
Dysphagia Due to Non-Hodgkin’s Lymphoma after Radiation:
A Case Report of Rehabilitation Management
Annisa Budi Prayuni, Ira Mistivani
Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo National General Hospital,
Faculty of Medicine, University of Indonesia, Jakarta, Indonesia
Keywords: Dysphagia, Head and Neck Cancer, Lymphoma, Rehabilitation Management
Abstract: A 63 years old female was consulted to Dysphagia Clinic in Medical Rehabilitation Department six months
after 20 times radiation with total dose 40Gy due to Non-Hodgkin’s Lymphoma (NHL). She complained
about difficulty in swallowing, dry saliva, and inadequate coughing. First Flexible Endoscopic Evaluation of
Swallowing (FEES) indicated that she had oropharyngeal neurogenic dysphagia with risk of post
swallowing aspiration and Functional Oral Intake Scale (FOIS) was 1 with tube dependent without oral
intake. She got 12 times Neuromuscular Electrical Stimulation (NMES) in suprahyoid and infrahyoid
muscle for 60 minutes and biofeedback 2times/week, breathing and oromotor exercises, Mendelsohn
maneuver, Masako and Shaker Exercise. After 2 months of intensive rehabilitation, the second FEES
showed a progression that patient might swallow semi-solid food with repeated swallowing, FOIS was 2
with tube dependent with minimal oral intake and after 5 months continued with oromotor and swallowing
exercises FOIS was 3 with tube supplements with consistent oral intake. QoL was assessed with M.D.
Anderson Dysphagia Questionnaire, result was improving from 53,68 to 70. Comprehensive rehabilitation
management for dysphagia due to HNC after radiation can improve swallowing function, safety oral intake,
and enhance QoL
1 INTRODUCTION
Dysphagia is a common symptom of head and neck
cancer (HNC), including Non-Hodgkin’s
Lymphoma (NHL), as well as representing a
complication of its treatment, chemoradiation. The
use of radiotherapy with or without chemotherapy
for treatment of HNC as a primary treatment
modality has increased significantly over the past
twenty years. Despite preservation of the structures
of the head and neck, swallow function is not
maintained at normal levels after treatment
(Hutscheson, 2012). Aspiration rates among HNC
patients is estimated to be 36%–94% have been
reported in the literature after treatment with primary
chemoradiotherapy while the incidence of silent
aspiration due to a decrease in the cough reflex is
22%–67% (Kweon, 2018).
Fibrosis of the irradiated tissue of the head and
neck results in impaired movement of the oral
tongue, tongue base, pharyngeal constrictors, and
larynx, leading to dysfunction. Due to mucositis,
edema of the soft tissues, copious mucous
production, xerostomia, and tissue swelling, patients
begin to develop acute dysphagia. These
complications begin to show from 4 to 5 weeks after
radiation-based therapy and persist through the first-
year posttreatment and may be present many years
after completion of radiotherapy (Pauloski, 2008;
King, 2016). Later, fibrosis, neuromuscular
dysfunction, muscles atrophy, lymphedema, and
damage to neural structures occur, leading to the late
effects of dysphagia (Hutscheson, 2012; Kweon,
2018).
Radiation-induced dysphagia is responsible for a
change in the type of diet and a prolongation of the
mealtimes, which participate in anorexia,
malnutrition, and decreasing quality of life (QoL)
(Kweon, 2018; Pauloski, 2008).
144
Prayuni, A. and Mistivani, I.
Dysphagia Due to Non-Hodgkin’s Lymphoma after Radiation: A Case Report of Rehabilitation Management.
DOI: 10.5220/0009066201440148
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 144-148
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2 CASE DESCRIPTION
A 63 years old female was consulted to Dysphagia
Clinic in Medical Rehabilitation Department after
six months after 20 times radiation with total dose
40Gy due to NHL. Radiation is carried out in the
neck region according to figure 1. She got
Nasogastric Tube for nutrition intake and
tracheostomy due to history of airway obstruction
cause of tumor enlargement. She complained about
difficulty in swallowing, dry saliva, mucositis and
inadequate coughing. She experienced weight loss
despite being consulted for nutritional intake via
NGT.
First Flexible Endoscopic Evaluation of
Swallowing (FEES) indicated that she had
oropharyngeal neurogenic dysphagia with risk of
post swallowing aspiration. The results showed that
she had delayed of laryngeal elevation, swallowing
reflex was decreasing, retroflexion of epiglottic was
delayed and cough reflex was inadequate. Her
Functional Oral Intake Scale (FOIS) was 1 with tube
dependent without oral intake. She got 12 times
Neuromuscular Electrical Stimulation (NMES) in
suprahyoid and infrahyoid muscle for 60 minutes
and surface EMG (sEMG) biofeedback 2 times a
week, breathing and oromotor exercises,
Mendelsohn maneuver, Masako and Shaker Exercise
(Figure 2 and 3). The exercises were given for home
exercise and evaluated with biofeedback at hospital.
