
The Immediate Effect of Radial Extracorporeal Shockwave Therapy
for Spasticity and Motor Function in Chronic Post-stroke Patients
Andre Tanuwijaya, Jeane Claudia Profita, Ardi Soeharta Chandra, Vitriana Biben, Ellyana Sungkar
Department of Physical Medicine and Rehabilitation, Dr. Hasan Sadikin General Hospital,
University of Padjadjaran, Bandung, Indonesia.
drandrefkunpad@gmail.com
Keywords: Chronic Stroke, Motor Function, Spasticity, Radial ESWT, Rehabilitation.
Abstract: This study aimed to report the immediate effect on spasticity and motor function of radial extracorporeal
shockwave therapy (rESWT) as part of a comprehensive treatment program for chronic stroke patients
with spasticity and functional problem in upper extremities. Chronic poststroke patients with spasticity on
upper extremity were enrolled and got rESWT that applied at muscle belly of the biceps muscle, flexor
carpi ulnaris muscle, and flexor carpi radialis muscle. Patients were evaluated for elbow flexor and wrist
flexor spasticity using Modified Ashworth Scale (MAS), and for motor function using Fugl-Meyer
Assessment for Upper Extremity (FMA-UE) at baseline and immediately after rESWT therapy session. 6
male and 1 female patients participated, age 59.7+5.5 years old, with mean onset time of stroke were 40.4
+ 25.2 months. The MAS score was 5.4 1.5 at baseline and 4.2 1.2 after the treatment (p<0.05). The
score of motor function FMA-UE scale was 26.4 9.0 at baseline and 28.6 9.9 after the treatment
(p<0.05). Radial ESWT immediately improved spasticity and motor function in some chronic poststroke
patients. More studies are necessary to establish if rESWT for spasticity and motor function in chronic
poststroke is clinically effective.
1 INTRODUCTION
Spasticity, commonly defined as “a motor disorder
characterized by a velocity-dependent increase in
tonic stretch reflexes with exaggerated tendon jerks,
resulting from hyperexcitability of the stretch reflex”
is a common complication in poststroke associated
with other signs and symptoms of the upper motor
neuron syndrome (Francisco, 2012). The prevalence
of poststroke spasticity has been reported
approximately 39% in patients with a first attack
stroke after 12 months (Watkins, 2002), and
approximately 17-25% after 3 months post stroke,
21-25% since 1-3 weeks after the attack.
(Sommerfeld, 2012; Katoozian, 2018).
Poststroke patients, presented with spasticity and
other upper motor neuron syndromes such as
agonist/antagonist co-contraction, weakness, and
lack of coordination, may have worse impairments
and functional problems that can predispose other
costly complications and detain rehabilitation
process (Francisco, 2012; Duncan, 2005). The
pathomechanism of spasticity is caused by
hyperexcitability of motor neurons by augmented of
excitatory synapse input and excitability of muscle
spindle, reduction of inhibiting synapse input,
change of nerve electrical characteristics or
mechanical alteration in intrinsic muscle
components (Hasuk, 2010). The main factor of the
spasticity in chronic poststroke is the mechanical
change of intrinsic muscle characteristics, such as
structural shortening of muscles (Lundy, 2013) and
muscle fibrosis (Mirbagheri, 2008). The current
general treatment for spasticity consists of passive
stretching, splints, oral medications, phenol
injection and botulinum toxin (BTX). However,
until recently spasticity therapy in poststroke
patients often inadequate (Francisco, 2012).
Radial ESWT (rESWT) is a type of shock wave
that is pneumatically generated, producing low to
medium energy, superficial, larger therapeutic area,
and more economical compared to traditional
focused ESWT (fESWT) (Chang, 2012). Recent
studies have reported that ESWT is a safe, non-
invasive, and is an alternative spasticity therapy that
does not cause muscle weakness or unwanted
Tanuwijaya, A., Profita, J., Chandra, A., Biben, V. and Sungkar, E.
The Immediate Effect of Radial Extracorporeal Shockwave Therapy for Spasticity and Motor Function in Chronic Post-stroke Patients.
