
Insignificant Difference of Mucociliary Clearance in Middle-Aged
and Elderly Patients
Febrian Mulya Santausa, Nury Nusdwinuringtyas
Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo General Hospital,
University of Indonesia, Jakarta, Indonesia
febrianmulyasantausa@gmail.com, nury_nus@yahoo.com
Keywords: Aging, Elderly, Middle-aged, Mucociliary Clearance
Abstract: Aging has always been assumed to have negative effect on mucociliary clearance, but studies are in fact
limited. Nasal mucociliary clearance (NMC) is a mirror image of bronchial clearance. This study aims to
evaluate the difference of NMC, measured by saccharin test, in middle-aged (40-59 years) and elderly
(>60 years) patients which are the most common age groups in our clinical settings. It is a cross-sectional
study involving middle-aged (n=18) and elderly (n=12) patients. Smokers and patients having respiratory
symptoms were excluded. Data of age, sex, history of diabetes, malignancy, forced vital capacity (FVC),
forced expiratory volume in one second (FEV1)/FVC ratio, and saccharin transit time were taken. There
is no significant difference in baseline characteristics, except FVC. Saccharin transit time (STT) was not
statistically different between middle-aged and elderly patients (11.9+5.8 vs 12.8+6.3 mins, p=0.696). A
patient with Bechet’s disease had abnormally prolonged STT (26.13 mins). With this patient excluded,
history of malignancy was the only factor associated with STT (p=0.026) after linear regression. In fact,
only subjects with history of chemotherapy had prolonged STT. The findings suggest that there are other
factors to be aware of while evaluating mucociliary clearance, such as history of chemotherapy and
autoimmune disease.
1 INTRODUCTION
Sputum retention is one of the most common
problem in pulmonary rehabilitation. Sputum
retention is a sign of inadequate mucociliary
clearance. This problem can lead to pneumonia
which could be life-threatening for the patient
(Marini, 2016). This is why it is clinically important
to recognize factors affecting mucociliary clearance.
Generally, there are two important factors
affecting mucociliary clearance, mucus consistency
and ciliary movement (Bonde, 2002). Increased
mucus consistency is usually caused by lung or
airway inflammation, but factors affecting ciliary
movement are rather unexplored (Rubin, 2004).
Smoking is a widely-known factor affecting ciliary
movement (Baby, 2014), but other factors are still
debatable. Malignancy and diabetes are also said to
have deteriorating effect on mucociliary clearance,
but data supporting it are scarce (Gupta, 2006;
Gurung, 2017). On the contrary, aerobic exercise
was found to have immediate effect in improving
mucociliary clearance (Ramos, 2015).
Besides the modifiable factors mentioned above,
there are other factors that might affect mucociliary
clearance. Aging is one of the unmodifiable factors
theoretically assumed to have negative effect on
mucociliary clearance. Little is known regarding the
mechanism of how aging affects mucociliary
clearance. A study (Bailey, 2014) suggests that it
might have something to do with protein kinase C
epsilon (PKCε) of which activity in lung is
increased with aging in mice, but it has not been
explored in humans. The author speculated that
increased PKCε activity can increase abnormal
phosphorylation of axonemal proteins, especially
outer dynein arm protein which has an important
role in ciliary movement. Based on the assumption,
geriatric patients have become a special concern in
pulmonary rehabilitation because they are predicted
to have slower mucociliary clearance. However, if
we look at the clinical evidence, not a lot of studies
have actually discussed this matter.
204
Santausa, F. and Nusdwinuringtyas, N.
Insignificant Difference of Mucociliary Clearance in Middle-Aged and Elderly Patients.
DOI: 10.5220/0009088102040208
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 204-208
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Some studies found that mucociliary clearance is
indeed slower in older patients, but with a cut-off of
40-45 years old (Ho, 2001; Paul 2013). This finding
does not have significant relevance in our clinical
settings because almost all patients are above 40
years old, both in outpatient and inpatient settings.
Therefore, this study aims to evaluate the difference
of nasal mucociliary clearance (NMC), measured by
simple saccharin test, in middle-aged (40-59 years)
and elderly (>60 years) patients which are the most
common age groups in our clinical settings.