After 2 months of intensive rehabilitation, the
second FEES showed a progression that patient
might swallow semi-solid food with repeated
swallowing, FOIS was 2 with tube dependent with
minimal oral intake. Oromotor exercises that include
ROM exercises, Mendelsohn maneuver, Masako and
Shaker exercises was continues until the 5
th
month.
Follow-up was done every month. After almost
seven months of rehabilitation, FEES showed an
improving that patient could swallow solid-food and
liquid with repeated swallowing without penetration
and aspiration, also cough reflex was adequate.
FOIS was 3 with tube supplements with consistent
oral intake. Figure 4 shows the progression of the
FOIS results. QoL was assessed with M.D.
Anderson Dysphagia Questionnaire, result was
improving from 53,68 to 70. Now, the patient still in
rehabilitation program to improve her swallowing
with target total oral intake.
Figure 2: Application of Neuromuscular Electrical
Stimulation and Biofeedback therapy of the patient
Figure 1: Patient’s radiation area
Dysphagia Due to Non-Hodgkin’s Lymphoma after Radiation: A Case Report of Rehabilitation Management
145
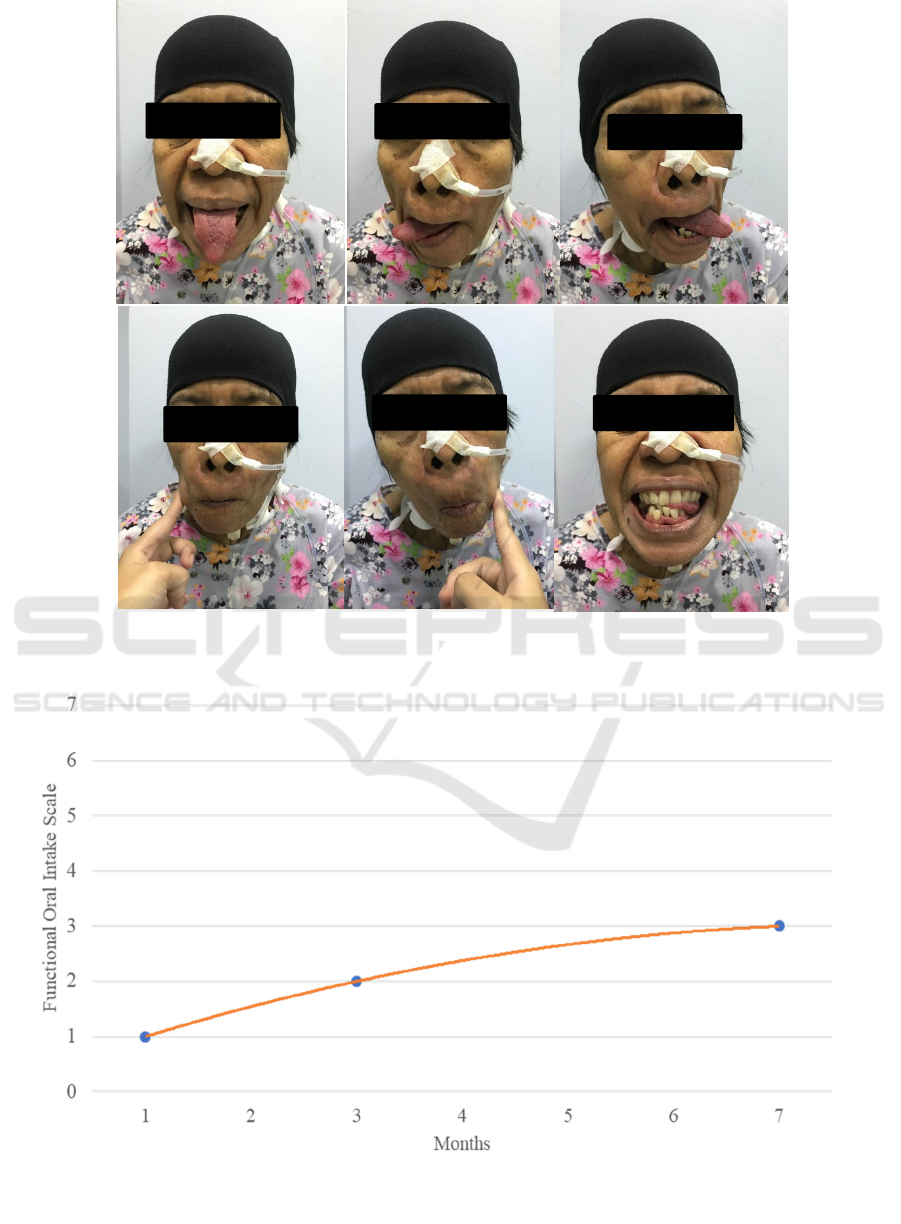
Figure 3: Oromotor Exercises and Masako Exercises of the patient
Figure 4: Progression of Functional Oral Intake Scale of the Patient
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
146

3 DISCUSSION
Patients with cancer of the head and neck may be
treated with surgery, radiotherapy, chemotherapy, or
a combination. Each treatment modality may have a
negative impact on post-treatment swallowing
function, especially in this case report dysphagia
occurred after treated by radiation. Rehabilitative
management available to reduce or eliminate
swallowing disorder in patients treated for cancer of
the head and neck, which include postures,
maneuvers, exercises, and modalities such as NMES
and sEMG biofeedback to help patient achieve
optimal function, improve swallowing function,
safety oral intake, and enhance QoL (Pauloski,
2008).
