
Late Referred Proximal Focal Deficiency:
A Comprehensive Rehabilitation Management - A Case Report
Juwita Arum M
1
, Damayanti Tinduh
1
, I Putu Alit Pawana
1
, SM Mei Wulan
1
, Keiichi Tsukishiro
2
1
Department of Physical Medicine and Rehabilitation, Dr. Soetomo Academic Medical Center Hospital, Universitas
Airlangga, Surabaya, Indonesia
2
Department of Assistive Rehabilitation, Faculty of Rehabilitation of Hiroshima International University,
Hiroshima, Japan
Keywords: PFFD, Proximal Focal Femoral Deficiency, Congenital limb deficiency, Phocomelia
Abstract: A child with Proximal Focal Femoral Deficiency (PFFD) would suffer a gait problem due to leg
deformities. PFFD is a rare congenital anomaly ranging from one case per 50,000 population to one case
per 200,000 population. This is a case report of a 5 years old girl with isolated left PFFD Aitken D. She
met the orthopedic at the age of 6 months and asked to come back at 5 years. She has left knee contracture
and limited involved hip range of motion also hypermobility joint in the uninvolved leg. The patient
walking by kneeling to compensate for the leg length discrepancy (LLD) and has an inadequate function
of the uninvolved leg. The rehabilitation program consists of a home-based strengthening and stretching
exercise program, gait training, balance exercise, elastic tape application, and an adaptive prosthesis. At
the end of 2 months of comprehensive rehabilitation management, the balance has improved and the
patient was able to stand at the same level as her friends and walking with an adaptive prosthesis with a
better gait pattern.
1 INTRODUCTION
Proximal focal femoral deficiency (PFFD) is a
congenital anomaly that involves the pelvis and
proximal femur with widely variable clinical
manifestations, from mild femoral shortening and
hypoplasia to the absence of any functional femur
and acetabulum aplasia (Dillon et al., 2005). The
more severe presentations would have progressive
subluxation to dislocation of the femur (Alexander
et al, 2015). Aitken in 1969 made a simple
classification for PFFD which is widely used
worldwide. This divides PFFD into four classes
based on the radiographic appearance and the
anatomic relationship between the acetabulum and
the proximal end of the femur (Lasanianos and
Kanakaris, 2015). The child may need a socket at a
relatively young age to capture the limb and
provide maximum stability. Surgery is not the first
option for PFFD treatment, it’s indicated to made
more acceptable stump, provide hip stability and
improving gait pattern when wearing a prosthesis
(Alexander et al, 2015). The fusion of the femoral
remnant to the tibial remnant would effectively
create a residual limb that functions and has
prosthetic needs of a knee disarticulation patient. A
Van Ness rotationplasty is another surgical
procedure frequently used in this case (Ackman et
al., 2013).
2 CASE REPORT
A 5 years old girl came to our hospital in the last
week of July 2019 with PFFD Aitken D. She lived
in a small village in Pasuruan district, about 90 km
from Surabaya. Her father was a carpenter, working
on a local businessman, while her mother was an
honorary clerk at the restaurant near the house. She
started kindergarten this semester. She is the only
child, spontaneous delivery at term by a midwife,
with 3700 grams birth weight and spontaneously
crying. No clear cause at prenatal history. At 6
months old she has met the orthopedic, got X-Rays
and come back at the age of 5 or 6 years old. Her
development was similar to another child, she eats
130
M, J., Tinduh, D., Pawana, I., Wulan, S. and Tsukishiro, K.
Late Referred Proximal Focal Deficiency: A Comprehensive Rehabilitation Management - A Case Report.
DOI: 10.5220/0009065001300134
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 130-134
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
the same food as the family, communicate verbally,
but shy with strangers. She could write a letter. No
complaint on pee nor defecation. Based on her
mother, the patient could walk as far as about 300
m to play to the neighbors. The girl wants to stand
upright and joint the carnival to celebrating the
independent day.
