
Physical Medicine and Rehabilitation Role in Pre-Operative
Management of Patient with Giant Bullae of Right Lung
with Scoliosis and a History of Systemic Lupus Erythematosus:
A Case Report
Andreas Ricky
1
, Tresia Fransiska U Tambunan
2
1
Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo Hospital,
University of Indonesia, Jakarta, Indonesia
2
Cardiorespiratory Division, Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo Hospital,
University of Indonesia, Jakarta, Indonesia
Keywords: Giant Bullae, Systemic Lupus Erythematosus, Pre-operative Management, Pulmonary Rehabilitation
Program.
Abstract: Giant bullae refers to the enlargement of one or more bullae occupying more than one-third of the
hemithorax. It creates larger and less efficient lung sacs that can’t properly manage the normal gas exchange
during breathing. Systemic Lupus Erythematosus (SLE) is a chronic inflammatory disease with pulmonary
manifestations is giant bullae due to excessive surface tension secondary to surfactant failure. Female
patient with history of SLE presenting with shortness of breath during moderate-intensity activities. CT
Scan showed giant emphysematous bullae in her right hemithorax. Patient had double curve scoliosis which
may affect her chest expansion. Evaluation of respiratory functions showed lung restrictive disease and its
predictive post-operative value of forced expiratory volume in one second (ppoFEV1) below 30%. During 8
weeks pulmonary rehabilitation program patient’s clinical state is improved and associated with increase in
forced expiratory volume in one second (FEV1). Home based aerobic exercise consisted of walk 15
minutes/day, 5 days a week. Due to her limited chest expansion, active breathing exercise and scoliosis
program exercise administered in the rehabilitation program. This case report elaborates on the effect of the
pre-operative pulmonary rehabilitation program in improving respiratory function and its readiness to
undergo surgical treatment.
1 INTRODUCTION
Giant bullae, referred to as vanishing lung syndrome
as a clinical syndrome, characterised by large bullae
that occupying at least one-third of one or both
hemithoraces (Huang et al., 2014; Garg et al., 2016).
Emphysema in giant bullae causes a loss of
elasticity in the walls of the small air sacs in the
lung. Eventually, the walls of the sacs stretch and
break, which creates larger, less efficient sacs that
can’t properly handle the normal exchange of
oxygen and carbon dioxide that occurs during
breathing. Difficulty in fully exhaling usually leads
to the capture of air in the lungs, known as
hyperinflation (Giant Bullae. Health Encyclopedi,
2019).
SLE is a chronic inflammatory disease of
autoimmune origin that can affect virtually every
organsystem of the human body (Lopez Velazquez
and Highland, 2018). Pulmonary manifestations of
SLE include airway disease, pleuritis (with or
without effusion), inflammatory and fibrotic forms
of interstitial lung disease (ILD), alveolar
hemorrhage, acute lupus pneumonitis (ALP),
pulmonary hypertension, giant bullae and
thromboembolic disease.
Pulmonary manifestations in systemic lupus
erythematosus (SLE) are relatively common but
giant bullae is the least common clinical
manifestation. Fewer than 100 cases have been
reported in the medical literature. Although giant
bullae can be asymptomatic, patients are usually
experience dyspnea caused by underlying
172
Ricky, A. and Tambunan, T.
Physical Medicine and Rehabilitation Role in Pre-Operative Management of Patient with Giant Bullae of Right Lung with Scoliosis and a History of Systemic Lupus Erythematosus: A Case
Report.
DOI: 10.5220/0009087501720176
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 172-176
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

emphysema. Surgical resection is treatment of
choice for patients with giant bullae. The goals are
to improve the quality of life for those in whom
medical treatment has failed and to resolve
complications while preserving lung function.
Surgical resection is considered only after an
assessment of exercise capacity, pulmonary-function
testing, and smoking cessation. Determination of the
preoperative bulla volume allows the prediction of
the expected increase of postoperative FEV1 (Giant
Bullae. Health Encyclopedia, 2019).
Based on the recommendations of the Enhanced
Recovery After Surgery (ERAS®) and the European
Society of Thoracic Surgeons (ESTS) pulmonary
rehabilitation and prehabilitation is strongly
recommended and so is perioperative nutrition
screening and oral nutritional supplements
(Batchelor, 2019). We report a case of a patient with
giant bullae, scoliosis, and SLE whose pulmonary
function improved significantly after following
prehabilitation program.