In this patient, radiation dose was 40 Gy which
may affect fibrotic in irradiated structures results in
limited mobility of the oral tongue, tongue base,
pharynx and larynx. Besides that, radiation also
damage the salivary glands results in significantly
reduced salivary flow. Patient also felt dry in saliva.
Studies of saliva flow after radiation showed that
reduce the dose with below 24 to 26 Gy made saliva
flow is persevered and will increase toward
pretreatment levels over the first year. Glands
receiving a mean dose higher than the threshold will
produce little saliva with no recovery over time.
Reduced saliva weight does not correlate with
slowed or inefficient swallow. Instead, reduced
saliva weight seems to change the patient’s
perception of swallowing ability and, on that basis,
affects diet choices (Logemann, 2001).
Oromotor exercises that include range of motor
(ROM) exercise, postures, and maneuvers were
given to the patient. The normal range of motion of
the lips, jaw, tongue, and larynx is often disrupted
after treatment for cancer of the head and neck, as a
result of fibrosis induced by radiation. ROM
exercises are designed to improve the movement by
extending the target structure in a desired direction
until a strong stretch is felt. Range of motion
exercises can be used for the lips, jaw, oral tongue,
tongue base, larynx, and hyoid-related musculature
to improve movement. Tongue range of motion
exercises for the oral tongue include extension,
lateralization, elevation, and retraction (Pauloski,
2008).
Mendelsohn maneuver is one of maneuver that
we give to the patient. This maneuver is a voluntary
prolongation of laryngeal excursion at the midpoint
of the swallow, intended to increase the extent and
duration of laryngeal elevation and thereby increase
the duration of cricopharyngeal opening. Since the
first FEES showed that patient had delayed of
laryngeal elevation, we choosed Mendelsohn
maneuver which research has indicated that it is
effective at increasing the extent and duration of
laryngeal elevation as well as duration of
cricopharyngeal opening. Mendelsohn maneuver
may be practiced with or without a bolus as dictated
for safety and as an exercise (Pauloski,2008).
The Masako exercise or tongue-hold exercise is
an oro-pharyngeal exercise rehabilitation technique
to enhance the function of the constrictor pharyngeal
superior. This technique is mainly performed to
strengthen its function of pushing food boluses from
the oral cavity to the pharynx by strengthening the
contact between the tongue base and the laryngo-
pharyngeal wall. Patient holds the tongue forward
between the teeth while swallowing. Its intent is to
improve movement and strength of the posterior
pharyngeal wall during the swallow (Logemann,
2008; Byeon, 2016).
Another exercise that we were given to the
patient is Shaker Exercise. Suprahyoid muscle group
responsible for displacement of the hyolaryngeal
complex and opening of the Upper Esophageal
Spinchter (UES) appears responsive to external
influences, like a simple isometric/isokinetic head
lift exercise. For this exercise, patient was instructed
to raise the head high and forward enough to be able
to see their toes without raising shoulders off the
ground. The rationale for the exercise is to build
strength in the suprahyoid musculature, thus
enhancing hyoid and laryngeal (Pauloski 2008).
sEMG Biofeedback was used to the patient twice
a week for evaluate the exercise. Biofeedback was
used during swallow attempts and oromotor exercise
to assist the patient in maintaining the requested
duration of each swallow attempt and to providing
progressively more challenging targets based on
strength. Electrodes were placed on the on the
submental muscles (mylohyoid, geniohyoid, anterior
belly of digastric, genioglossus) and a third
reference electrode was placed to one side of
zygomaticus. The sEMG signal represents the timing
and force of the muscle contraction and is displayed
graphically on a screen. An ascending threshold
approach was employed in which the patient was
required to progressively increase swallow effort
and strength to obtain a visual feedback (Benfield,
2008; Crary, 2004).