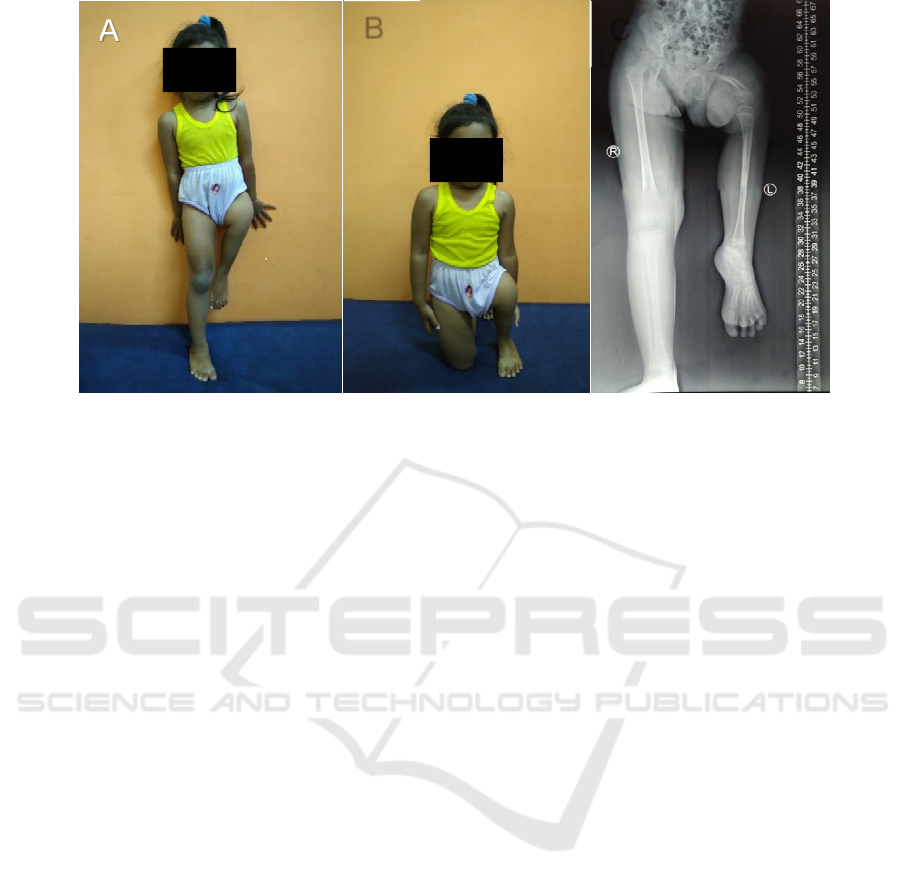
On examination, we found the left thigh was
much shorter than the right one, whereas the size of
the tibia and foot at both sides were the same (Fig
1). The body weight 16 kg with body length 102
cm, and head circumference 102 cm. She had
limitations range of movement (ROM) on her left
hip, the left knee ROM was 60 – 135 with hard
end feel and. The manual muscle test (MMT) of left
hip flexor and extensor were 2. She can’t do one leg
stands (OLS) with open eyes on her good leg. The
girl walked by kneeling her right knee to
compensate for the difference in leg length. When in
the house, she walks with kneeling the right knee,
while on the ground, she walks using both of her
foot so the right knee at her chest level. She used
pelvic rotation to move forward to compensate for
the weakness of the hip flexors. There were no
anomalies were found on the skeletal, cardiac,
gastrointestinal, genitourinary, or nervous systems
were observed. No trauma she got, no pain, no
swollen or redness on her left leg. There were no
family members has the same deformity as hers. For
the time being, the parent not considered surgery as
the acceptable treatment. The radiograph in
standing position, show there were no femoral head
nor acetabulum on the left side. The femoral
remnant hanging in abduction and flexion position.
(Figure 1C).
In the first week of rehabilitation program, our
main goal was to increase her balance. Due to the
socioeconomic condition, she was given a home-
based exercise program. The program would be
evaluated every 2 weeks. The progress sent weekly
by the mother via Whatsapp®. We taught her
mother to stretch the hip abductor, flexor and
internal rotator, bridging exercise, sit to stand and
how to walking with the walker, OLS practice and
strengthening lower extremity. Continuous
counseling also was given both to the patient and the
parent to help them to accept the girl’s condition and
boost the girl’s confidence. The adaptive prosthesis
was made with specification: ischial containment
adaptive socket with an open front and footrest, knee
joint, shank, sach foot (Figure 2A).
