
Factors Associated with Functional Outcome Improvement in
Hospitalized-Ischemic Stroke Patients
Martha Kurnia Kusumawardani
1
, Syeda Tazkia Noor
2
, Putri Ayu Madedi Budiawan
2
, Meisy
Andriana
1
1
Department of Physical Medicine and Rehabilitation, Dr. Soetomo General Hospital,Faculty of Medicine,
University of Airlangga, Surabaya, Indonesia
2
General Practitioner, Surabaya, Indonesia
dr.marthakurnia.spkfr@gmail.com, syeda.tazkia@gmail.com, gabriella.putri7792@gmail.com, meisy1913@yahoo.com
Keywords: Stroke Ischemic, Functional Outcome, Disability, Barthel Index, Predictive Factors.
Abstract: Aim: to identify factors associated with the improvement of functional outcome among hospitalized
ischemic stroke patients who had received rehabilitation program. Methods: A retrospective study of stroke
patient's medical records. Functional outcome improvement was measured by evaluating the Barthel Index
(BI) score on the first day of rehabilitation treatment and the last day in the hospital. Factors that were
thought to associate with BI changes were analyzed using SPSS 23, including door-to-rehabilitation time,
length of hospital stay, hemiparetic side, aphasia, and spasticity. Results: A total of 208 medical records,
121 data were included. Subjects were 52.1% male with a mean age was 57.36 (SD=11.03). There were
33.1% of subjects who had at least one comorbidity. Most of the subjects experienced paresis unilateral
(90.3%). Stroke-related complications were spasticity (19.8%), dysarthria (19%), aphasia (14.9%) and
others. The median time of door-to-rehabilitation treatment and length of stay was 2 days and 9 days. The
increase of the BI score was ranging between 5 to 70. Among the factors analyzed with BI score
improvement, only spasticity that was statistically significant (p=0.002). Conclusion: Spasticity was
significantly associated with functional outcome improvement after stroke rehabilitation program in
hospitalized-ischemic stroke patients.
1 INTRODUCTION
Stroke is a global health problem and a major cause
of long-term disability in Indonesia. The clinical
syndrome of stroke is characterized by an acute loss
of focal brain function lasting more than 24 hours
and in some cases, may lead to death. In Indonesia,
data in 2011 showed that 250.000 (2,5%) people
died due to stroke and the rest (97,5%) had mild to
severe disabilities (Yayasan Stroke Indonesia, 2011).
The prevalence of stroke in Indonesia mostly occurs
in people aged over 45 years and increases
according to the patient's age. That incidence of
stroke has increased gradually according to
Riskesdas (Riset Kesehatan Dasar) from 2007 to
2013 (Depkes RI, 2013). Therefore, considering the
increase in stroke prevalence, the burden of
post-stroke disability has garnered greater
importance to public health. Most stroke survivors
living with long-term physical and functional
disorders such as disruption of the activity of daily
living (ADL).
The World Health Organization (WHO) divides the
burden due to stroke into 3 such as impairment,
disability and handicap (WHO, 2011). A
rehabilitation program is considered one of the key
factors to improve functional outcome in post-stroke
patients. Post-stroke outcomes vary widely, between
and within world regions depending on multiple
factors including demographic profile, stroke type,
severity and immediate and long-term post-stroke
care (Mweshi M et al, 2016). Previous studies have
explained various factors that can affect functional
outcomes in ischemic stroke patients. However,
there are no studies that assess the factor that affects
functional outcomes in ischemic stroke patients who
had received rehabilitation programs in Indonesia.
This study aims to identify factors associated with
the improvement of functional outcomes among
296
Kusumawardani, M., Noor, S., Budiawan, P. and Andriana, M.
Factors Associated with Functional Outcome Improvement in Hospitalized-Ischemic Stroke Patients.
DOI: 10.5220/0009089702960300
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 296-300
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

hospitalized ischemic stroke patients who had
received a rehabilitation program.