2 CASE PRESENTATION
A 43-year-old woman, a nonsmoker presented in
August 2019 with shortness of breath during
moderate-intensity activities. Patient has a history of
giant bullae of her right lung which was diagnosed
on January 2019. Patient started to experience
shortness of breath while conducting regular
activities which gradually worsened. She would feel
shortness of breath after climbing one flight of stairs
although she could still walk 500 meters without the
symptom. Patient also began experiencing fever.
The fever was accompanied with frequent vomiting
and non-productive cough. A chest radiograph (Fig.
1) revealed increased lucency in the upper half of the
right hemithorax suspected as several loculated
pleural effusions. This was followed by a chest
computed tomography (CT) scan that revealed a
giant bullae occupying her right lung accompanied
by pleural effusion on both bases of her lungs.
(Fig.2).
Figure 1: Chest radiograph suspect loculated pleural
effusion in right upper zone, with increased interstitial
markings in lower zone.
Figure 2: CT chest – Giant bullae in right lung, with
loculated pleural effusion and calcified pleura at basal
right lung.
Physical Medicine and Rehabilitation Role in Pre-Operative Management of Patient with Giant Bullae of Right Lung with Scoliosis and a
History of Systemic Lupus Erythematosus: A Case Report
173
Patient has a history of SLE that was first
diagnosed in the year 2000. Afterwards put her in
routine medication (methylprednisolone, myfortic).
In 2006 she began experiencing back pain that
gradually worsened over the time and diagnosed
with osteoporosis. Patient also took kolkatriol and
CaCO3 once a day. The patient denied any history
of tuberculosis, diabetes mellitus type 2, stroke, and
cardiovascular illnesses.
The patients social history; The patient is a
housewife. She was a never smoker, but had
exposure to environmental tobacco smoke. She did
have any exposure to biological or industrial dusts.
Therewas no family history of respiratory illnesses.
On examination, she had a heart rate of 99 beats
per minute, and a blood pressure of 140/94. The
respiratory rate was 21 breaths per minute, with an
oxygen saturation of 97% on ambient air. She was of
small build with BMI 16,4 (underweight).
Respiratory examination revealed a vesicular breath
sounds, with reduced sound on the right hemithorax,
no rhonchi, no wheezing. Hypersonor was found in
lateral right hemithorax during chest percussion. She
had thoracoabdominal breathing pattern, with
contraction of inspiratory accessory muscle, slightly
delayed chest expansion on right hemithorax, and
inadequate effort to cough. Chest expansions were
decreased, with a difference between inspiration and
expiration of 5.
In postural examination, patient left shoulder is
slightly higher than the right, vertebral alignment S-
shaped with convexities on left mid-thoracic region
and right thoracolumbar region, pelvic obliquity
positive with right side higher than the left, very
slightly observable hump on right mid-thoracic
region of the vertebrae. Spasm paravertebral muscles
was found on the concave side. Schober test is 15 +
4 cm, and with Adams test showed a functional
scoliosis with hump (height 1 cm) on right side of
mid-thoracic region (T6) 6 cm from midline.
Patient was consulted for a rehabilitation
program as the patient is waiting for surgery. Pre-
operative management aimed to increase
cardiorespiratory endurance, strengthening of
diaphragm muscle, increase chest wall mobility,
reduce muscle imbalance due to scoliosis, energy
conservation, and improve nutritional status.
Table 1: Baseline lung function and capacity test.
Chest Expansion 5cm – 5 cm – 6cm
PFR 2.70 L/s
FVC 1.09 L (32% pred)
FEV1 1.00 L (36% pred)
FEV1/FVC 91.74%
6MWT
Mileage: 418 meter
(predicted mileage
514.2 meter) =
81.29%
Vo2Max: 16.8
METS: 4.80
Chest Expansion 5cm – 5 cm – 6cm
Table 2: Lung Function and capacity test after
rehabilitation program.