Two weeks later, the girl already could do OLS
less than a second and could walk with a walker. We
found the Lachman test, valgus and varus stress test
on the right knee were positive. Anterior drawer test
in both ankles was also positive. The hypermobility
joints were not helped her balance. We gave her
elastic tape on her right knee and ankle to provide
more stability. Soon after elastic tape application,
the girl could do OLS for four seconds. In the fourth
Figure 1: Clinical appearance patient. (A) The front view, the left ankle at the right knee level. The girl can not stand
without holding to something. (B) Patient position when walking indoor, the right knee touching the floor with her lower
leg bending backward and the left ankle in tip toeing. (C) Radiograph image. The left acetabulum not formed and absence
of femoral head. The size of the left femoral shaft is less than 50% of the right femur. Note the linear blurry image, which
caused by patient’s movement due to poor balance.
A
B
C
Late Referred Proximal Focal Deficiency: A Comprehensive Rehabilitation Management - A Case Report
131

week, the girl could do OLS for 2 seconds without
elastic tape, and six seconds with elastic tape. We
give elastic tape once every 2 weeks which lasts for
5 days on the girl.
The girl got adapted prosthesis at the sixth week
of our rehabilitation program, but she rejected her
prosthesis. She cried and would not looked into it.
We explained to the parents and showed the girl
some videos with a girl wearing lower limb
prostheses. We monitored as the girl slowly accept
her prosthesis. She had difficulty to control the knee
unit, so we suggest the parent to lock the knee
momentarily. The girl’s response was good. She felt
more stable with the knee locked in the extended
position. The next week, she could walk with the
prostheses by handheld to the parents. At the eighth
week, she already could walk some steps with her
prosthesis independently, with fast steps and limping
gait. There were no pain nor discomfort during the
use of prosthesis and no
redness nor blisters on the
skin that contact with the socket. After given some
correction on her gait and motor education, she
could walk further (about 5m) independently (Fig 2
B,C). The pelvic rotation is reduced. The balance
was significantly improved, she could do OLS for 7
seconds without elastic tape. However, the girl’s still
couldn’t do hoping and sit to stand without hold. She
still has to hold on when walking long distance. The
strengthening exercise continued at home and the
gait exercise would be done every 2 weeks.
3 DISCUSSION
PFFD is an anomaly that results from the
development failure of the subtrochanteric portion of
the femoral shaft. It’s a rare skeletal disorder ranging
from one case per 50,000 population to one case per
200,000 population (Lasanianos and Kanakaris,
2015). It could be diagnosed early at 20 weeks
gestational age using ultrasound with characteristic
the absent of femoral head and shortening femoral
shaft (D’Ambrosio et al., 2016). Early diagnosed
PFFD would help the parent to accept their child’s
condition. Although the etiology of PFFD is
uncertain, the common etiologies of the short femur
should be excluded, such as aneuploidy (especially,
trisomy 21), poor diabetic control, exposure to drugs
(thalidomide), viral infections, radiation, focal
ischemia between the 4
th
and 8
th
week of gestation
(Lin et al., 2013).
Aitken in 1969 has described a classification that
has been widely used. The radiographic findings are
ranked from a benign form (A) to a severe form (D)
according to the extent of the femoral deficiency.
Type A has a small area of deficient femur below
the femoral head. In type B this same segment is
absent. In type C the femoral head is absent and the
acetabulum deformed. Finally in type D both the
acetabulum and femoral head are absent (Lasanianos
and Kanakaris, 2015).
