
The Description of Lung Function in Stable Chronic Obstructive
Pulmonary Disease (COPD) Patients after Following Respiratory
Muscles Training based on Assessment of Peak Expiratory Flow Rate
and Chest Expansion
Putri Alfaridy Lubis
1
, Octariany
2
, Fanny Indah Prammita
3
1
Department of Physical Medicine and Rehabilitation, Aulia Hospital, Pekanbaru, Riau
2
Department
of Pulmonology, Aulia Hospital, Pekanbaru, Riau, Indonesia
3
General Practitioner, Aulia Hospital, Pekanbaru, Riau, Indonesia
Keywords : Chronic Obstructive Pulmonary Disease (COPD), Respiratory Muscles Training, Peak Expiratory Flow
Rate (PEFR), Chest Expansion (CE)
Abstract : This study aimed to evaluate the effect of respiratory muscles training to peak expiratory flow rate (PEFR)
and chest expansion (CE) in COPD patients and to provide new information about the effect of a short
training program (only 4 weeks) on respiratory function. It was 4-weeks experiment with pre and post
design. Six stable COPD patients have enrolled to this study. Respiratory muscles training consisted of
expiratory muscles training, inspiratory muscles training, and breathing excercise. In this study found that
all levels of CE increased after respiratory muscles training. The average of upper CE increased from 2.3 cm
to 5.3 cm (p 0.000), the average of middle CE increased from 4.5 cm to 6.2 cm (p 0.011), and the avarage of
lower CE also increased from 4.2 cm to 6.5 cm (p 0.005). The average value of PEFR also increased from
267.7 L/min to 319.3 L/min (increased 19%, p 0.046). This study found a significant improvement on CE
and PEFR value after following short respiratory muscles training (only 4 weeks). The training in this study
can be an option for management of COPD to improve patient’s health outcomes.
1 INTRODUCTION
Chronic Obstructive Pulmonary Disease (COPD) is
a chronic disease. The characteristics of this disease
are persistent respiratory symptoms and airflow
limitation. Patients with COPD are often
hospitalized due to exacerbations (Dhamane et al,
2015). After an exacerbation, a patient may
experience a degradation of functional ability and
impaired quality of life. (Shah et al, 2016).
COPD is a systemic inflammatory disease, it can
cause repercussion on several systems like skeletal
muscle dysfunction and weight loss (Barreiro &
Gea, 2015; Lee et al, 2017). Changes in body
composition that result in a reduction in muscle mass
which leads to atrophy in all muscle fibers,
decreasing muscle oxidative capacity, and making
muscles more prone to fatigue (Man et al, 2009).
Muscle fatigue caused by the deleterious effect
of COPD may compromised respiratory muscle
function (Barreiro & Jaitovich, 2018). Among the
respiratory muscles involved, the diaphragm is
mechanically disadvantaged due to airway
obstruction and lung hyper insufflation (Rocha et al,
2017). The mechanical detriment of the diaphragm
associated with loss of mass can lead to reduce
diaphragm movement, therefore contributing to
respiratory distress and exercise intolerance
(Barreiro & Gea, 2015).
The guideline from The Global Strategy for the
Diagnosis Management, and Prevention of COPD
and Global Initiative for Chronic Obstructive Lung
Disease (GOLD) 2018 explains the steps to reduce
symptoms and risk factors which can aggravate the
disease. One of the steps is pulmonary rehabilitation
program (Vaes et al, 2018)
154
Lubis, P., Octariany, . and Prammita, F.
The Description of Lung Function in Stable Chronic Obstructive Pulmonary Disease (COPD) Patients after Following Respiratory Muscles Training based on Assessment of Peak Expiratory
Flow Rate and Chest.
DOI: 10.5220/0009066601540161
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 154-161
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

The success of pulmonary rehabilitation in
COPD patient has been demonstrated in several
studies (Houchen-Wollof et al, 2017). Although
pulmonary rehabilitation is a multi-dimensional
therapy, muscle training appears to be its most
effective component. As mentioned in several
studies, expiratory muscles have been found to be
active in COPD patients both at rest and during
exercise, mostly at the end of expiration.
