
Observational Study of Recurrent Heart Attacks and Barriers to
Participation in Exercise Training Cardiac Rehabilitation:
A Serial Case Report
Lia Miranda
1
, Deddy Tedjasukmana
2
1
Physical Medicine and Rehabilitation Residency Program, Faculty of Medicine, Universitas Indonesia, Indonesia
Dr. Cipto Mangunkusumo National Hospital
2
Cardiorespiratory Division, Physical Medicine and Rehabilitation Department, Universitas Indonesia, Indonesia
Dr. Cipto Mangunkusumo National Hospital
li4mir4nd4@gmail.com, deddytedjasukmana60@gmail.com
Keywords: Recurrent Heart Attack, Exercise Training, Barriers in Cardiac Rehabilitation
Abstract: Acute coronary syndrome (ACS) is the most common cause of mortality in Coronary Artery Disease
(CAD) patients, 20% of ACS survivors will experience a recurrent heart attack. Exercise training as a part
of cardiac rehabilitation increases the quality of life, functional capacity, prevents recurrent heart attack
and reduces mortality but the participation rate is still very low. Among 36 patients who were admitted in
July 2019 in ICCU Ward, RSCM, 14 patients had recurrent heart attacks where 11 patients did not follow
phase II cardiac rehabilitation while 2 patients took part in cardiac rehabilitation. Recurrent heart attacks
are influenced by modifiable and unmodifiable factors and exercise training as a core of cardiac
rehabilitation is important to prevent this cardiac event because it has cardioprotective mechanisms.
Patients who got recurrent heart attacks had barriers to participate in exercise training included lack of
education, difficulty to arrange schedule, transportation or distance, no rehabilitation center and lack of
awareness. Exercise training in cardiac rehabilitation has beneficial effects in preventing recurrent heart
attacks and barriers to participate in it are challenges that we must overcome.
1 INTRODUCTION
In 2016, the American Heart Association (AHA)
reported 15.5 million Americans with age more
than 20 years had coronary heart disease, where per
42 seconds a person has suffered from myocardial
infarction (Heart Disease Fact, 2017). In Indonesia,
coronary heart disease is the second leading cause
of death after stroke, which is as much as 3.6% of
the age group most often occurs in the age group of
65-74 years followed by the age group of 75 years
and over (3.2%), age group 55-64 years (2.1%) and
age group 35-44 years (1.3%) (Penyakit Jantung
Penyebab Kematian Tertinggi, 2017). According to
the European Association for Cardiovascular
Prevention and Rehabilitation, coronary heart
disease remains a leading cause of mortality and
morbidity, although mortality of coronary heart
disease has declined considerably in the past 20
years.
1
However, the 1-year mortality rate is around
20% in patients with myocardial infarction (MI).
Among the patients who survive, 20% will
experience a recurrent MI within 1 year. It is
estimated that recurrent events caused by progression
of coronary and systemic atherosclerosis. Secondary
prevention including cardiac rehabilitation (CR) is
therefore essential to improve the long-term
prognosis of patients with MI and to improve their
quality of life and functional capacity (Hald, 2018).
The cardiac rehabilitation program for coronary
heart disease is a class 1 recommendation according
to the American Heart Association, the American
College of Cardiology and the European Society of
Cardiology (Kachur, 2017). In 1994, the AHA
declared that cardiac rehabilitation should not be
limited to an exercise training program but also
should include multifaceted strategies aimed at
reducing or controlling modifiable risk factors so it
can reduce morbidity and mortality. Cardiac
rehabilitation as secondary prevention programs
currently include baseline patient assessments,
nutritional counseling, aggressive risk factor
management (such as lipids, hypertension, weight,
diabetes, and smoking), psychosocial and
vocational counseling, and physical activity
counseling and exercise training, in addition to the
Miranda, L. and Tedjasukmana, D.
Observational Study of Recurrent Heart Attacks and Barriers to Participation in Exercise Training Cardiac Rehabilitation: A Serial Case Report.
DOI: 10.5220/0009066001350138
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 135-138
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
135
appropriate use of cardioprotective drugs that have
evidence-based efficacy for secondary prevention
(Leon, 2005).
However, an exercise in cardiac rehabilitation is
commonly underused throughout this process only
30% to 50% of eligible patients are typically
referred to outpatient cardiac rehabilitation, with
fewer still completing programs (Giuliano, 2017).