Figure 2. (A) The adaptive prosthesis with adaptive front open ischial containment socket and foot rest. (B) The girl stand
in her good leg. (C) The girl and her adaptive prosthesis anterior view. (D) Lateral view of the girl
B
C D
A
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
132
Each child with PFFD must be assessed
individually since no single treatment approach
applies to all cases. Limb lengthening is indicated in
cases which predicted discrepancies at maturity not
exceeding 20 cm, in hips that are or can become
stable and when a relative good knee, ankle, and foot
is present. In the case of predicted discrepancies
greater than 20 cm or if other reasons do not render a
child suitable for limb lengthening, prostheses
should be considered Treatment options could be
generalized based on Aitken classification which
vary from shoe lift, prosthesis, and both surgery and
prosthesis. In classes C and D a stable hip joint
cannot be obtained thus a fusion of the hip and,
possibly, the knee joint is necessary (Lasanianos,
Kanakaris and Giannoudis, 2015). The fusion of the
femoral remnant to the tibial remnant, would
effectively create a residual limb that functions and
has prosthetic needs of a knee disarticulation patient.
A Van Ness rotationplasty is another surgical
procedure frequently used in this case (Ackman et
al., 2013). A Van Nesh rotationplasty indicated
when the ankle level of the affected side is at the
same with the knee level of the unaffected side.
When the femoral remnant is less than 50%, it
would made the ankle fell above the knee, Syme
amputation is the recommended procedure to
provide a good stump. However, surgery not the first
option in this case. Since the girl’s parent objection
for the surgery and the girl already could walk by
herself, we decide prosthesis would be the best
treatment choice for the time being.
Weakness and contracture of the left limb of the
girl due to lack of use. She walks in an abnormal
position for her first 4 years. As the prosthesis use
needs several qualifications, exercise is also the
main treatment in this case. Side lying in the left side
would stretch the hip abductor, bridging would
target hip extensor, and sit to stand exercise would
activate the quadriceps muscle and increased knee
stability (Da Costa, Savelsbergh and Rocha, 2010).
The child with lower limb deficiency should be
fitted with a prosthesis when he or she is ready to
pull up to a standing position (Abudu et al., 2006).
This usually occurs between 9 and 10 months of age.
The goals in fitting a prosthesis at this early age are
to allow for normal two-legged standing,
proprioceptive input, provide a better means for
reciprocating gait development, and provide a
normal appearance (Alexander et al, 2015). The
prosthesis should be simple in design, allow growth
adjustment, suspend securely, and preferably