Unfortunately, there are not enough studies that
explained about the benefit of short-term expiratory
muscle training program on lung function (Mota et
al, 2005).
The main program is associated with the chief
complain that it has disturbed the daily activity and
caused the lack of productivity, such as dyspnea and
excessive sputum production. Increased sputum
production is a common feature of COPD that
frequently require initiation of early therapy to
decrease its impact upon clinical outcomes (Langer
et al, 2009; Sahin et al, 2016). Prescription of
mucolytic and/or mucoactive agents may target
reductions in sputum viscosity, concurrently with
non-pharmacological therapies like airway clearance
techniques (ACTs). There are many types of ACTs
used in clinical practice, including breathing
exercise such as active cycle of breathing technique
(ACBT), autogenic drainage, and hand-held positive
expiratory pressure (PEP) devices such as mask,
mouthpiece or oscillatory PEP. Coughing is
involved in ACTs (Osadnik CR et al, 2015).
Not all coughs are effective in clearing excess
mucus from the lungs. Explosive or uncontrolled
coughing induces airways to collapse and spasm,
trapping mucus. The effective or controlled cough
comes from deep within the lungs and has just
enough force to loosen and carry mucus through the
airways without causing them to narrow and
collapse. Controlled coughing saves energy and
therefore, oxygen (Osadnik CR et al, 2015)
We modified the exercise to train respiratory
muscles and taught the patients to cough effectively.
We trained expiratory muscles with Positive
Expiratory Pressure (PEP) device. Inspiratory
muscles were trained with LVR method which was
performed with insufflation technique which used a
simple hand-held resuscitation bag, and the ACTs
was performed with breathing exercise as called as
Active Cycle of Breathing Technique (ACBT). This
cycle of exercise was performed to improve lung
function which could be assessed by the values of
peak expiratory flow rate and chest expansion.
(Malaguty et al, 2009; Ozgocmen et al, 2014;
McKim et al, 2011).
The aim of this present study was to evaluate the
effect of respiratory muscles training on Peak
Expiratory Flow Rate (PEFR) and Chest Expansion
(CE) in COPD patients, and to provide new
information about the effect of a relatively short
training program (only 4 weeks) on respiratory
function. This outcomes can be considered as the
major short-term targets in the treatment of COPD
patients.
2 METHODS
This was 4 weeks experiment with pre and post
design. We collected the subjects with purposive
sampling method. This study was carried out in
Aulia Hospital, Pekanbaru, Riau, Indonesia.
2.1 Ethic and Subjects
Study participants provided written informed
consent to a potocol approved by Aulia Hospital
ethical committees. Thirty COPD patients visited
Aulia Paru Center a month before we did the
research. We predicted these patients would come
back to meet pulmonologist to control their disease.
Only 18 patients met the inclusion and exclusion
criteria. Twelve patients refused to follow this study
due to some reasons. So, we prospectively recruited
6 patients with mild to severe COPD admitted to our
Pulmonology Center dedicated outpatient between
June 24th until July 13th 2019.
2.2 Inclusion and Exclusion Criteria
The inclusion criteria were as follows: 35-65 years
of age, FEV1 more than 30% predicted, FEV1/FVC
ratio <0.7, not having an exacerbation, taking
medicine from pulmonologist regularly, and the
patients agreed to follow this study. Exclusion
criteria were severe exacerbation of COPD or the
hospitalization for COPD within 4 weeks
recruitment, the patients who suffered cardiac
disease, cor-pulmonale disease, joint disorder,
rheumatoid arthritis, neurologic disorder, cognitive
disorder which was assessed by Mini Mental State
Exam (MMSE), and inability to comply with study
procedures or the rejection from the patient to attend
the study.