The low participation in cardiac rehabilitation is
influenced by many things including transportation
problems or long distance to the heart rehabilitation
center, time problems such as difficulty in arranging
schedules due to work, economic factors, other
health factors and lack of awareness about the
importance of cardiac rehabilitation (Haddadzadeh,
2011)
From this study, we predicted that patients who
participated in the exercise program of cardiac
rehabilitation had a lower risk for recurrent cardiac
events.
2 METHODS
This is an observational study of patients who were
admitted to the Intensive Cardiology Care Unit
(ICCU) at Cipto Mangunkusumo National General
Hospital for recurrent heart attacks. Data were
obtained from patients' register in July 2019,
medical record and information by phone.
Information about patients' characteristics, risk
factors, heart attack frequency, and cardiac
rehabilitation program were gotten from patients'
registration, medical records and confirmation by
phone.
3 RESULT
Among 36 patients who were admitted in July 2019
in ICCU ward, RSCM because heart attacks, 14
patients had recurrent heart attacks consisted of 10
men and 4 women with age range 42-74 years old.
One patient had 8 times recurrent heart attacks, 2
patients had 4 times recurrent heart attacks, 1 patient
had 3 times recurrent heart attacks and 10 patients
had 2 times recurrent heart attacks (Table 1). Among
them, 9 patients had uncontrolled hypertension, 5
patients had uncontrolled diabetes mellitus, 8
patients had overweight or obesity, 9 patients have a
history of the smoking habit, 11 patients had a
sedentary lifestyle and 8 patients had genetic history.
Twelve (85.7%) of 14 patients who got recurrent
heart attacks did not a joint exercise in cardiac
rehabilitation because of many reasons. Five Patients
(41.7%) said that there were no information or
education about exercise in cardiac rehabilitation, 2
(16.7%) patients because difficulty to arrange
schedule, 2 (16.7%) patients because lack of
awareness, 1 (8.3%) patient had other medical
problems, 1 patient did not participate exercise in
cardiac rehabilitation because there was no
rehabilitation center and 1 patient because
transportation problem.
Among 14 patients who got recurrent heart
attacks, 2 patients followed cardiac rehabilitation but
1 patient was not compliance in phase II cardiac
rehabilitation because a musculoskeletal problem
that is limb pain because the history of neglected
fracture of the right femur and 1 patient did not
continue to phase III cardiac rehabilitation because
of lack of motivation.
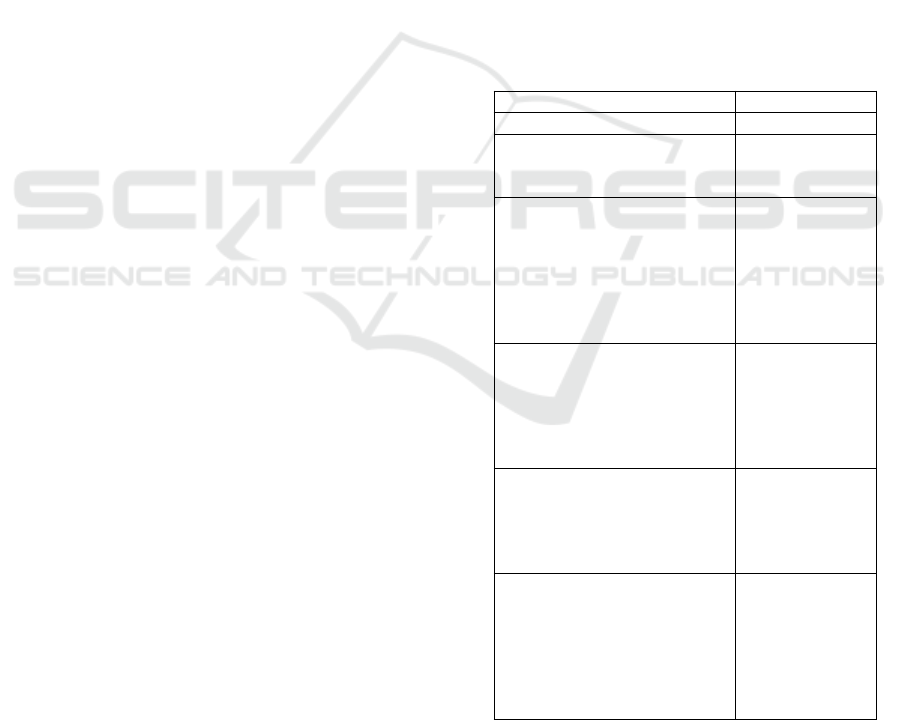
Table 1: Patients’ Characteristic.