4 weeks 8 weeks
Chest
Expansion
5cm – 5 cm –
8cm
5cm – 5 cm –
8cm
PFR 3.31 L/s 3.74 L/s
FVC
1.9 L
(66% pred)
2.59 L
(86.9% pred)
FEV1
1.71 L
(69.5% pred)
2.20 L
(87% pred)
FEV1/FVC 90% 84.94%
6MWT
Mileage: 409
meter (predicted
mileage 518,6
meter) =
78.86%
Vo2Max: 15.4
METS: 4.4
Mileage: 465
meter (predicted
mileage 517
meter) = 89.2%
Vo2Max: 18.4
METS: 5.20
3 DISCUSSION
Giant bullae is a disorder characterized by bullae
occupying more than a third of the hemithorax, and
mostly affects men who are smokers (Kiang, Tan
and Li, 2015) In our case, although the she never
smoked a day in her life, the patient was exposed to
cigarette smoke since childhood as her late father
was a heavy smoker. In addition, nowadays she
lives by a garbage disposal site that burns garbage
on a daily basis. Thus, it may not be unreasonable to
assume that different triggers incite the same
cascade of subcellular inflammatory mediators that
cause the destruction of alveolar walls and resulting
in permanent and abnormal enlargement of distal
airspaces. Interestingly, GB in our patient may have
and associations with medical conditions (and
systemic lupus erythematous), (Kiang, Tan and Li,
2015)
Enlarging bullae cause symptoms by interfering
with respiratory mechanics and gas exchange. As
they grow larger, they compress on normal lung
parenchyma, reduce lung compliance, and increase
work of breathing. As dead space fraction increases
with bullae formation, gas exchange is also impaired
This symptom similar in our setting that showed
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
174
dyspnea was the main problem, and pulmonary
functional study showed restrictive lung disease.
Patient with single giant bulla with underlying
normal lung is the “ideal candidates” and stand the
best chance of success of surgery. Success is defined
as both a lessening of the pressure and other
symptoms, and the recovery or restoration of lung
function.(Giant Bullae. Health Encyclopedia, 2019)
It is still uncertain whether the patient in this case
falls in this category. Even with a single giant bulla
and remaining lungs mostly in normal condition, the
CT result showed a fibrosis in segment 9 of left lung
accompanied by pleural effusion. In addition the
single giant bulla was formed by combination of
multiple giant bulla existed in the right lung with the
size of approximately 11.4 x 6.7 x 17.6 cm3.
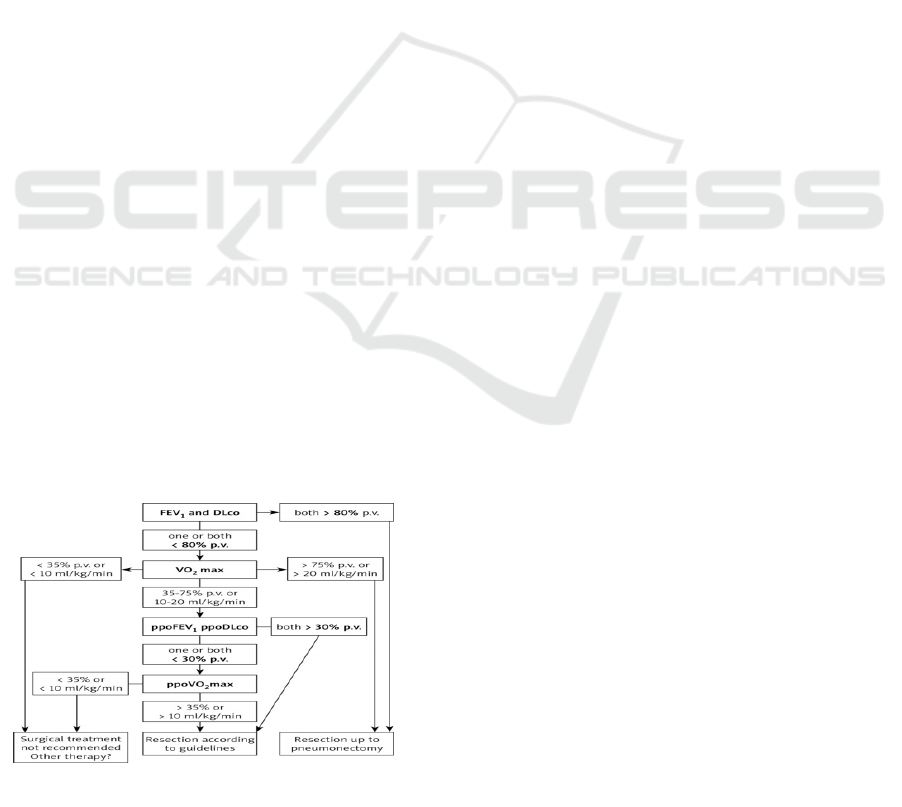
Before planned surgical treatment of lung cancer,
the patient's respiratory system function should be
evaluated. According to the current guidelines (fig
3), the assessment should start with measurements of
FEV1 (forced expiratory volume in 1 second) and
DLco (carbon monoxide lung diffusion capacity).