2.3 Study Design
This study consisted of a screening visit and 2 weeks
of optimalization of medical therapy from
The Description of Lung Function in Stable Chronic Obstructive Pulmonary Disease (COPD) Patients after Following Respiratory Muscles
Training based on Assessment of Peak Expiratory Flow Rate and Chest
155

pulmonologist. The patients were scheduled to
follow the program 3 sections in a week for 4 weeks.
Every section needed 20-30 minutes.
Patients who met inclusion criteria on screening
visit (following from clinical manifestation and
confirmed by spirometry testing) were enrolled and
instructed to register all data during the study period.
Values of lung function were assessed by PEFR and
CE. These values were assessed before program, in
the first, second, third, and fourth week of the
program.
2.4 Measurements and Outcomes
At registration, patient’s anthropometric and
physiological characteristics were recorded.
Respiratory measurements included short of
breathing (dyspnea), cough and sputum scale, as
well as health status assessment evaluations and
respiratory functions like FVC, FEV1, FEV1/FVC,
FEF 25 %predicted, FEF 50 %predicted, PEFR and
CE.
Diagnosis and severity of COPD have been
confirmed by using GOLD Guidelines. Respiratory
function test (FVC, FEV1, FEV1/FVC, FEF 25
%predicted, FEF 50 %predicted) was assessed using
CHEST SPIROMETER type HI-105 that has been
calibrated before conducting the study. Each patient
was sitting during spirometry test. They were asked
to blow into the straw and measurement of FVC,
FEV1, FEV1/FVC, FEF 25 %predicted, FEF 50
%predicted were recorded.
2.4.1 Chest Expansion Measurement
A measuring tape was used to measure chest
expansion (CE) in centimeters (cm) at three levels of
the rib cage. For upper CE, the anatomical markers
were the 3rd intercostal space (front aspect) and 5th
thoracal spinosus process (back aspect) to measure
lung expansion for upper and medial lobe. For
middle CE, the 4th intercostal space (front) and 6th
thoracal spinosus process (back) was expected to
predict lung expansion in medial lobe, while
xyphoid process (front) and 10th thoracal spinosus
process (back) was measured as lower CE to predict
expansion in lower lobe (Reddy et al, 2019; Mulyo
et al, 2015). The measurement was held by one
person to all patients from the beginning until the
end of the program.
2.4.2 Instructions to Subjects
The instruction given by the examiner to patient
during breathing was standardized. Prior to the
thoracic measurement, patients were asked to
“inhale slowly and rhythmically through the nose
against the measuring tape to open up the lung as
much as you can”, and then the patients were asked
to “exhale through the mouth completely.” CE
measurement was taken at the end of the inspiration
and expiration cycle. The patients were in a standing
position with their arms were at the side of their
body. The examiner placed the “0” point of the
measuring tape on the back aspect. Holding
measuring tape was standardized by crossing the
tape close to the skin. The measurement was taken
three times, and the mean of these values was
collected for each levels.
2.4.3 Peak Expiratory Flow Rate (PEFR)
Measurement
The PEFR measurement was performed using a
Philips respironic peak flow meter. The best PEFR
was adopted from three correct blows when patients
exerted maximal expiratory efforts in a sitting up
straight position. We calculated the average of three
values of PEFR on each patients. PEFR
measurement was collected before training. We
evaluated this value on the first, second, third, and
fourth week of the training.
2.5 Respiratory Muscles Training
2.5.1 Expiratory Muscles Streghtening
This training used PEP device (PHILIP
RESPIRONIC threshold PEP) to train expiratory
muscles. We asked patient to put nose clip on nose,
breathe through mouth, seal lips around mouthpiece,
take a full breathe in and breathe out 2 or 3 times
longer than breathe in. Due to the absence of
respiratory pressure meter, we modified the
technique to determine initial dose of treatment.
We started from the lowest number of resistance
dose and asked patients to continue this pattern for
10 times. We increased the dose and assessed the
patient’s degree of dyspnea by using BORG Scale.