Nasal mucociliary clearance (NMC) is a mirror
image of bronchial clearance. Ideally, NMC is
measured by using radioisotope, so the physician
will know both the time of NMC and the length of
airway tract. However, the measurement is
expensive and not feasible to be performed in daily
clinical settings (Yadav, 2005). Therefore, in this
study we used saccharin test as a simple test to
measure NMC. Saccharin transit time (STT) was
expected to be longer in elderly patients.
2 METHODS
This is a cross-sectional study held in August
2019 involving middle-aged (n=18) and elderly
(n=12) patients in our outpatient clinic in
Department of Medical Rehabilitation, Cipto
Mangunkusumo National General Hospital,
Indonesia. Consecutive sampling was performed to
recruit subjects. The inclusion criteria were as
follows: (1) patient aged 40-59 (middle-aged group)
or >60 years old (elderly group), (2) no history of
smoking, (3) no respiratory symptoms in the last 2
weeks (runny nose, cough, sore throat, dyspnea).
Subjects were excluded if saccharin transit time
(STT) exceeds 60 minutes because there is a
possibility that the patient has impaired taste
perception if this happens. Drop out criteria is when
subjects could not follow our instruction or refuse to
continue the study during the measurements. Wide
criteria were .purposely used
and subjects with comorbidities were not excluded
so that the subjects in this study reflect real patients
in our clinical settings.
In this study, independent variable is age group
and dependent variable is STT with history of
diabetes and malignancy as confounding factors. We
also measured forced vital capacity (FVC) and
forced expiratory volume in one second
(FEV1)/FVC ratio to see if there were any patients
with obstructive or restrictive lung disease. After
receiving explanation regarding the study and
signing informed consent, subjects in this study were
asked about some data including age, sex, history of
diabetes, malignancy, and any other diseases.
Medical records were also checked to match
patient’s information. Spirometry was then
conducted according to the protocol of American
Thoracic Society (ATS).
Lastly, the saccharin test was performed.
Saccharin particle (+1 mm
3
) was placed about 1 mm
posterior to the anterior border of inferior turbinate.
Subject was asked to flex his head about 10
o
and
breathe normally, but not allowed to sniff, sneeze,
cough, eat, or drink during the test. Subject was then
asked to swallow every 60 seconds. The time taken
by the subject to perceive the sweet taste was noted
as saccharin transit time (STT). All data were
collected and linear regression test was performed to
prove whether age group is an independent factor of
NMC with history of diabetes and malignancy as
possible confounding factors. The conduction of this
study had been previously approved by the Ethical
Committee of Faculty of Medicine, Universitas
Indonesia.
3 RESULTS
Among our subjects, 83.3% (n=25) were female,
16.7% (n=5) had history of diabetes, and 13.3%
(n=4) had history of malignancy. Mean age of
middle-aged and elderly group were 53.44+4.85 and
69.92+7.37 years respectively. Besides FVC which
was found lower in elderly patients (p=0.03), there is
no significant difference in gender, history of
diabetes, malignancy, and FEV1/FVC ratio between
two groups (Table 1). Saccharin transit time (STT)
was not found significantly different (11.9+5.8 vs
12.8+6.3 mins, p=0.696) between middle-aged and
elderly patients using bivariate analysis.