DOI: 10.5220/0009088202090214
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 209-214
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
209

effects in patients with strokes (Santamato, 2013).
The mechanism underlying the beneficial effects of
ESWT on spasticity still needs to be explored.
Previous studies have proposed the theory that
ESWT affects the production of nitric oxides (NO)
(Mariotto, 2005), decreases muscle fibrosis,
modifies spinal cord excitability (Manganotti,
2005), or impacts on Golgi tendon organs or
mechanical vibrations (Hasuk, 2010).
Hypothetically, mechanical vibration from ESWT
will cause an immediate decrease of muscle fibrosis
that will modify muscle spindle excitability causing
decreases the spasticity (Manganotti, 2005).
Some studies have shown that ESWT
administration can reduce hand and wrist spasticity
accompanied by improved wrist and hand control
function in chronic poststroke patients (Li, 2016)
(Guo, 2017). Even though rESWT immediate effect
on spasticity poststroke using Modified Ashworth
Scale (MAS) had been done in many studies (Hasuk,
2010; Li, 2016), there is no other study evaluate
rESWT immediate effect on motor function using
Fugl-Meyer Assessment for Upper Extremity (FMA-
UE). The Fugl-Meyer Assesment is a well-designed,
feasible and efficient clinical examination method
that has been tested widely in the stroke population.
The Fugl-Meyer motor scale is recommended highly
as a clinical and research tool for evaluating changes
in motor impairment following stroke (Gladstone,
2002).
Therefore, the aim of this study is to report the
immediate effect on spasticity and motor function of
radial extracorporeal shockwave therapy (rESWT)
as part of a comprehensive rehabilitation program
for chronic post-stroke patients with spasticity and
functional problem in upper extremities.
2 METHODS
This is an experimental study, done at the outpatient
Physical and Medical Rehabilitation Clinic of Dr.
Hasan Sadikin General Hospital, Bandung,
Indonesia. This study included chronic post-stroke
patients with spasticity on upper extremity (MAS
1+) that persist more than 3 months after stroke.
Patients with joint contracture, recently got phenol
or botox injection, had malignancy, coagulopathy,
infection, using pacemaker were excluded.
Each subject got rESWT (Swiss Dolorclast
®
Smart20) that applied at muscle belly of the biceps
muscle, flexor carpi ulnaris muscle, and flexor carpi
radialis muscle. Each site had 2000 shot of rESWT
with pressure 3 bar, frequency 8 Hz, applicator 36
mm
2
.
Patients were evaluated for elbow flexor and
wrist flexor spasticity using Modified Ashworth
Scale (MAS). The maximum MAS score in this
study was 5, and 1+ was converted to 2. The average
MAS score was calculated as the mean MAS score
of the elbow flexor and wrist flexor spasticity (Chia-
Ling, 2019). Evaluation motor function was using
total motor function score Fugl-Meyer Assessment
for Upper Extremity (FMA-UE) with minimum
score is 0 and maximum score is 66. The evaluation
was done at baseline and immediately after rESWT
session. Each participant signed the informed
consent form. This study had been approved by the
local hospital ethical review board (No:
LB.02.01/X.6.5/101/2019).
All analyses were performed using Statistical
Package for Social Sciences (SPSS) software ver.
17.0 (SPSS Inc., Chicago, IL, USA). A paired t-test
was conducted to determine statistical differences in
the variables between the pre and post treatment.
Values are presented as mean±standard deviation for
data with normal distribution, and p<0.05 was
considered statistically significant.
3 RESULTS
Six male and 1 female patients were included, mean
age 59.7+5.5 years. Mean time were 40.4+25.2
months after the onset of stroke. The scores of MAS
improved immediately after radial rESWT in 71.4 %
of patients. The MAS score was 5.4
1.5 at baseline
and 4.3
1.1 after the treatment (p=0.007). The score
of motor function FMA-UE scale was improved
immediately after rESWT in 71.4 % patients. The
score of motor function FMA-UE scale was
26.4
9.0 at baseline and 28.6
9.9 after the treatment
(p=0.015)(Table 1, Figure 1).