A higher number equals greater effort. When the
patients were unable to complete 10 Repetitive
Movement (RM), initial dose was determined by
80% of the last dose that patient could complete 10
RM correctly. We took this exercise for 3 sets, 1 set
consisted of 10 RM and it took 30-60 seconds to rest
before continuing the next set.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
156
2.5.2 Lung Volume Recruitment (LVR)
The second exercise was Lung Volume Recruitment
(LVR) to train inspiratory muscles. This method was
performed with insufflation technique which used a
simple hand-held resuscitation bag. The patient was
ordered to breathe in through the mask slowly while
the instructor squeezed the bag 3 times, and then the
patient was asked to cough effectively 3 times. We
took this method for 3 sets, 1 set consisted of 3 RM,
and it took 30-60 seconds to rest before continuing
the next set.
2.5.3 Breathing Exercise
The last was breathing exercise which was called as
ACBT technique. It consisted of 3 stages. There
were breathing control, thorax expansion exercise,
and forced expiratory technique. Each stage was
repeated for 5 times and ended with cough
effectively. This cycle was repeated for 3 times, and
it took 30-60 seconds to rest before continuing the
next set.
3 RESULTS
3.1 Demographic Data
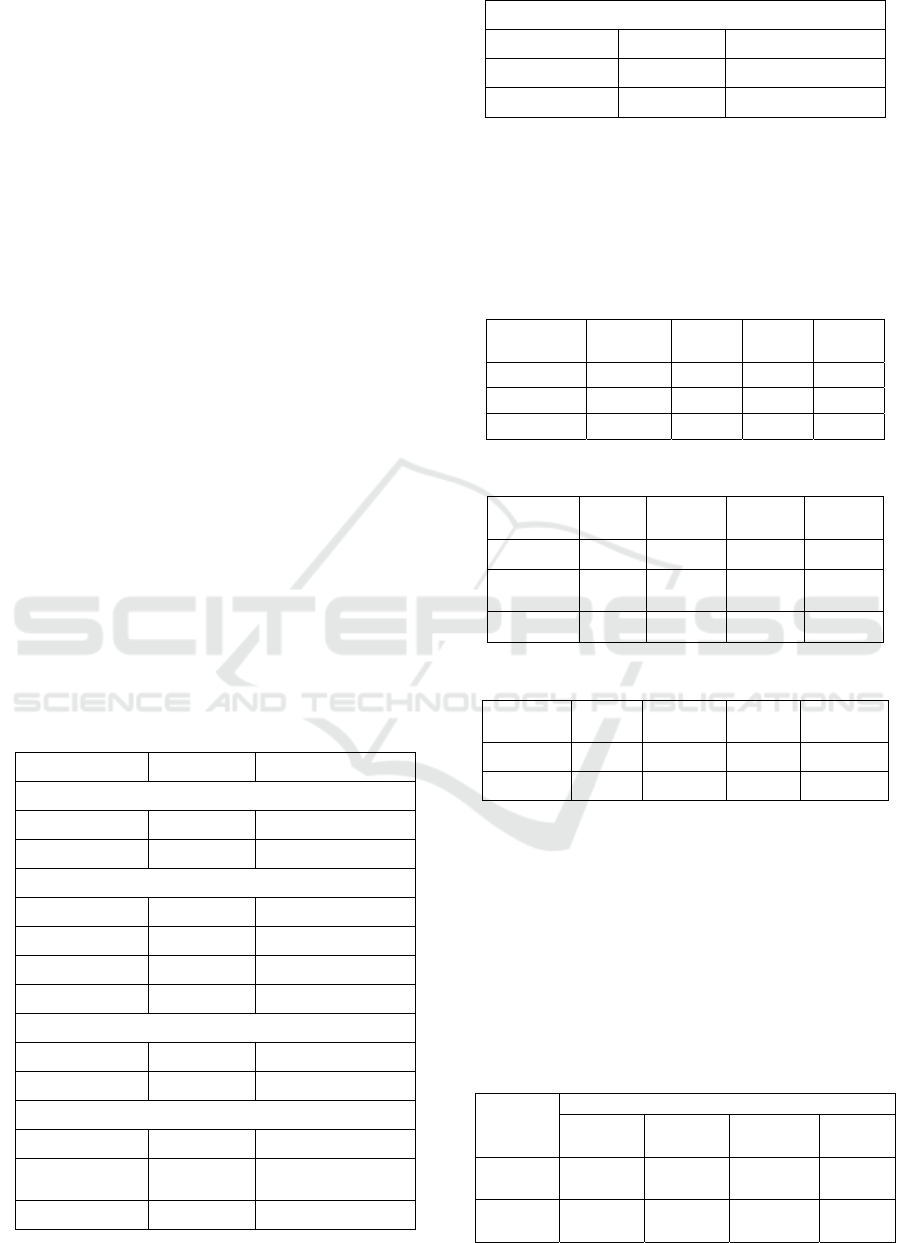
Demographic data were shown in Table 1.