Insignificant Difference of Mucociliary Clearance in Middle-Aged and Elderly Patients
205
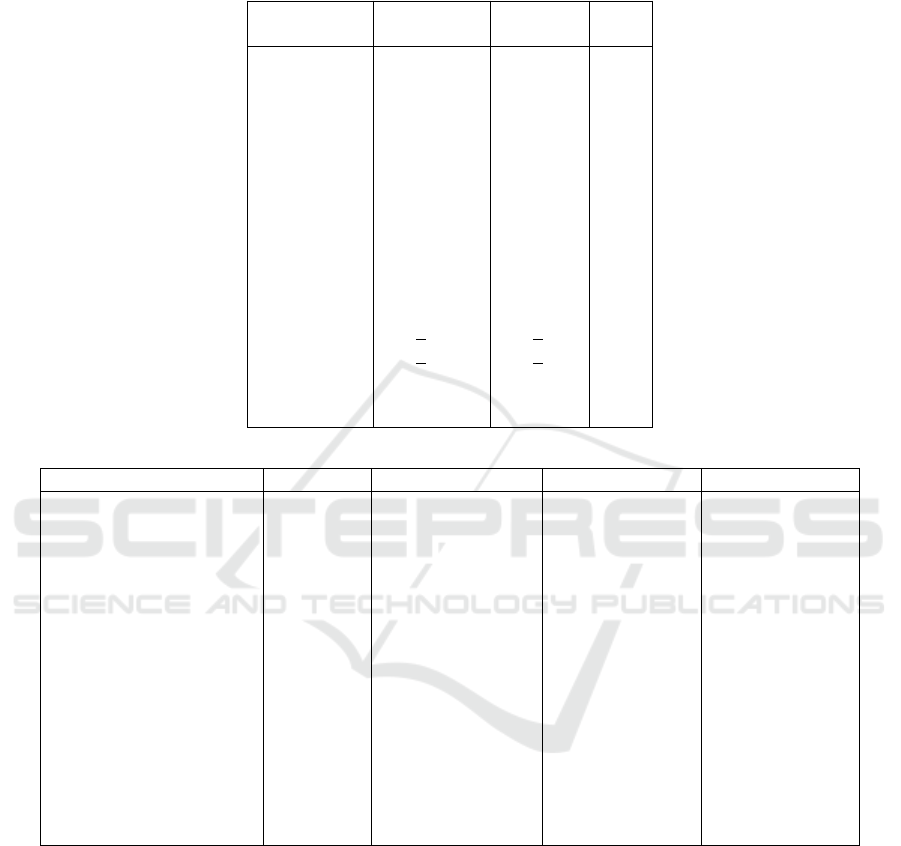
Table 1: Baseline Characteristics of Patient
*Fissher test
**Unpaired t-test
Table 2: Linear Regression of Factors Affecting STT.
β
Standard Error
95% CI
p-value
Model 1
Constant
Age group
History of diabetes
History of malignancy
Model 2
Constant
History of diabetes
History of malignancy
Model 3
Constant
History of malignancy
10.139
1.123
1.889
6.653
10.623
1.954
6.154
10.936
6.329
1.413
2.061
2.524
2.910
1.084
2.486
2.724
1.001
2.695
7.230-13.049
-3.123-5.368
-3.309-7.086
0.660-12.646
8.395-12.851
-3.157-7.065
0.555-11.752
8.882-12.989
0.779-11.860
0.591
0.461
0.031
0.439
0.032
0.026
The analysis was then continued using linear
regression to find the association of age group,
history of diabetes, and history of malignancy
towards STT. At first, none of these factors had
association with STT. The closest one was history of
malignancy (p=0.069), but not statistically
significant. However, it was noticed that a patient
with Bechet’s disease had an abnormally prolonged
STT (26.13 minutes). When this patient was
excluded and linear regression was reperformed, we
found that history of malignancy had a significant
association with STT (p=0.026). When we analyzed
further the patients who had history of malignancy
(n=4), only two of them had prolonged STT (>20
minutes). Further history taking revealed that these
two patients had history of chemotherapy, as
compared to the other two who only underwent
surgery for their cancer.
Variable
Middle-aged
(n=18)
Elderly
(n=12)
p
Gender
- Male
- Female
Diabetes
- Yes
- No
Malignancy
- Yes
- No
FVC (L)
FEV1/FVC
(%)
2
16
3
15
4
14
1.99+0.53
89.0+7.8
3
9
2
9
0
11
1.56+0.41
89.2+10.4
0.364
*
1.000
*
0.268
*
0.03
*
*
0.949
**
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
206

4 DISCUSSION
The reason why it is important to know the
pathophysiology of impaired mucociliary clearance
is that the choice of therapy might differ. For
example, hypertonic saline nebulization is given to
dilute thick mucus, while salbutamol nebulization
(mucokinetic) is used to improve ciliary beat
frequency (Elkins, 2011). If mucociliary clearance is
indeed slower in geriatric patients, mucokinetic
agents might have a role in reducing sputum
retention in elderly patients. However, if it is not the
case, the management should be based on the
condition of the patient rather than the age itself.
In this study we found that mucociliary clearance
is not significantly different in elderly and middle-
aged patients before and after linear regression test.
Possible confounding factors such as respiratory
symptoms, history of smoking, diabetes, and
malignancy have been ruled out or included in
multivariate analysis. This finding is different from
previous studies (Ho, 2001; Paul 2013) which found
significantly different STT in healthy patients below
and above 40-45 years old.