2 MATERIALS AND METHOD
2.1 Study Population
This was a retrospective, cross-sectional study,
carried out at Dr. Soetomo General Academic
Hospital, Universitas Airlangga, which is a referral
hospital for eastern Indonesia, located in Surabaya,
East Java. Data were retrieved from medical records
of ischemic stroke patients who were admitted to the
neurology ward and consulted to the Physical
Medicine and Rehabilitation department from
January till December 2018, consecutively. The
diagnosis of ischemic stroke was made by
neurologists. The following information was
obtained from the patient medical records: age; sex;
risk factors (hypertension, diabetes, dyslipidemia,
smoking history, current history of stroke,
cardiovascular disease); presence of comorbid
disease; paresis side, stroke-related complication;
Barthel index score; door-to-rehabilitation time;
length of hospital stay and other relevant data.
Patients were excluded if the diagnosis was not an
ischemic stroke (e.g., hemorrhagic, embolic,
transient ischemic attack [TIA], brain injury), there
was no improvement of BI (remain BI or death) at
last day of admission and medical records data was
incomplete. This study already had ethical clearance
from the institutional ethical board.
2.2 Diagnosis Categories
All data were obtained from the patient's medical
record. All patients underwent standardized
supporting examination, including laboratory
examination (hematology, coagulation, and others),
chest X-ray, electrocardiography (ECG) and
CT-scan. Diagnose of hypertension, diabetes
mellitus, dyslipidemia, cardiovascular disease
(myocardial infarction and atrial fibrillation), and
comorbid diseases were obtained from medical
records, which were diagnosed by a related
specialist doctor (neurologist, cardiologist,
pulmonologist and internist). Paresis side and other
stroke-related complications were defined from
physical and neurological examination result in the
patient's medical records. Door-to-rehabilitation time
was defined as a time difference between patient
first-day admission in the hospital with a first-day
stroke rehabilitation program started. Barthel index
score was assessed on the first day of the
rehabilitation program started and the last day of
hospital admission to evaluate if there any
improvement of the BI score. Only
door-to-rehabilitation time, length of hospital stay,
hemiplegic side, spasticity, and aphasia were
evaluated as the factors that were predicted influence
BI score changes.
2.3 Statistical Analysis
Categorical data were presented as number (%) and
continuous data were presented as mean and
standard deviation if normally distributed.
Statistically, the analysis was done using SPSS for
Windows version 23. Continuous variables were
analyzed with the Mann-Whitney test, Wilcoxon test
and Spearman test. A probability level of p<0.05
was considered significant.
3 RESULTS
Of all 208 ischemic stroke patient’s data, there were
121 ischemic stroke patients enrolled in this study.
The age distribution was 19 to 88 years old with the
proportion of males across all groups was 63
(52.1%). Most of the risk factors were hypertension
(87.6%), type-2 diabetes mellitus (47.1%) and
previous history of stroke (30.6%), see Table 1.
About forty (33.1%) patients had comorbid
diseases with the most prevalent was the presence of
other diseases (10.7%), consist of cardiovascular and
kidney disease; and infection (9.9%) including
pulmonary infection (pneumonia, bronchitis,
pulmonary tuberculosis) and sepsis. Notably, the
majority experienced hemiparesis (91.7%) with 54%
of them had left hemiparesis. The most frequent
stroke-related complication was spasticity,
dysarthria, and aphasia with 19.8%; 19% and 14.9%,
respectively. The average length of hospital stay was
varied between 5 to 30 days. Meanwhile,
door-to-rehabilitation time was also varied from zero
to 11 days.