Table 1: Demographic data.
Variables n %
Sex
Male 6 100
Female 0 0
Age
45-50 2 33.3
51-55 0 0.0
56-60 0 0.0
61-65 4 66.7
History of smoking
Yes 5 83.3
No 1 16.7
Brinkman Index
<200 (Mild) 2 40
200-600
(Moderate)
3 60
>600 (Severe) 0 0
Staging of COPD
Mild 1 16.7
Moderate 3 50.0
Severe 2 33.3
3.2 Chest Expansion (CE), Peak
Expiratory Flow Rate (PEFR), and
Spirometry Test
These data were shown in table 2-4.
Table 2: CE value before respiratory muscle training.
Pre
Training
Mean SD
Minim
um
Maxi
mum
Upper CE 2.33 0.516 2 3
Middle CE 4.50 1.049 3 6
Lower CE 4.17 0.753 3 5
Table 3: CE after respiratory muscle training.
Post
Training
Mean SD
Mini-
mum
Maxi-
mum
Upper CE 5.33 0.516 5 6
Middle CE 6.17 0.408 6 7
Lower CE 6.5 0.548 6 7
Table 4: PEFR Value.
(PEFR) Mean SD
Mini-
mum
Maxi-
mum
Pre 267.6 99.725 120 370
Post 319.5 136.141 133 476
3.3 Changes Test Between Upper,
Middle, Lower CE, and PEFR
Before and After Training
Results from Paired T Test showed significant
changes between upper, middle, lower CE, PEFR
value before and after training. These results were
shown in table 5.
Table 5 : Paired T-Test Between Upper, Middle, Lower
CE, and PEFR Before and After Training.
Before
Training
After Training
Upper
CE
Middle
CE
Lower
CE
PEFR
Upper
CE
p= 0.000
Middle
CE
p= 0.01
The Description of Lung Function in Stable Chronic Obstructive Pulmonary Disease (COPD) Patients after Following Respiratory Muscles
Training based on Assessment of Peak Expiratory Flow Rate and Chest
157

0
2
4
6
8
AR S J Z L EK
Pre Week1 Week2 Week3 post
Lower CE p= 0.005
PEFR p= 0.046
3.4 Post Respiratory Muscle Training
Measurement
We evaluated the training based on the values of CE
and PEFR. These values were increase after training.
The enhancement of these values were shown in
figure 1-6. Evaluation of spirometry test was shown
in figure 7.
Figure 1 : Evaluation of Upper CE Every Week.
Figure 2 : Evaluation of Middle CE Every Week.
Figure 5: Evaluation of PFM Every Week.
0
100
200
300
400
500
600
AR S J Z L EK
Pre Week1 Week2
Week3 Post
0
2
4
6
8
AR S J Z L EK
Pre Week1 Week2 Week3 Post
0
2
4
6
8
UpperCE MidleCE LowerCE
Pre Week1 Week2 Week3 Post
Figure 4 : Average of CE Expansion Every
Week.
0
2
4
6
8
AR S J Z L EK
Pre Week1 Week2 Week3 Post
Figure 3 : Evaluation of Lower CE Every
Week.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
158

Figure 6: Comparison of PFM (Pre and The Average
During Program).