A study (Ho, 2001) especially proved that aging
has a significant correlation with mucociliary
clearance (r=0.64, p<0.001). Similar result, but with
weaker correlation was found in another study (r-
0.324, p<0.001) (Valia, 2008). Based on this data we
suspect that the effect of aging might be subtle so
that significant difference will only be seen in two
groups of patients with wide age gaps. This
deduction is supported by a study (Oliveira-maul
,
2013) (n=252) which found that age has a significant,
but small effect in increasing the risk of having
prolonged STT with the odds ratio of 1.02 (95% CI
1.003-1.033, p=0.015). It has to be noted though that
this study used a cutoff of 12 mins to determine
patients with prolonged STT, while other references
used a cutoff of 20 mins (Deborah, 2014) and even
36 mins (Valia, 2008) for prolonged STT. This
major difference could significantly alter the
calculation of OR. Further study should be
conducted to determine the normal value of STT in
Indonesian patients.
The subjects in this study were recruited with
wide criteria, only excluding patients with
respiratory symptoms and smoking history. The
purpose of this method was to recruit subjects whose
characteristics were as close as possible as real
patients in our clinical settings, as it is rare to find
patients without comorbidities. Diabetes and
malignancy were analyzed as confounding factors
because few studies have found their relation to
mucociliary clearance (Gupta, 2006; Gurung, 2017).
From the baseline characteristics, the subjects in
this study had relatively normal lung function.
Elderly patients were found to have lower FVC, but
it is a normal finding since lung volume has been
widely known to decrease along with age
(Stanojevic, 2008). Other characteristics were not
statistically different between groups. In this study
we also found significantly different STT in patients
who had history of chemotherapy. This finding is in
accordance with the result of a study (Gupta, 2006)
which found that STT in patients with
chemoradiation is significantly longer than patients
with radiotherapy alone (31.68±1.32 vs 28.64±1.88,
p=0.0047). On the other hand, diabetes did not
appear to have significant effect on STT. This
finding is different from the result of a study
(Gurung, 2017) which found that STT was longer in
DM type 2 patients (16.51±2.44 vs 9.96±2.24 mins,
p<0.001). However, this might be caused by the
small number of patients with history of diabetes in
our study, as it is not the main factor that would be
evaluated.
One patient with Bechet’s disease also had
abnormally prolonged STT. A study (Ozbay, 2016)
(n=60) found that NMC was significantly longer in
subjects with Bechet’s disease (13.4+3.3 vs 9.0+1.8
mins, p<0.001). Furthermore, this study also found a
strongly positive correlation between NMC and the
duration of Bechet’s disease (p<0.001, r=0.882).
This finding suggests that there might be other
autoimmune diseases which could also impair
mucociliary clearance.
Regarding the applicability of saccharin test itself,
even though it is a very simple test feasible to be
performed in daily clinical settings, we found that
some patients complained of nose discomfort during
the test. Some patients also firmly refused to be
included in this study because they considered the
test to be invasive, although it had already been
explained thoroughly that the test is not harmful.
The relatively long duration of the test also seemed
to be a problem for the patient. Therefore, we
suggest that unless sputum retention is the main
problem and it is unclear whether the cause is
impaired mucociliary clearance or other factors (e.g.
inadequate cough), it is not recommended to
perform saccharin test as a routine examination for
mucociliary clearance. Physician should focus on
history taking instead regarding possible factors
affecting mucociliary clearance.
The limitations of this study are small sample
size, no random sampling, and no blinding. The
Insignificant Difference of Mucociliary Clearance in Middle-Aged and Elderly Patients
207

subjects of this study were patients visiting our
outpatient clinic for various reasons. If the patient
agreed to be recruited in this study, they would have
to spend more time after the consultation, therefore,
it is somehow difficult to find subjects. The only
confounding factors analyzed in this study were
history of malignancy and diabetes, however, there
might be other confounding factors that we still have
not evaluated, such as structural abnormalities of the
nose, which could not be thoroughly examined in
this study due to limited resources. Nevertheless, we
purposely did not set strict inclusion criteria so that
the patients recruited in this study closely would
reflect real patients in our clinical settings.
In conclusion, no significant STT difference was
found between middle-aged and elderly patients in
this study. Instead, history of chemotherapy and
Bechet’s disease were found to affect STT.
REFERENCES
Baby, M.K., Muthu, P.K., Johnson, P., and Kannan, S.