Factors Associated with Functional Outcome Improvement in Hospitalized-Ischemic Stroke Patients
297
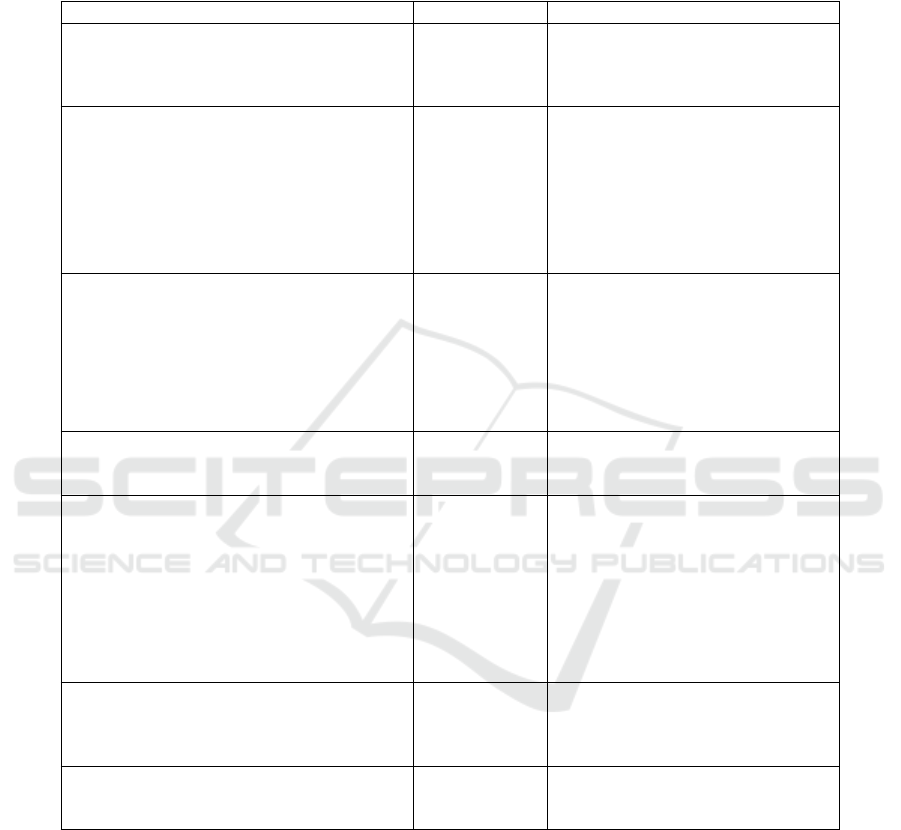
Table 1: Characteristics of the subjects (n=121)
Characteristic
n (%)
Mean ± SD / Median (min-max)
Demographics
Male
Female
Age (years old)
63 (52.1)
58 (47.9)
57.36 ± 11.03
Risk factors
∑ of risk factors
Hypertension
Diabetes mellitus
Smoking
Hyperlipidemia
History of stroke
Cardiovascular disease
106 (87.6)
57 (47.1)
20 (16.5)
20 (16.5)
37 (30.6)
7 (5.8)
2 (0-4)
Comorbidities
∑ of comorbidities
Seizure / Epilepsy post-stroke
Pressure ulcer
Infection
Overweight & obesity
Other diseases
5 (4.1)
3 (2.5)
12 (9.9)
11 (9.1)
13 (10.7)
0 (0-5)
Paresis side
Unilateral
Bilateral
111 (91.7)
10 (8.3)
Other stroke-related complication
Dysphagia
Dysarthria
Aphasia
Motoric
Sensory
Global
Spasticity
Clonus
6 (5)
23 (19)
18 (14.9)
7 (5.8)
1 (0.8)
10 (8.3)
24 (19.8)
4 (3.3)
Ambulation function
Bedridden
Wheelchair
Walking aid
7 (5.8)
29 (24)
1 (0.8)
Barthel Index (BI) score
First-day rehabilitation
Last day hospitalization
30 (0-90)
60 (5-100)
BI score changes were statistically significant
(p<0.001) with a range of BI scores improvement
was 5 to 70. Among factors that were predicted to
affect the increase of the BI score, only the spasticity
was statistically significant with p=0.002. However,
although door-to-rehabilitation time and length of
hospital stay were not statistically significant, each
variable was negatively correlated with BI score
improvement with r= -0.09 (p=0.35) and r= -0.103
(p=0.26), respectively (see Table 2.).