Figure 7: Comparison of spirometry test (pre and post
training).
4 DISCUSSIONS
The main finding of this present study is the
improvement in CE and PEFR in COPD patients
after following a short respiratory muscles training
period (only 4 weeks). Although the study on
respiratory muscles only a few, it is known that in
COPD patients these muscles can exhibit weakness,
as evidenced by either mild reduction in maximal
force and/or endurance (Weiner et al, 2003). Since
muscle weakness might be improved through
different mechanisms by training, our hypothesis is
that specific respiratory muscles training program
using an appropriate schedule would promote
clinical benefits. This study was designed to respond
to the relative lack of information about the impact
of respiratory muscles training on respiratory
function.
Previous study showed CE measurements
significantly correlate with lung function parameters
(FVC, FEV1, FEV1/FVC, and VC). Therefore
maintaining chest wall mobility may be an important
element for preserving FVC and FEV1/FVC in
elderly male patients with COPD. There was a
reduction of chest expansion value in COPD patients
which compared with healthy nonsmoker (Reddy et
al, 2015). Mean value of upper chest expansion in
healthy subjects was 6.2 cm, 6.86 cm for middle
chest expansion, and 7.25 cm for lower chest
expansion (Mulyo A.N.D et al, 2015). Debouche et
al found the mean of upper CE in young healthy men
was 5.9 cm and 7.1 cm for the lower CE (Debouche
et al, 2016). Reddy et al found mean value of upper
CE was 3.7 cm and 4.9 cm for lower CE in COPD
patients. Our study has similar finding that the mean
value of upper CE was 4.5 cm, 4.1 cm for middle
CE, and 4.96 cm for lower CE before training.
The reduction of CE value in this study may
because patients with respiratory problems like
COPD may present with abnormalities in chest
biomechanics. Rib cage mobility might be decreased
as a consequence of airway obstruction and
hyperinflation which happened in COPD patients
(Debouche et al, 2016). The normal range of CE
tends to decline with age (decline up to 50-60%
between ages 15 and 75 years) and to be 20% greater
in men (Lanza FC et al, 2013), which also explained
the low mean of CE in our study, because the
subjects in our study were between 45-60 years old
and all the subjects were male.
Currently, PEFR reduction was one of the most
common alternative tools suggestive of the presence
of airflow limitation and employed in COPD case-
finding studies (Martinez et al, 2017). Normal
individuals may produce a PEFR as great as 720
L/min and occasionally higher in healthy individuals
(Homnick DN, 2007). Su et al found that PEFR
value range in non COPD subjects was 472±113
L/min, while in COPD patient, the range was 290
±120 L/min (Su et al, 2018). Similarly with our
study which also found the reduction of PEFR value
in COPD patients before respiratory muscles
training. We found that the mean value of PEFR was
267.6 L/min. Sivasothy et al suggested that
premature peripheral airway closure, exacerbation of
hyperinflation with insufflation, or induced
bronchoconstriction might have contributed to the
reduced PEFR and volumes in the patients with
COPD (Sivasothy, 2001).
0
50
100
AR S J Z L EK
SpirometryTest
FEV1%PREDICTEDBEFORETRAINING
FEV1%PREDICTEDAFTERTRAINING
FVC%PREDICTEDBEFORETRAINING
FVC%PREDICTEDAFTERTRAINING
0
100
200
300
400
500
AR S J Z L EK
Pre AvarageDuringProgram
The Description of Lung Function in Stable Chronic Obstructive Pulmonary Disease (COPD) Patients after Following Respiratory Muscles
Training based on Assessment of Peak Expiratory Flow Rate and Chest
159

We found improvement of CE and PEFR
measurement after respiratory muscles training in
every patient. Increasing of CE happened in every
level. The mean value of upper CE became 5.33 cm
(p 0.000), middle CE became 6.17 (p 0.011), and
lower CE became 6.5 cm (p 0.005). The
improvement of PEFR value from 267.6 L/min to
319.5 L/min (p 0.046). Abdominal muscle is critical
during expiration, such as forced expiration and
coughing.