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
210
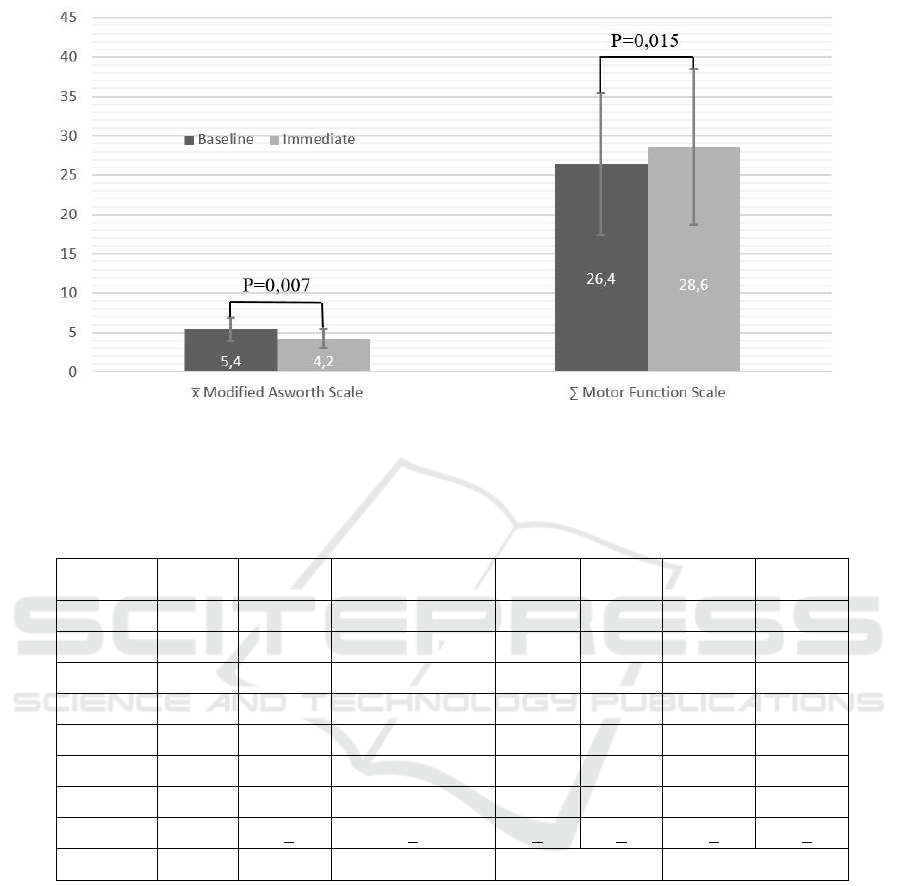
Figure 1: Immediate Improvements after rESWT.
Table 1: Results.
M: Male, F: Female, MAS-B: Modified Ashworth Scale Baseline, MAS-I: Modified Ashworth Scale Immediate, MF-
B: Motor Function from Fugl-Meyer Assesment for Upper Extremity Baseline, MF-I: Motor Function from Fugl-
Meyer Assesment for Upper Extremity Immediate. *The result is significant at p < 0.05
4 DISCUSSIONS
The present study evaluated the effects of rESWT in
chronic post-stroke patients with spasticity on the
upper extremity in terms of spasticity improvement,
and motor function features. We found statistically
significant improvement in spasticity after the
treatment in this study. The score change of
spasticity (1.1429±0.667) in this study exceeds the
minimal clinically important difference of average
Modified Ashworth Scale of the effect size 0.8
standard deviations for extremity muscles which are
0.76 (Chia-Ling, 2019). This result is similar to
previous study that there was immediate effect of
rESWT on chronic poststroke patient's spasticity
(Hasuk, 2010).
The effect of ESWT for chronic poststroke
spasticity in the short-term and long-term had been
studied in many studies (Suputtitada, 2018). Li et al.
found that the effect of a single application of
rESWT on post stroke spasticity persists at least 8 to
12 weeks, while 3 sessions of rESWT effect persist
at least 16 weeks (Li, 2016). However, Hasuk et al.
study had a different result. They conclude that
spasticity after chronic poststroke improved
immediately after rESWT, but was not changed
Subject
No.