lightweight. It is very important to establish a
standing position for the girl as soon as possible. It
would provide better proprioceptive which is
important for walking endgram (Barra and
Pérennou, 2013). The gait pattern maturity around
the age of 7-8 years old. As the girl is now 5 years
old, it is important to improve the child’s posture
and walking pattern at this time.
The girl has hypermobility syndrome, which
worsening her balance. We put elastic tape on her
right knee and ankle so it would help to stabilize the
leg. Elastic taping could give the proprioceptive
stimuli to establish the joints (Chinn et al., 2014).On
the second visit, elastic tape application was
significantly improved OLS time, from 1 second to 4
seconds after elastic tape application.
The home-based exercise is more often used in
elderly patients with frailty (Clegg et al., 2014). In
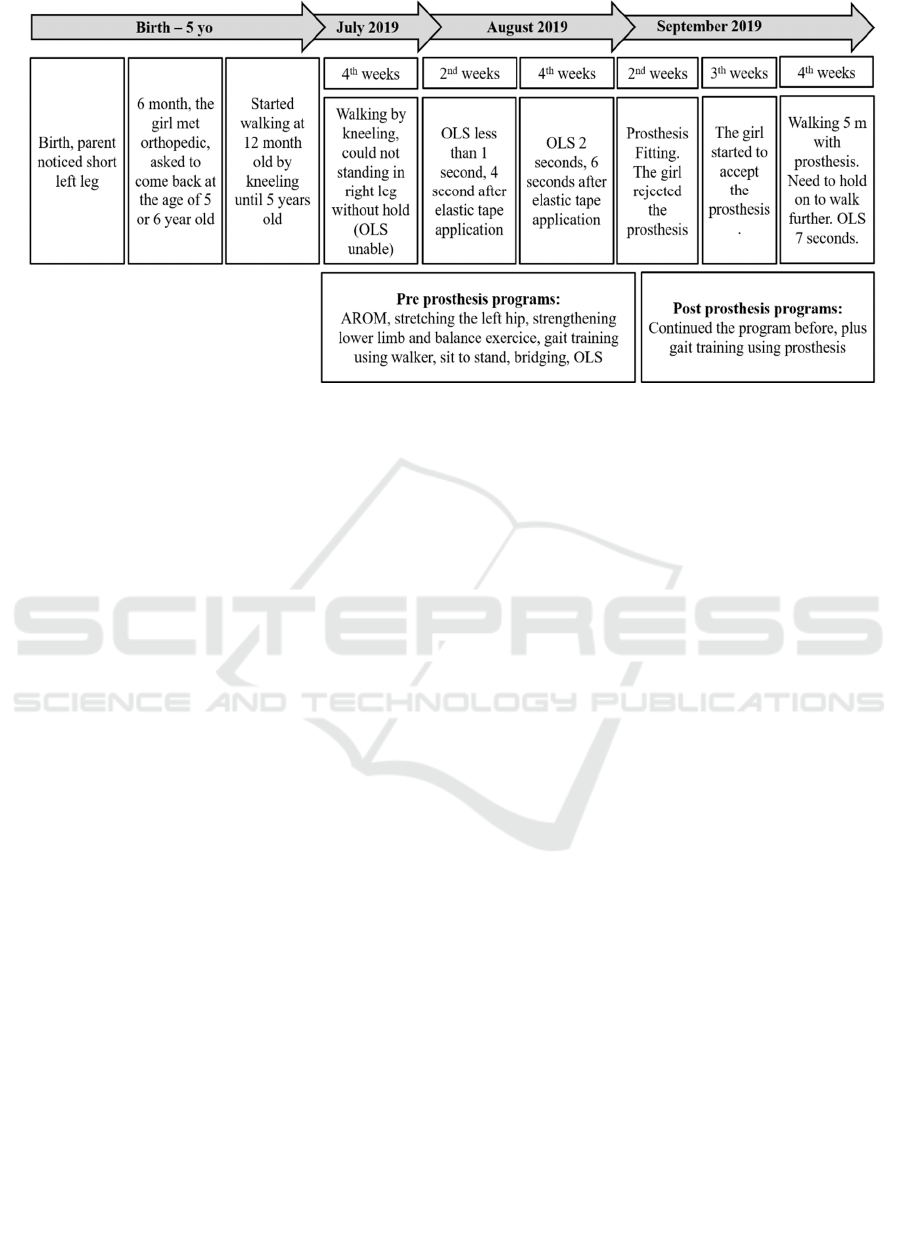
Figure 3: The timeline of the patient’s history. OLS: one leg stand. AROM: active range of motion
Late Referred Proximal Focal Deficiency: A Comprehensive Rehabilitation Management - A Case Report
133

this case, due to the socioeconomic conditions of the
patient and the location of the house which is quite
far from our hospital, we thought home-based
exercise program is the best option for the patient. In
this case, the result of home-based exercise mostly
depends on parent’s contribution. Adequate
education must be given. Prosthesis rejection also
became some issue in our rehabilitation program. It
took a week for the girl to accept her prosthesis and
started the gait exercise using a prosthesis. Postema
et al recommended the age of the first fitting for
upper-limb prosthesis, not more than 25 months.
Fitting after this age seems to be related to higher
rejection rates.The other systematic review by Meurs
et al said that fitting age of prosthesis depends on
clinical experience rather than evidence-based
(Meurs et al., 2006). The girl had difficulty to
control the knee unit given in the adaptive
prosthesis. The locked knee in full extension helped
the girl to walk better. The knee unit in children’s
first prosthesis rather difficult to control (Cummings,
2000). As the girl’s control of her prosthesis getting
better, the knee unit could be used. The myoelectric
prosthesis would be the best choice for this
condition (Tsukishiro, 2003). However, it would be
cost too much for the family.
For the future, the girl still needs to be routinely
evaluated. We continued to monitor for any redness
or blisters due to the use of prostheses. As the girl
continues to grow, the prosthesis would need several
times to adjust. The exercise should be done
regularly. It is important to improve ROM and
strength of both of the legs. The continuous
counseling for both the child and the parents would
be need.