2014. Effect of cigarette smoking on nasal mucociliary
clearance: a comparative analysis using saccharin test,
Lung India, 31(1), pp.39–42.
Bailey, K.L., Bonasera, S.J., Wilderdyke, M., Hanisch,
B.W., Pavlik, J.A., DeVasure, J., et al. 2014.
Aging
causes a slowing in ciliary beat frequency,
mediated by PKCε. Am J Physiol Lung Cell Mol
Physiol, 306, pp.L584–9.
Bonde, P., Papachristos, I., Mccraith, A., Kelly, B., Wilson,
C., Mcguigan, J.A., et al. 2002. Sputum Retention
After Lung Operation: Prospective, Randomized Trial
Shows Superiority of Prophylactic Minitracheostomy
in High-Risk Patients. Ann Thorac Surg, 74, pp.196-
203.
Deborah, S. and Kim, P. 2014. Measurement of Nasal
Mucociliary Clearance, Clin Res Pulmonol, 2(2),
pp.1019.
Elkins, M.R. and Bye, P.T. 2011. Mechanisms and
applications of hypertonic saline, J R Soc Med, 104,
pp.2–5.
Gupta, S.C., Chandra, S., and Singh, M. 2006. Effects of
irradiation on nasal mucociliary clearance in head and
neck cancer patients, Indian J Otolaryngol Head Neck
Surg, 58(1), pp.46–50.
Gurung, N., Yadav, J., Aggarwal, H.K. 2017. Nasal
mucociliary clearance time in type 2 diabetes mellitus:
a case control study, International Journal of Scientific
Research, 6, pp.51-4.
Ho, J.C., Chan, K.N., Hu, W.H., Lam, W.A.H.K., Zheng,
L., Tipoe, G.L., et al. 2001. The Effect of Aging on
Nasal Mucociliary Clearance, Beat Frequency, and
Ultrastructure of Respiratory Cilia, Am J Respir Crit
Care Med, 163(4), pp.983-8.
Oliveira-maul, J.P., Carvalho, H.B., Goto, D.M., Maia,
R.M., Fló, C., Barnabé, V., et al. 2013. Aging,
Diabetes, and Hypertension Are Associated With
Decreased Nasal Mucociliary Clearance, Chest, 143(4),
pp.1091–7.
Ozbay, I., Kucur, C., Temizturk, F., Ozkan, Y., Kahraman,
C., and Oghan, F. 2016. Assessment of nasal
mucociliary activity in patients with Behçet’s disease,
The Journal of Laryngology & Otology, 130, pp.348–
51.
Paul, P., Johnson, P., Ramaswamy, P., Ramadoss, S.,
Geetha, B., and Subhashini, A.S. 2013. The Effect of
Ageing on Nasal Mucociliary Clearance in Women: A
Pilot Study, ISRN Pulmonology, 598589, pp.1-5.
Marini, J.J. and Formenti, P. 2016. Pathophysiology and
prevention of sputum retention. In: Web A, Angus D,
Finfer S, Gattinoni, L. and Singer, M., eds. Oxford
Textbook of Critical Care, 2
nd
ed, England: Oxford
University Press.
Ramos, E.M.C., Vanderlei, L.C.M., Ito, J.T., Lima, F.F.,
Rodrigues, F.M.M., Manzano, B.M., et al. 2015. Acute
Mucociliary Clearance Response to Aerobic Exercise
in Smokers, Respir Care, 60(11), pp.1575-84.
Rubin, B.K. and Schans, C.P. 2004. Therapy for mucus-
clearance disorders, United States of America: Marcel
Dekker Inc.
Stanojevic, S., Wade, A., Stocks, J., Hankinson, J., Coates,
A.L., Pan, H., et al. 2008. Reference Ranges for
Spirometry Across All Ages A New Approach, Am J
Respir Crit Care Med, 177, pp.253–60.
Valía, P.P., Valero, C., Pardo, M., Rentero, B., and
González, C. 2008. Saccharin Test for the Study of
Mucociliary Clearance: Reference Values for a
Spanish Population, Arch Bronconeumol, 44(10),
pp.540–5.
Yadav, J., Verma, A., and Gupta, K.B. 2005. Mucociliary
clearance in bronchial asthma, Indian J Allergy
Asthma Immunol, 19(1), pp.21-3.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
208