Wang et al reported that the FVC% and FEV1%
in two groups were improved compared with that
before breathing training (Wang et al, 2019).
Contrary with our study, not all patients showed
enhancement of FVC% and FEV1%, and PEFR
value after training in our study also did not show a
normal value. This might be because that respiratory
muscles
training helps slow down or stop the disease
progression, but cannot reverse the lung lesions that have
occurred.
There were significant changes when we
observed the value of upper, middle, lower CE, and
PEFR before and after attending the program. These
data can become preliminary data for futher research
which can collect larger amount of subjects
.
5 CONCLUSIONS
Our study found significant improvement on
respiratory functions which were assessed by CE
and PEFR value after following short respiratory
muscles training (only 4 weeks). Thus, this training
in this study can be an option for management of
COPD to improve patient’s health outcomes.
Guidelines for the referral of patients with COPD to
pulmonary rehabilitation recommend referral of
those who are motivated, medically stable, and
symptomatic with impairment in daily activities.
In our experience, this sort of training is easy to
incorporate into clinical practice and has no adverse
effects. Furthermore, its simplicity suggests that
respiratoy muscles training could probably also be
performed at home, given a few supervised session
to ensure correct procedure on the part of the patient.
Both primary care providers and pulmonology
center have crucial role to play in realizing the full
potential of rehabilitation strategies. Since the stable
COPD patients come to these units after hospitalized
due to exacerbation. These units can refer COPD
patients to physical medicine and rehabilitation unit
for following respiratory muscles training as the
additional strategy to treat COPD patients.
There were some limitations in our study. First,
the short time for collecting the subjects. Second, the
sample size of this study was very small that we
cannot correlate the CE and PEFR value to other
lung function values which were observed by
spirometer. Even so, these results also had clinical
significance for the therapy of COPD. To sum up,
we confirm that short training of respiatory muscles
improves lung functional as assessed by CE and
PEFR.
ACKNOWLEDGEMENT
We would like to thank to Dr Dewi Wijaya and Dr
Surya Hajar as the pulmonologist in Aulia
Pulmonology Center for their contribution in giving
reference and recommending their patients to
physical medicine and rehabilitation unit.
REFERENCES
Dhamane, A., Moretz, C., Zhou, Y., et al., 2015. COPD
exacerbation frequency and its association with health
care resource utilization and costs. International
Journal of Chronic Obstructive Pulmonary Disease,
10: 2609–18
Shah, T., Press, V, G., Huisingh-Scheetz, M., White, S, R.,
2016. COPD readmissions. Chest, 150 (4): 916–26
Barreiro, E., & Gea, J., 2015. Respiratory and limb
muscle dysfunction in COPD. Journal of Chronic
Obstructive Pulmonary Disease, 12(4): 413-26
Lee, L, W., et al., 2017. Body composition changes in
male patients with chronic obstructive pulmonary
disease: Aging or disease process?. PLoS One, 12(7):
1-14
Man, W., Kemp, P., Moxham, J., & Polkey, M., 2009.
Skeletal muscle dysfunction in COPD: Clinical and
laboratory observation. Clinical science, 117: 251-64
Barreiro, E., & Jaitovich, A., 2018. Muscle atropy in
chronic obstructive pulmonary disease: Molecular
basis and potential therapeutic target. Journal of
Thorasic Disease, 10(12): 1415-24
Rocha, F, R., et al., 2017. Diaphragmatic mobility:
Relationship with lung function, respiratory muscle
strength, dyspnea, and physical activity in daily life in
patients with COPD. Jornal Brasileiro de
Pneumologia, 43(1): 32-7
Vaes, A, W., Delbressine, J, M, L., Mesquita, R., et al.,
2018. The impact of pulmonary rehabilitation on
activities of daily living in patients with COPD.