Gender
(M/F)
Age
(years)
Time since stroke
(months)
x
MAS-B
x
MAS-I
∑
MF-B
∑
MF-I
1
M
53
24
4
2
18
20
2
M
65
82
6
5
41
47
3
M
54
6
5
5
13
20
4
M
50
9
3
3
21
21
5
M
61
18
8
6
16
16
6
M
65
84
8
6
40
48
7
F
70
60
4
3
36
38
meanSD
59.7+5.5
40.4+25.2
5.4+1.5
4.2+1.2
26.4+9.0
28.6+9.9
t-test
p =0.007*
p =0.015*
The Immediate Effect of Radial Extracorporeal Shockwave Therapy for Spasticity and Motor Function in Chronic Post-stroke Patients
211

significantly at 1 week and 4 weeks after rESWT
(Hasuk, 2010). We conduct this preliminary report
as a part of an ongoing, larger and long-term study
about the effect of rESWT on poststroke spasticity.
We intended to give additional prespective to those
contradictory results about the short-term and long-
term effects of rESWT on spasticity poststroke.
The spasticity can be categorized into the part by
stretch reflex, as the neural component of hypertonia,
and stiffness of muscle intrinsic, as the nonneural
component of hypertonia. Spasticity triggered by
stretch reflex progressively increases for 1-3 months
after stroke and after that, it decreases, so the muscle
intrinsic stiffness takes part in the main trigger of the
spasticity. Over the course of time, prolonged
muscle activation due to spasticity will cause muscle
fiber shortening which results in increased passive
stiffness that caused by increased amounts of
collagen in the extracellular matrix of muscle fiber
bundles (Lynn, 2015). Mirbagheri et al also found
that there is neural reflex of skeletal muscle factor
and intrinsic mechanical factor contribute to
spasticity that is different according to the status of
disease, patients' age, and duration of disease
(Mirbagheri, 2008). In this study, we found that
there was an immediate improvement of spasticity
after treatment in most patients, but there is no
immediate improvement in 2 patients with shorter
duration of disease. The muscle intrinsic factor
would be the main factor in the spasticity is highly
probable in patient with longer duration of diseases
and there could be marked immediate effect of
spasticity reduction effect by mechanical high-
frequency vibration of ESWT in those patients
(Manganotti, 2005; Hasuk, 2010). The reduced
extensibility, due to soft tissue changes, causes
pullings to be transmitted more readily to the muscle
spindles. In this condition, an exaggerated spindle
discharge in response to muscle stretch might lead to
an increased stretch reflex. The reduction of non-
reflex hypertonia could modify muscle spindles
excitability, leading to a secondary reduction of
spasticity (Gracies, 2005; Marinelli 2015).
The improvement of motor function from Fugl-
Meyer Assesment for Upper Extremity is found in 5
of 7 patients in this study. The improvement was
statistically significant when compared with the
baseline. The increased score indicates improvement
of the motor function of poststroke patients and in
this study, the increment exceeded the minimal
clinically important difference for Fugl-Meyer
Assesment for Upper Extremity which is more than
4.25 in 3 patients (Page, 2012).
The upper limb function of poststroke patients is
affected by many factors, such as muscle strength,
muscle tone, joint disturbances, proprioception, pain,
and motor control. However, spasticity and
weakness are the primary reason for rehabilitative
intervention in the chronic stages (Bang 2009;
Gandolfi, 2019). Upper limb weakness after stroke is
prevalent and determinant of upper limb function in
ADLs. Literature supports upper limb strengthening
training effectiveness for all levels of impairment
and in all stages of recovery (Harris, 2010). Those
findings were underlining the importance the
neurorehabilitation treatment such as strengthening
exercises for the antagonist muscles, endurance
exercises, balance and coordination training for
enhancement the movement ability and the
functional outcome of the patients (Suputtitada,
2018).
Improvement of the spasticity from the rESWT
therapy session not directly make the improvement
of the upper limb function in our study. Poststroke
patients with mild-moderate impairment of muscle
strength with reduce spasticity seems will have
greater improvement of upper limb function
compare patients to one with severe impairment of
muscle strength. Unfortunately, we didn’t collect
data on muscle strength of each patient to conduct
such analysis.