Surface neuromuscular electrical stimulation
(NMES) has recently been proposed as a treatment
option for pharyngeal dysphagia. Surface electrical
stimulation is applied through electrodes placed on
the neck with the goal of promoting increased hyoid
Dysphagia Due to Non-Hodgkin’s Lymphoma after Radiation: A Case Report of Rehabilitation Management
147

or laryngeal elevation. NMES for dysphagia has
become a widely utilized clinical procedure yet is
accompanied by considerable controversy because
of a lack of physiologic rationale and limited
published efficacy data (Pauloski,2008).
Study from Ryu et al evaluated the effect of
NMES in patient suffering from dysphagia
following treatment for head and neck cancer with
procedure 30 minutes of NMES, 5 days a week for 2
weeks combined with traditional swallowing
therapy. This study showed that NMES combined
with traditional swallowing training is superior to
traditional swallowing training alone in patients
suffering from dysphagia following treatment for
head and neck cancer (Ryu, 2009). Meanwhile,
another study from Langmore et al that did a
randomize controlled trial of 170 patients with active
NMES and swallow exercises versus sham NMES
and swallow exercises group showed that after 12
weeks program, NMES did not add benefit to
traditional swallow exercises (Langmore, 2016).
Although the results of existing studies showed
inconsistent results, NMES combined with oromotor
and swallowing exercises seems provide benefits to
the patients with progressing Functional Oral Intake
Scale (FOIS) and increasing the QoL from M.D.
Anderson Dysphagia Questionnaire result. Now, the
patient still in rehabilitation program to improve her
swallowing function with target safety total oral
intake with adequate nutrition. Patient may still need
modification of diet and swallowing maneuver.
In conclusion, comprehensive rehabilitation
management for dysphagia due to HNC after
radiation can improve swallowing function, safety
oral intake, and enhance QoL.
REFERENCES
Hutscheson KA, Lewin JS, Barringer DA, Lisec A, Gunn
B, Moore MWS, et al. 2012. Late Dysphagia after
Radiotherapy-Based Treatment of Head and Neck
Cancer. Cancer, 118(23), pp.5793-9.
Kweon S, Koo BS, Jee S. 2018. Change of Swallowing in
Patients with Head and Neck Cancer After Concurrent
Chemoradiotherapy. Ann Rehabil Med, 40(6),
pp.1100-7.
Pauloski BR. 2008. Rehabilitation of Dysphagia
Following Head and Neck Cancer. Phys Med Rehabil
Clin N Am, 19(4), pp.889–928.
King SN, Dunlap NE, Tennant PA, Pitts T. 2016.
Pathophysiology of Radiation-Induced Dysphagia in
Head and Neck Cancer. Dysphagia, 31(3), pp.339–51.
Logemann JA, Smith CH, Pauloski BR, et al. 2001.
Effects of xerostomia on perception and performance
of swallow function. Head Neck, 23(4), pp.317–21.
Logemann JA. 2008. Treatment of Oral and Pharyngeal
Dysphagia. Phys Med Rehabil Clin N Am, 19,
pp.803–16.
Byeon H. 2016. Effect of the Masako maneuver and
neuromuscular electrical stimulation on the
improvement of swallowing function in patients with
dysphagia caused by stroke. J. Phys. Ther. Sci, 28,
pp.2069–71.
Benfield JK, Everton LF, Bath PM, England TJ. 2008.
Does Therapy With Biofeedback Improve Swallowing
in Adults With Dysphagia? A Systematic Review and
Meta-Analysis. Archives of Physical Medicine and
Rehabilitation, 100(3), pp.551-61.
Crary MA, Carnaby GD, Groher ME, Helseth E. 2004.
Functional Benefits of Dysphagia Therapy Using
Adjunctive sEMG Biofeedback. Dysphagia, 19,
pp.160–4.
Ryu JS, Kang JY, Park JY, Nam SY, Choi SH, Roh JL, et
al. 2009. The effect of electrical stimulation therapy
on dysphagia following treatment for head and neck
cancer. Oral Oncology, 45, pp.665-8.
Langmore SE, McCulloch TM, Krisciunas GP, Lazzarus
CL, Daele DJV, Pauloski BR, et al. 2016. Efficacy of
Electrical Stimulation and Exercise for Dysphagia in
Head and Neck Cancer Patients: A Randomized
Clinical Trial. Head Neck, 38 (1), pp.1221-31.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
148