4 CONCLUSIONS
It is important to know the characteristic of PFFD
and the treatment option we could offer to the
patient. Treatment of PFFD not as simple as to
choose between either prosthesis or surgery. We
need a comprehensive rehabilitation program that is
tailored as the patients need. We suggest the patients
with PFFD came to a physiatrist soon after birth.
REFERENCES
Abudu, A. et al. 2006. ‘The use of prostheses in skeletally
immature patients’, Orthopedic Clinics of North
America, 37(1), pp. 75–84. doi:
10.1016/j.ocl.2005.08.008.
Ackman, J. et al. 2013. ‘Long-term follow-up of Van Nes
rotationplasty in patients with congenital proximal
focal femoral deficiency’, Journal of Bone and Joint
Surgery - Series B. doi: 10.1302/0301-
620X.95B2.30853.
Alexander, M. A., and Matthews, D. J .2015. Pediatric
Rehabilitation, chapter 13: Pediatric Limb Deficiency.
Fifth Edition: Principles and Practice. pp 308 - 329
Barra, J. and Pérennou, D. 2013. ‘Is the sense of
verticality vestibular?’, Neurophysiologie Clinique.
doi: 10.1016/j.neucli.2013.02.001.
Chinn, L. et al. 2014. ‘Gait kinematics after taping in
participants with chronic ankle instability’, Journal of
Athletic Training. doi: 10.4085/1062-6050-49.3.08.
Clegg, A. et al. 2014. ‘The Home-based Older People’s
Exercise (HOPE) trial: A pilot randomised controlled
trial of a home-based exercise intervention for older
people with frailty’, Age and Ageing. doi:
10.1093/ageing/afu033.
Da Costa, C. S. N., Savelsbergh, G. and Rocha, N. A. C.
F. 2010. ‘Sit-to-Stand Movement in Children: A
Review’, Journal of Motor Behavior. doi:
10.1080/00222891003612763.
Cummings, D. R. 2000. ‘Pediatric prosthetics: Current
trends and future possibilities’, Physical Medicine and
Rehabilitation Clinics of North America.
D’Ambrosio, V. et al. 2016. ‘Prenatal diagnosis of
proximal focal femoral deficiency: Literature review
of prenatal sonographic findings’, Journal of Clinical
Ultrasound, 44(4), pp. 252–259. doi:
10.1002/jcu.22306.
Dillon, J. E. et al. 2005. ‘MR imaging of
congenital/developmental and acquired disorders of
the pediatric hip and pelvis’, Magnetic Resonance
Imaging Clinics of North America, 13(4), pp. 783–
797. doi: 10.1016/j.mric.2005.08.007.
Lasanianos, N. G. and Kanakaris, N. K. 2015. ‘Femoral
congenital deficiency’, in Trauma and Orthopaedic
Classifications: A Comprehensive Overview. doi:
10.1007/978-1-4471-6572-9_97.
Lasanianos, N. G., Kanakaris, N. K. and Giannoudis, P. V.
2015. ‘Trauma and orthopaedic classifications: A
comprehensive overview’, Trauma and Orthopaedic
Classifications: A Comprehensive Overview, pp. 1–
547. doi: 10.1007/978-1-4471-6572-9.
Lin, T. H. et al. 2013. ‘Prenatal diagnosis of proximal
femoral focal deficiency: A case report andliterature
review’, Taiwanese Journal of Obstetrics and
Gynecology. doi: 10.1016/j.tjog.2013.04.020.
Meurs, M. et al. 2006. ‘Prescription of the first prosthesis
and later use in children with congenital unilateral
upper limb deficiency: A systematic review’,
Prosthetics and Orthotics International, 30(2), pp.
165–173. doi: 10.1080/03093640600731710.
Tsukishiro, K. 2003. ‘Up-to-date Information on Upper
and Lower Extremity Prostheses’, Rigakuryoho
Kagaku. doi: 10.1589/rika.18.141.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
134