In addition, we conducted data collection for
pain during and after shockwave therapy using
Numeric Rating Scale (NRS) and asked if they
would recommend ESWT for other patients with
same condition as them because recent studies have
found that ESWT application is considered painfull
(Roerdink, 2017; Haake, 2002) and would make
some rejection of the patients. From those data, we
found that all patients reported shockwave to be
painful during treatment (NRS ≥ 6 out of 10), but
there is no post treatment pain. Furthermore, 5 of 7
patients still would recommend ESWT for other
patients with same condition as them.
Our study has several limitations. First, this
study had a small sample size. Second, we evaluated
only the immediate outcomes. Third, there is no
control group. We suggest to do a further
investigation with larger sample size, with
evaluation short-term and long-term effect of
rESWT on poststroke spasticity with comparison to
conventional therapy. The study also needed to
evaluate characteristics of poststroke patient have
good response to rESWT and specific regimen with
regard to dose, frequency, and location of therapy
that more effective to decrease the spasticity.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
212

5 CONCLUSIONS
Radial ESWT immediately improved spasticity and
motor function in some chronic poststroke patients.
More studies are necessary to establish the
effectiveness of rESWT in spasticity and motor
function in chronic poststroke.
REFERENCES
Bang Y-S, Kim H-Y, Lee M-k. 2009. Factors affecting the
upper limb function in stroke patients. The Journal of
the Korea Contents Association; 9:202-10
Chang K-V, Chen S-Y, Chen W-S, Tu Y-K, Chien K-L.
2012. Comparative effectiveness of focused shock
wave therapy of different intensity levels and radial
shock wave therapy for treating plantar fasciitis: a
systematic review and network meta-analysis. Arch
Phys Med Rehabil; 93(7):1259–68
Chen CL, Chen CY, Chen HC, Wu CY, Lin KC, Hsieh
YW, et al. 2019. Responsiveness and minimal
clinically important difference of modified ashworth
scale in patients with stroke. Eur J Phys Rehabil Med.
doi: 10.23736/S1973-9087.19.05545-X.
Duncan PW, Zorowitz R, Bates B, Choi JY, Glasberg JJ,
Graham GD, et al. 2005. Management of adult stroke
rehabilitation care: a clinical practice guideline. Stroke;
36(9):e100-143
Francisco GE, McGuire JR. 2012. Poststroke spasticity
management. Stroke; 43(11):3132–6
Gandolfi M, Valè N, Dimitrova EK, Mazzoleni S, Battini
E, Filippetti M, et al. 2019. Effectiveness of robot-
assisted upper limb training on spasticity, function and
muscle activity in chronic stroke patients treated with
botulinum toxin: a randomized single-blinded
controlled trial. Front. Neurol. 10:41. DOI:
10.3389/fneur.2019.00041
Gerdesmeyer L, Wagenpfeil S, Haake M, Maier M, Loew
M, Wörtler K, et al. 2003. Extracorporeal shock wave
therapy for the treatment of chronic calcifying
tendonitis of the rotator cuff: a randomized controlled
trial. JAMA; 290(19):2573–80
Gladstone DJ, Danells CJ, Black SE. 2002. The fugl-
meyer assessment of motor recovery after stroke: a
critical review of its measurement properties.
Neurorehabil Neural Repair;16(3):232-40.
Gracies J. 2005. Pathophysiology of spastic paresis. I:
Paresis and soft tissue changes. Muscle Nerve; 31:
535-551.
Guo P, Gao F, Zhao T, Sun W, Wang B, Li Z. 2017.
Positive effects of extracorporeal shock wave therapy
on spasticity in poststroke patients: A Meta-Analysis.
J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc;
26(11):2470–6
Haake M, Böddeker IR, Decker T, Buch M, Vogel
M, Labek G. 2002. Side-effects of extracorporeal
shock wave therapy (eswt) in the treatment of tennis
elbow. Arch Orthop Trauma Surg; 122:222-8
Harris JE, Eng JJ. 2010. Strength training improves upper-
limb function in individuals with stroke: a meta-
analysis. Stroke; 41:136–40. DOI:
10.1161/STROKEAHA.109.567438
Hasuk B, Min LJ, Hwan LK. 2018. The effects of
extracorporeal shock wave therapy on spasticity in
chronic stroke patients. Ann Rehabil Med; 34(6):663-9
Katoozian L, Tahan N, Zoghi M, Bakhshayesh B. 2018.