Pneumonectomy is possible when FEV1 and DLco
are > 80% of the predicted value (p.v.). If either of
these parameters is < 80%, an exercise test with
VO2 max (oxygen consumption during maximal
exercise) measurement should be performed. When
VO2 max is < 35 % p.v. or < 10 ml/kg/min,
resection is associated with high risk. If VO2 max is
in the range of 35-75% p.v. or 10-20 ml/kg/min, the
postoperative values of FEV1 and DLco (ppoFEV1,
ppoDLco) should be determined. The exercise test
with VO2 max measurement may be replaced with
other tests such as the shuttle walk test and the stair
climbing test. The distance covered during the
shuttle walk test should be > 400 m. Patients
considered for lobectomy should be able to climb 3
flights of stairs (12 m) and for pneumonectomy 5
flights of stairs (22 m).(Trzaska-Sobczak, M
Skoczyński and Pierzchała, 2014)
Figure 3: Algorithm for assessing respiratory system
function in lung cancer surgery candidates.
In this patient the ppoFEV1 was 15 pv and
ppoVO2 max was 6.73 ml/kg/min which means
surgical treatment was not advised and other therapy
was recommended. In 21 studies (including 5 RCTs)
focusing on pre- rather than postoperative
rehabilitation, the intervention was delivered mainly
in the outpatient setting or in a training facility.
Prescribed exercises included aerobic training (lower
and/or upper limbs), with the addition of strength
training in some studies. Respiratory exercises were
also included in the majority of studies. The addition
of other elements, such as relaxation techniques and
educational sessions, were inconsistent. The median
duration was 4 weeks (range 1–10 weeks) with a
frequency of 5 sessions per week (range 2–
14 weeks) of moderate to high intensity, generally
tailored to the patient’s tolerance.(Batchelor, 2019)
This patient receives pre-operative pulmonary
rehabilitation program in outpatient setting which
includes: (1) aerobic exercise 5 times a week, (2)
respiratory exercises, and (3) exercise program for
scoliosis. Aerobic exercise prescribed for moderate
intensity although in reality the patient was allowed
to do them as tolerated. Based on her 6-minute-
walking-test result which was 418 meters in 6
minutes (VO2 max 16.8, METs: 4.80), we decided
to prescribe her aerobic exercise starting from 50%
of the maximum walking distance from her 6MWT,
thus ideally prescribing the patient with 30 minutes-
walk (with the same pace as when she walked the
6MWT) for 3 days a week. However, as the patient
has had a history of SLE with multiple
musculoskeletal manifestation in addition to her
sedentary lifestyle, we made the decision to
prescribe her aerobic exercise that started low and
progress slowly starting with walking for 15
minutes, 5 days a week, instead.
As for her respiratory exercise, the patient
receives a set of exercise that consisted of
diaphragmatic breathing, deep breathing, chest
expansion, and pursed lip breathing. Aside from
relaxation effect the exercise may give to the patient
each one was prescribed for different reasons. As
the right hemithorax could not expand
symmetrically with the left one, thoracic expansion
could be assisted by excursion of the diaphragm and
flexing and abducting the upper extremities. If the
patient were to follow through with surgery later on,
the patient would be prepared with diaphragm and
intercostal muscles that has good strength and
flexibility. She would also benefit from the
relaxation breathing when experiencing post-
surgical pain. While pursed lip breathing helps in
airway clearance as the patient has limited
Physical Medicine and Rehabilitation Role in Pre-Operative Management of Patient with Giant Bullae of Right Lung with Scoliosis and a
History of Systemic Lupus Erythematosus: A Case Report
175

inspiratory capacity. In addition, patient was also
prescribed 2 session of chest physical therapy
aiming to educate her chest mobility exercise.