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
298
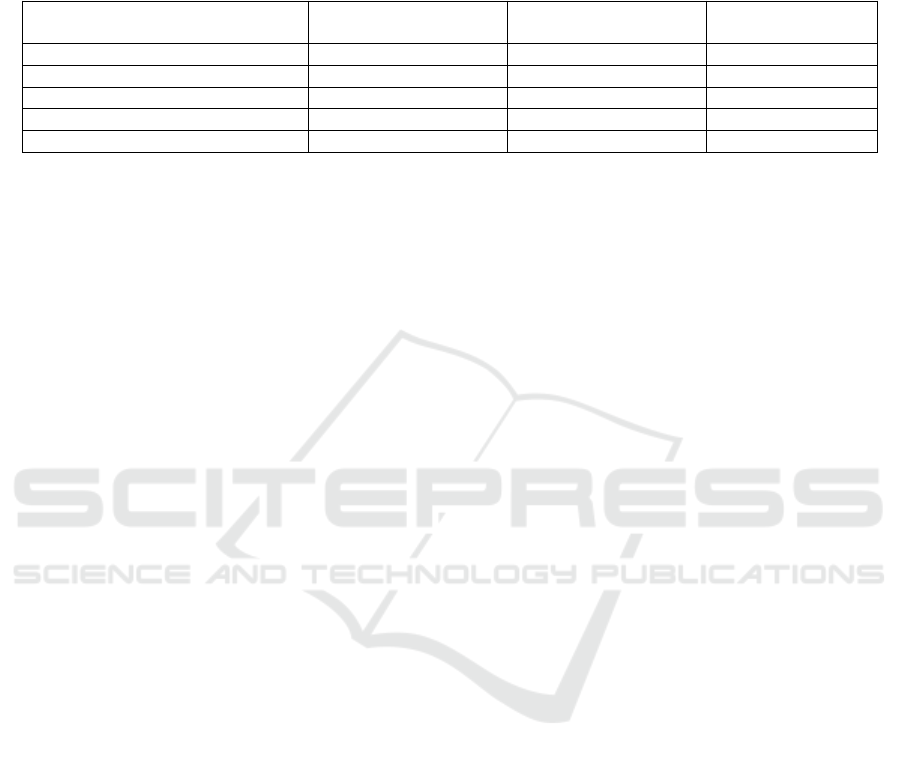
Table 2: Bivariate analysis of variables that could influence the Barthel index (BI) score improvement (n=121)
Variable
Median (min-max)
Spearman’s correlation
value
p-value
Door-to-rehabilitation time (day)
2 (0-11)
- 0.09
0.35
a
Length of stay (day)
9 (5-30)
- 0.103
0.26
a
Hemiparetic side (categorical)
N/A
N/A
0.18
b
Aphasia (categorical)
N/A
N/A
0.09
b
Spasticity (categorical)
N/A
N/A
0.002
b
a
= Spearman correlation test,
b
= Man-Whitney test
4 DISCUSSIONS
Previous studies have shown different results
regarding factors associated with the functional
score changing after the stroke rehabilitation
program. This study used the Barthel Index
(BI)score to measure the activity of daily living
(ADL). However, generally, numerous variables that
associated with functional outcome based on prior
studies are age, gender, prior stroke, diabetes,
severity of stroke, stroke subtype, paresis side, and
neurological complications (McNaughton H et al,
2001; Weimar C et al, 2002; Pei L et al, 2016;
Langhammer B et al, 2017). Besides, a neurological
complication that has been suggested affects
independence were limb paresis, trunk ataxia and
dysphagia (Weimer C et al, 2016). Different from
the previous study, our study only correlates
door-to-rehabilitation time, length of stay,
hemiparetic side, aphasia and spasticity with
functional outcome improvement. Meanwhile, other
suggested factors as in the previous study only
analyze descriptively.
In our study, the overall changes in functional
scores demonstrated a significant improvement.
Surprisingly, door-to-rehabilitation time, length of
stay, hemiparetic side and aphasia had no influence
on the functional outcome after stroke rehabilitation
during hospitalization. Consistent with the study by
Joseph et al, the length of hospital stay showed no
clear effect with the functional outcome of patients
with stroke following rehabilitation (Joseph C and
Rhoda A, 2013). On the contrary, Langhammer et al
(2017) suggested that time to rehabilitation
admission and length of hospital stay associated with
activities of daily living after stroke rehabilitation.
However, Langhammer et al (2017) study had a
bigger sample size and a better study design.
Along with dysarthria, aphasia also has been
reported as a factor associated with functional status
(Kim G et al, 2016; Kongsawasdi S et al, 2018). In
the present study, aphasia had no significant effect
on the BI score improvement. Also, congruent with
Park SY et al (2011), the hemiparetic side did not
contribute to the functional outcome of stroke
patients receiving rehabilitation programs (Park SY
et al, 2011). Only spasticity showed a significant
association with BI score improvement after the
stroke rehabilitation program. Another study
suggested that stroke patients with spasticity had a
lower BI (Wissel et al, 2010). Rate of patient
dependency on ADL according to BI also higher in
patients with spasticity (Lundström E et al, 2008;
Cacho RO et al, 2017). Other factors that suggested
associated with functional outcome improvement by
Langhammer et al. were the number of various
therapies per day and hours of therapy provided per
day, which were not assessed in the present study
(Langhammer B et al, 2017).