Characteristic
Number (%)
Age
42 – 74 y. o
Gender
Female
Male
4 (28.6 %)
10 (71.4 %)
Risk Factor
Hypertension
Diabetes
Obesity
Dyslipidemia
Smoking
Sedentary Lifestyle
9 (64.3 %)
5 (35.7 %)
8 (57.1 %)
9 (64.3 %)
9 (64.3 %)
11 (78.6 %)
Number of recurrent heart
attack
2 times
3 times
4 times
>4 times
10
1
2
1
Phase II and III Cardiac
Rehabilitation Exercise
Participation
Yes
No
2 (14.3%)
12 (85.7%)
Reasons not following CR
Lack of education
Lack of awareness
Schedule problem
Distance/transport problem
No Rehabilitation center
Other medical problems
5 (41.7 %)
2 (16.7%)
2 (16.7%)
1 (8.3%)
1 (8.3%)
1 (8.3%)
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
136

4 DISCUSSION
Recurrent heart attacks are influenced by
unmodifiable risk factors such as genetics, age,
gender and modifiable risk factors such as
hypertension, diabetes mellitus, obesity, smoking,
dyslipidemia, and physical inactivity or sedentary
lifestyle (Humal, 2012) All of the patients who got
recurrent heart attacks was more than 40 years old
with higher prevalence in man than woman with
ratio 5:2 and 8 (57.1%) patients had genetic risk
factor. All of these increased unmodifiable risk
factors of patients to get recurrent heart attacks
(Foussas, 2016). More than 50% of patients had
uncontrolled modifiable risk factors such as
hypertension, diabetes mellitus, dyslipidemia,
smoking, overweight or obesity, and a sedentary
lifestyle. All of these also increased the risk of
getting recurrent heart attacks.
Exercise training as a core of cardiac
rehabilitation is really important to prevent these
recurrent cardiac events (Leon, 2005). Exercise in
cardiac rehabilitation has 3 phases that are a phase I
for inpatient, phase II for outpatient as long as 8-12
weeks and phase III as a maintenance phase for
lifetime exercise (Basuni, 2016). Exercise training,
as part of a comprehensive rehabilitation program,
has cardioprotective mechanisms that can slow the
progression or partially reduce the severity of
coronary atherosclerosis. Multiple factors directly or
indirectly appear to contribute to this anti-
atherosclerotic effect. Increased flow-mediated shear
stress on artery walls during exercise results in
improved endothelial function which is associated
with enhanced synthesis, release, and duration of
action of nitric oxide. Nitric oxide is responsible for
endothelium-dependent vasodilatation and inhibits
multiple processes involved in atherogenesis and
thrombosis. Chronic inflammation plays a major role
in the pathogenesis of CAD and plaque stability. The
plasma level of C-reactive protein, a nonspecific
biomarker of inflammation, is associated with an
increased risk of CAD. Aerobic exercise training
and improved cardiorespiratory endurance are
associated with reduced C-reactive protein levels,
which suggests that exercise training has anti-
inflammatory effects. Besides, exercise training and
regular physical activity can result in moderate
losses in body weight and adiposity (Leon, 2005).
Endurance exercise also can promote decreases
in blood pressure and serum triglycerides, increases
in high-density lipoprotein cholesterol and
improvements in insulin sensitivity and glucose
homeostasis which along with modest weight
reduction have been shown to reduce the risk of type
2 diabetes mellitus in individuals with glucose
intolerance. Endurance exercise training also has
potential anti-ischemic effects. it can reduce
myocardial ischemia decreasing myocardial oxygen
demands during physical activity and exercise
thereby raising the ischemic threshold. Also,
exercise training can increase coronary flow by
improving coronary artery compliance or elasticity
and endothelium-dependent vasodilatation and by
increasing the luminal area of conduit vessels
through remodeling or arteriogenesis and myocardial
capillary density by angiogenesis (Leon, 2005).
Many meta-analyses studies showed the
effectiveness of exercise in cardiac rehabilitation in
coronary heart disease. Existing data indicated that
comprehensive cardiac rehabilitation after
myocardial infarction will reduce mortality by 15%
to 28% and the mortality rate of patients undergoing
an exercise in cardiac rehabilitation decreases 26%
to 31% when compared to patients who do not
participate in cardiac rehabilitation. Guidelines
issued by the American Heart Association and the
American College of Cardiology recommend cardiac
rehabilitation in patients after a heart attack
(Stephens, 2009).