Journal of Applied Physiology
Houchen-Wolloff, L., Williams, J, E., Green, R, H., et al.,
2017. Survival following pulmonary rehabilitation in
patients with COPD: the effect of program completion
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
160

and change in incremental shuttle walking test
distance. Int J Chron Obstruct Pulmon Dis, 13, 37-44
Mota, S., Güeli, R., Barreiro, E., et al., 2007. Clinical
outcomes of expiratory muscle training in severe
COPD patients. Respiratory medicine, 101: 516-24
Langer, D., Hendriks, E., Burtin, C., et al. 2009. A clinical
practice guideline for physiotherapists treating patients
with chronic obstructive pulmonary disease based on a
systematic review of available evidence. Clin Rehabil,
23(5): 445–462
Sahin H, Varol Y, Naz I, et al. 2016. The effect of
pulmonary rehabilitation on COPD exacerbation
frequency per year. Clin Respir J , 12(1): 165–174.
Osadnik, C, R., McDonald, C, F., Jones, A, P., Holland, A,
E., 2012. Airway clearance techniques for chronic
obstructive pulmonary disease. Cochrane Database of
Systemic Review
McKim, D., 2011. Airway clearance and lung volume
recruitment for individuals with neuromuscular
disease. Ventolator assisted living, 25(4): 3-5
Malaguti, C., Rondelli, R, R., de Souza, L, M., M.
Domingues, M., Dal Corso, S., 2009. Reliability of
chest wall mobility and its correlation with pulmonary
function in patients with chronic obstructive
pulmonary disease. Respiratory Care, 54(12): 1703–
11
Ozgocmen, S., Cimen, O, B., and Ardicoglu, O., 2014.
Relationship between chest expansion and respiratory
muscle strength in patients with primary fibromyalgia.
Clinical Rheumatology, 21(1): 19–22
Reddy, R, S., et al., 2019. Reliability of chest wall
mobility and its correlation with lung functions in
healthy nonsmokers, healthy smokers, and patients
with COPD. Canadian Respiratory Journal, 2019: 1-11
Mulyo, A.N.D, Biben, V., Prabowo, T., 2015. Thorax
expansion and its correlation to spirometry. Indonesian
Journal of Physical Medicine & Rehabilitation, 4: 1-8
Weiner, P., Magadle, R., Beckerman, M., Winer, M.,
Berar-Yanay, N., 2003. Spesific expiratory training in
COPD. Chest, 124: 468-73
Debouche, S., Pitance, L., Robert, A., et al., 2016.
Reliability and reproducibility of chest wall expansion
measurement in young healthy adults. Journal of
Manipulative and Physiological Therapeutics, 20: 1-7
Lanza, F, C., de Caniago, A.A., Archija, L, R., Selman, J,
P., Malaguti, C., Dal, C,S., 2013. Chest wall mobility
is related to respiratory muscle strength and lung
volumes in healthy subjects. Respir Care, 58(12):
2107-12
Martinez, F, J., et al., 2017. Anew approach for identifying
patients with undiagnosed chronic obstructive
pulmonary disease. Am. J. Respir. , 195: 748-56
Homnick, D, N., 2007. Mechanical insufflation-
exsufflation for airway mucus clearance. Respiratory
Care, 52(10): 1296-1305
Su, K, C., 2019. An accurate prediction model to identify
undiagnosed at-risk patients with COPD: a cross
sectional case finding study. Npj Primary Care
Respiratory Medicine, 22: 1-7
Sivasothy, P., Brown, L., Smith, I, E., Sbneerson, J, M.,
2001. Effect of manually assisted cough and
mechanical insufflation on cough flow of normal
subjects, patients with chronic obstructive pulmonary
disease (COPD), and patients with respiratory muscle
weakness. Thorax, 56(6): 438-44
Wang, J., et al., 2019. Observation of the curative effect of
device-guided rehabilitation on respiratory function in
stable patients with chronic obstructive pulmonary
disease. Medicine, 98(8): 1-5
The Description of Lung Function in Stable Chronic Obstructive Pulmonary Disease (COPD) Patients after Following Respiratory Muscles
Training based on Assessment of Peak Expiratory Flow Rate and Chest
161
