a caregiver in a home
setting.
REFERENCES
Azar, E. S. et al. 2015. ‘Home-based versus center-based
care in children with cerebral palsy: a cost-
effectiveness analysis', Journal of medicine and life,
8(4), pp. 245–251.
Balci, N. C. 2016. ‘Current Rehabilitation Methods for
Cerebral Palsy’, in Gunel, M. K. (ed.) Cerebral Palsy -
Current Steps. Croatia: Intech, pp. 51–78.
Becher, J. G. 2002. ‘Pediatric Rehabilitation in Children
with Cerebral Palsy ’:, JPO Journal of Prosthetics and
Orthotics, 14(4), pp. 143–149.
İçağasıoğlu, A. et al. 2015. ‘Rehabilitation outcomes in
children with cerebral palsy during 2 years', J. Phys.
Ther. Sci., 27(10), pp. 3211–4.
Jan, M. M. . 2006. ‘Cerebral palsy: Comprehensive review
and update’, Annals of Saudi Medicine, 26, pp. 123–
32.
Kaushik, P. S. et al. 2018. ‘A randomized control trial of
botulinum toxin A administration under ultrasound
guidance against manual palpation in spastic cerebral
palsy', Journal of Pediatric Neurosciences, 13(4), pp.
443–447. DOI: 10.4103/JPN.JPN_60_18.
Kolar, P. et al. 2013. Clinical Rehabilitation. Edited by P.
Kolar. Prague: Alena Kobesova.
Love, S. et al. 2010. ‘Botulinum toxin assessment,
intervention, and after-care for lower limb spasticity in
children with cerebral palsy: international consensus
statement', Eur J Neurol, 17(Suppl. 2), pp. 9–37.
Miller, F. 2005. Cerebral Palsy. New York, US: Springer-
Verlag. DOI: 10.1007/b138647.
Novak, I. et al. 2013. ‘A systematic review of
interventions for children with cerebral palsy : state of
the evidence Study design', Developmental Medicine
& Child Neurology. DOI: 10.1111/dmcn.12246.
Ofluo, D. 2009. ‘Orthotic management in cerebral palsy',
Acta Orthop Traumatol Ture, 43(2), pp. 165–172.
DOI: 10.3944/AOTT.2009.165.
Patrícia, P. et al. 2012. ‘Cerebral palsy - lower limbs :
rehabilitation’, Acta Fisiatr, 19(2), pp. 114–122. doi:
10.5935/0104-7795.20120018.
Pin, T., Dyke, P. and Chan, M. 2006. ‘The effectiveness of
passive stretching in children with cerebral palsy’,
Dev Med Child Neurol, 48, pp. 855–62.
Sharan, D. et al. 2016. ‘Neuromusculoskeletal
Rehabilitation of Severe Cerebral Palsy’, in Gunel, M.
K. (ed.) Cerebral Palsy - Current Steps. Croatia:
Intech, pp. 141–172.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
350