Exercise in cardiac rehabilitation is safe to do.
The incidence of side effects in supervised exercises
is very small, namely 1/50,000 to 1 /120,000 (Leon,
2005). Cardiac rehabilitation is a class I
recommendation for all patients with CAD based on
a growing body of evidence that participation can
reduce hospital bed usage, cardiovascular mortality,
as well as improve functional capacity and quality of
life but participation rate of exercise is still very low
at around 30% - 50%, and influenced by various
factors (Giuliano, 2017). This agrees with this study
where among 14 patients who got recurrent heart
attacks, 12 (85.7%) patients did not participate in
phase II cardiac rehabilitation and 2 (14,3%) patients
participated in phase II cardiac rehabilitation but 1
patient was not compliance in phase II cardiac
rehabilitation because musculoskeletal problem and
1 patient did not continue to phase III cardiac
rehabilitation because lack of motivation.
The low participation in cardiac rehabilitation is
influenced by many things including transportation
problems or long distance to the heart rehabilitation
training center, time such as difficulty arranging
schedules due to work, economic factors, other
health problems and lack of awareness that the
importance of cardiac rehabilitation (Haddadzadeh,
2011). In this study, lack of information or education
(41.7%) as being the most reason patients did not
Observational Study of Recurrent Heart Attacks and Barriers to Participation in Exercise Training Cardiac Rehabilitation: A Serial Case
Report
137

participate in cardiac rehabilitation, followed by
difficulty to arrange schedule (16.7%), lack of
awareness (16.7%), no rehabilitation center (8.3%)
and transportation or distance problem (8.3%) and
other medical problem (8.3%).
5 CONCLUSION
Exercise training in cardiac rehabilitation has
beneficial effects in preventing recurrent heart
attacks and barriers to participate in it are challenges
that must be overcome.
REFERENCES
Central For Disease and Control Prevention. 2017. Heart
Disease Facts.
https://www.cdc.gov/heartdisease/facts.htm. Cited 26
September 2019 (15:23)
Kesehatan Kesehatan Republik Indonesia. 2017. Penyakit
Jantung Penyebab Kematian Tertinggi, Kemenkes
Ingatkan CERDIK. http://www.depkes.go.id. Cited 26
September 2019. (16.00)
Hald, K., Nielsen, MK., Nielsen, CV., Meillier, LK. 2018.
Expanded cardiac rehabilitation in socially vulnerable
patients with myocardial infarction: a 10-year follow-
up study focusing on mortality and nonfatal events.
BMJ Open. 8:019307.
Kachur, S., Chongthammakun, V., Lavie, CJ., Arena, R.,
Milani, R V., et al. 2017. Progress Cardiovascular
Disease. http://dx.doi.org/10.1016/j.pcad.2017.07.002.
Cited 26 September 2019 (16.30)
Leon, AS., Franklin, BA., Costa, F., Balady GJ. 2005.
Cardiac Rehabilitation and Pencegahan sekunder of
Coronary Heart Disease. Circulation. 111,pp.369-376.
Giuliano, C., Parmenter, BJ., Baker, MK., Mitchell BL.
2017. Cardiac Rehabilitation for Patients With
Coronary Artery Disease: A Practical Guide to
Enhance Patient Outcomes Through Continuity of
Care. Clinical Medicine Insights: Cardiology 11,pp.1–
7.
Haddadzadeh, MH., Maiya1, AG., Padmakumar, R., Shad
B. 2011. Effect of Exercise-Based Cardiac
Rehabilitation on Ejection Fraction in Coronary Artery
Disease Patients: A Randomized Controlled Trial.
Heart Views. 12,pp.51-7.
Humal, S., Tariq, R., Amin1, F., Mahmood, KJ. 2012.
Modifiable and Non-modifiable predisposing Risk
Factors of Myocardial Infarction -A Review. Sadia
Huma et al /J. Pharm. Sci. & Res. 4(1),pp.1649-1653.
Foussas, S. 2016. Obesity and Acute Coronary Syndromes.
Hellenic J Cardiol 57(1), pp.63-65.
Basuni, DT., Putra, HL. 2016. Rehabilitasi
Kardiovaskular. 1
st
ed. PB PERDOSRI
Stephens, MB. 2009. Cardiac Rehabilitation. American
Family Physician. 80(9):955-959, 960.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
138