As a nature of the retrospective study, the major
limitation was the certainty of BI score evaluation
because it was only obtained as a total score, we can
not evaluate each component of daily living
activities in Barthel Index. Besides, the evaluation of
the BI score was not done in the same evaluation
time frame. Risk factors analyzed in this study were
limited, even though other risk factors should be
accounted for as in the prior studies. Our study
design also does not allow follow up, therefore, the
further large and multicenter prospective study
design is needed to better understand factors
associated with functional outcome improvement of
stroke rehabilitation in Indonesia.
5 CONCLUSIONS
Improvement of the BI score represented significant
functional outcome improvement. Spasticity showed
a significant effect on functional outcome
Factors Associated with Functional Outcome Improvement in Hospitalized-Ischemic Stroke Patients
299

improvement. Further study with better study design
is required to evaluate prognostic factors of
functional improvement after stroke rehabilitation
programs in the Indonesian population.
ACKNOWLEDGEMENT
The authors would like to thank Dr. Soetomo
Hospital, Department of Physical Medicine and
Rehabilitation Dr. Soetomo Hospital - Universitas
Airlangga, and others who support this research.
REFERENCES
Yayasan Stroke Indonesia. 2011. Tangani Masalah Stroke
di Indonesia. [cited in 1st April 2013]. Available from:
www.yastroki.or.id.
Depkes RI. 2013. Laporan Hasil riset kesehatan dasar,
RISKESDAS Indonesia Tahun 2013. Depkes, Jakarta
WHO. 2011. International Classification of Functioning,
Disability, and Health (ICF).
Mweshi M, Shula H, Nkhata L, Chiluba B. 2016.The Best
Time to Start Stroke Rehabilitation: A Review of the
Evidence in Resource-Adequate and
Resource-Constrained Settings. Journal of Preventive
and Rehabilitative Medicine.1(1):7-12.
McNaughton H, Weatherall M, Taylor W, McPherson K.
2001.Factors influencing rate of Barthel Index change
in hospital following stroke. Clinical Rehabilitation 15:
422–7.6.
Weimar C, Ziegler A, König IR, Diener HC. 2002.
Predicting functional outcome and survival after acute
ischemic stroke. J Neurol. 249:888–95
Pei L, Zang XY, Wang Y, Chai QW, Wang JY, Sun CY,
Zhang Q. 2016. Factors associated with activities of
daily living among the disabled elders with stroke.
international journal of nursing sciences. 3:29-34
Langhammer B, Sunnerhagen KS, Lundgren-Nilsson A,
Sallstrom S, Becker F, Stanghelle JK. 2017. Factors
enhancing activities of daily living after stroke in
specialized rehabilitation: an observational
multicenter study within the sunnies international
Network. European Journal of physical and
rehabilitation Medicine. 53(5):725-34
Joseph C, Rhoda A. 2013. Activity limitations and factors
influencing functional outcome of patients with stroke
following rehabilitation at a specialized facility in the
Western Cape. African Health Sciences. 13(3):
646-54.
Kim G, Min D, Lee EO, Kang EK. 2016. Impact of
cooccurring dysarthria and aphasia on functional
recovery in post-stroke patients. Annals of
Rehabilitation Medicine 40(6):1010–17.
Kongsawasdi S, Klaphajone J, Watcharasaksilp K,
Wivatvongvana P. 2018. Prognostic Factors of
Functional Recovery from Left Hemispheric Stroke.
The Scientific World Journal.
Park SY, Lee IH. 2011. The influence of age, lesion side
and location on rehabilitation outcome after stroke. J
Phys. Ther. Sci. 23:817-9.
Wissel J, Schelosky LD, Scott J, Christe W, Faiss JH,
Mueller J. 2010. Early development of spasticity
following stroke: a prospective, observational trial. J
Neurol.. 257(7): 1067-72.
Lundström E, Tere A, Borg J. 2008. Prevalence of
disabling spasticity one year after first-ever stroke. Eur
J Neurol.15(6):533-9.
Cacho RO, Cacho EWA, Loureiro AB, Cirne GNM,
Pereira SA, Freitas RPA, Lima NMFV, Borges G.. 2017.
The spasticity in the motor and functional disability in
adults with post-stroke hemiparetic. Fisioter Mov.
30(4):745-52.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
300