The onset and frequency of spasticity after first ever
stroke. J. Natl Med Assoc;110(6):547-552
Li T-Y, Chang C-Y, Chou Y-C, Chen L-C, Chu H-Y,
Chiang S-L, et al. 2016. Effect of radial shock wave
therapy on spasticity of the upper limb in patients with
chronic stroke: a prospective, randomized, single blind,
Controlled Trial. Medicine (Baltimore); 95(18):e3544
Lundy-Ekman L. 2013. Neuroscience: Fundamentals for
rehabilitation: Elsevier/Saunders; 217-220.
Lynn Bar-On, Guy Molenaers, Erwin Aertbeliën, et al..
2015. Spasticity and Its Contribution to Hypertonia in
Cerebral Palsy. BioMed Research International; vol.
2015, Article ID 317047, 10
pages. https://doi.org/10.1155/2015/317047.
Manganotti P, Amelio E. 2005. Long-term effect of shock
wave therapy on upper limb hypertonia in patients
affected by stroke. Stroke; 36(9):1967-71
Marinelli L, Mori L, Solaro C, Uccelli A, Pelosin E, Currà
A, et al. 2015. Effect of radial shock wave therapy on
pain and muscle hypertonia: a double-blind study in
patients with multiple sclerosis. Mult Scler;
Apr;21(5):622-9. DOI: 10.1177/1352458514549566.
Epub 2014 Sep 25. PubMed PMID: 25257616.
Mirbagheri MM, Tsao C, Settle K, Lilaonitkul T, Rymer
WZ. 2008. Time course of changes in neuromuscular
properties following stroke. Conf Proc IEEE Eng Med
Biol Soc; 2008:5097-100
Page SJ, Fulk GD, Boyne P. 2012. Clinically important
differences for the upper-extremity fugl-meyer scale in
people with minimal to moderate impairment due to
chronic stroke. Phys Ther; 92(6):791-8
Roerdink RL, Dietvorst M, van der Zwaard B, van der
Worp H, Zwerver J. 2017. Complications of
extracorporeal shockwave therapy in plantar fasciitis:
Systematic review. Int J Surg.; 46:133-45
Santamato A, Notarnicola A, Panza F, Ranieri M, Micello
MF, Manganotti P, et al. 2013. SBOTE study:
extracorporeal shock wave therapy versus electrical
stimulation after botulinum toxin type an injection for
post-stroke spasticity-a prospective randomized trial.
Ultrasound Med Biol; 39(2):283–91
Sommerfeld, D. K., Gripenstedt, U., & Welmer, A.-K.
2012. Spasticity after stroke: an overview of
prevalence, test instruments, and treatments. Am J
Phys Med Rehabil; 91(9), 814–820
Suputtitada A. 2018. Novel Evidences of Extracorporeal
Shockwave Therapy for Spasticity. J Physic Med
Rehabilita Stu 1(1): 101
Trompetto C, Marinelli L, Mori L, Pelosin E, Currà A,
Molfetta L, et al. 2014. Pathophysiology of spasticity:
The Immediate Effect of Radial Extracorporeal Shockwave Therapy for Spasticity and Motor Function in Chronic Post-stroke Patients
213

implications for neurorehabilitation. BioMed Research
International; vol. 2014, Article ID 354906,
https://doi.org/10.1155/2014/354906.
Watkins CL, Leathley MJ, Gregson JM, Moore AP, Smith
TL, Sharma AK. 2002. Prevalence of spasticity post
stroke. Clin Rehabil; 16(5):515–22
Yao X-Y, Lin Y, Geng J-L, Sun Y-M, Chen Y, Shi G-W,
et al. 2012. Age- and gender-specific prevalence of
risk factors in patients with first-ever ischemic stroke
in china. Stroke Res Treat; 2012:136398-
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
214