Moreover, a TheraBand strengthening exercise is
also planned to strengthen her pectoralis mayor and
core muscles that may help with overall recovery.
Scoliosis exercise programs were aimed to
correct the muscle imbalance. It consist of (1)
strengthening weakened muscles on the convex side,
(2) stretching of muscle spasm on concave side with
6 seconds hold, 10 repetitions, 3-5 times/day.
ESPEN guidelines recommend delaying surgery to
allow for preoperative enteral nutrition in patients
with at least one of the following criteria: weight
loss >10–15% within 6 months, body mass index
(BMI) <18.5 kg/m2 and serum albumin <30 g/l (with
no evidence of hepatic or renal dysfunction).
Current general recommendations suggest
administration of 5–7 days of oral supplements
before surgery in patients at risk of
malnutrition.(Batchelor, 2019)
In this case the patient’s BMI falls less than 18.5
kg/m2, and there hasn’t been any lab work up to rule
out hepatic nor renal dysfunction considering
patient’s history of SLE. Patient is planned to be
consulted to nutritionist regarding her perioperative
nutrition preparation. 4 weeks after home-based
program the chest expansion is increase in lower
segment. And also increasing in pulmonary function
test, ppoFEV1 29 pv, and ppoV02max 6.16
ml/kg.min. After 8 weeks of program FEV1 is
increased to 2.20 L (87% pred), so does the
ppoFEV1 (36 pv) and ppoVo2max (7.37 ml/kg.min)
(table 2). Although patient still was not advised to
undergo surgical treatment, better pulmonary
function already help patient to do her daily activity.
Patient right now can climb 2 flights of stairs
without feeling any shortness of breath, and can do
housework without any symptoms.
4 CONCLUSIONS
Pulmonary rehabilitation can be given to patient
with giant bullae in pre-operative setting. This will
lead to better cardiorespiratory endurance,
respiratory function, and better endurance to do her
daily activity. Pre-operative pulmonary
rehabilitation program should be given to the giant
bullae patient to increase her readiness to undergo
surgical treatment.
REFERENCES
Batchelor, T., 2019 Guidelines for enhanced recovery after
lung surgery: recommendations of the Enhanced
Recovery After Surgery (ERAS®) Society and the
European Society of Thoracic Surgeons (ESTS), Eur J
Cardiothorac Surg, 55(1), pp. 91–115. doi:
https://doi.org/10.1093/ejcts/ezy301.
Garg, I. et al., 2016. Giant Bulla or Tension
Pneumothorax: Diagnostic Dilemma in Emergency.
Chest, 150(4), p. 929A. doi:
10.1016/j.chest.2016.08.1029.
Giant Bullae. Health Encyclopedia, 2019. University of
Rochester. Available at:
https://www.urmc.rochester.edu/encyclopedia/content.
aspx?contenttypeid=22&contentid=giantbullae.
Accessed: 19 August 2019.
Huang, W. et al., 2014. Surgery for giant emphysematous
bullae: case report and a short literature review, J
Thorac Dis, 6(Mvv), pp. 104–107. doi:
10.3978/j.issn.2072-1439.2014.04.39.
Kiang, C., Tan, R. and Li, Y., 2015. Respiratory Medicine
Case Reports A breath from Houdini e A case of giant
bullous emphysema, Respir Med Case Rep, 14, pp.
30–33. doi: 10.1016/j.rmcr.2014.12.003.
Lopez Velazquez, M. and Highland, K., 2018. Pulmonary
manifestations of systemic lupus erythematosus and
Sjögrenʼs syndrome. Curr Opin Rheumatol. doi:
10.1097/bor.0000000000000531.
Trzaska-Sobczak, M Skoczyński, S. and Pierzchała, W.,
2014. Pulmonary function tests in the preoperative
evaluation of lung cancer surgery candidates. A
Review of Guidelines. Kardiochir Torakochirurgia
Pol, 11(3), pp. 278–82. doi:10.5114/kitp.2014.45677.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
176
