
Exercise Training after Cardiac Surgery
Sri Wahyudati
Department of Physical Medicine and Rehabilitation, Dr. Kariadi General Hospital,
Faculty of Medicine, Universityof Diponegoro, Semarang, Indonesia
Keywords: Exercise Training, Cardiac Rehabilitation
Abstract: Exercise training is one important part of cardiac rehabilitation after cardiac surgery. This training is
aimed at improving exercise capacity and optimizing daily physical functioning concerning individual
physical activity limitations and participation restrictions. Exercise training should be started as early as
possible after cardiac surgery, which must be prescribed and supervised under medical guidance. In the
case of rehabilitation after cardiac surgery exercise training should be individually tailored according to
the clinical condition. Exercise training for patients after cardiac surgery has benefits in improving
exercise capacity, increasing muscular strength, improving graft patency and recovery of cardiac function
after surgery. Exercise training is a major component in cardiac rehabilitation programs has been proven
to be safe and effective in improving cardiac surgery patients' outcomes. Each cardiac rehabilitation
programs are tailored individually according to the clinical condition.
1 INTRODUCTION
Exercise training is one important part of Cardiac
Rehabilitation after Cardiac Surgery. This training
is aimed at improving exercise capacity and
optimizing daily physical functioning concerning
individual physical activity limitations and
participation restrictions and also can induce
inactive patients to develop and maintain an active
lifestyle, and consequently lower their future
cardiovascular risk. (Lavie CJ et.al, 2009; Taylor et
al, 2004) Cardiac rehabilitation (CR) itself usually
beginning during hospitalization (phase I,
inpatient), followed by a supervised outpatient
program lasting 3-6 months (phase II), and
continuing in a lifetime maintenance stage in
minimally supervised or unsupervised setting
(phase III). Physical activity counseling and
individually prescribed and supervised exercise
training are core components of a comprehensive
cardiac rehabilitation program, compromising 30–
50% (up to >70%) of all cardiac rehabilitation
activities. This applies to phase II as well as to
phase III cardiac rehabilitation for patients post-
acute coronary syndrome (ACS) and post-primary
coronary angioplasty (PCI), post-cardiac surgery
(coronary artery bypass, valve heart surgery, cardiac
transplantation), as well as in chronic heart failure
patients. Within large meta-analysis of the
Cochrane database, exercise training interventions
have been shown to reduce overall mortality rate of
patients with coronary artery disease by 27% (risk
reduction 0.73; con dence interval 0.54–0.98) and
mortality rate due to cardiovascular disease by 31%
(risk reduction 0.87, con dence interval 0.71–1.05).
(Jolliffe JA et al, 2001; Taylor RS et al, 2004)
Figure.1: Effectiveness of exercise only or exercise as
part of a comprehensive cardiac rehabilitation program on
all-cause mortality and cardiac mortality (according to
Jolliffe et al).
76
Wahyudati, S.
Exercise Training after Cardiac Surgery.
DOI: 10.5220/0009062800760081
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 76-81
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

There are some benefits of exercise training for
patients after cardiac surgery. They improve exercise
capacity, increase muscular strength, improves
ventilatory efficiency, and also can improve graft
patency and recovery of cardiac function. For
example, inpatient after CABG, exercise training
can improve exercise capacity, without significant
complications or other adverse effects. Kavanagh et
al reported exercise test data for 12,169 male
rehabilitation candidates and found the most
powerful predictor of cardiac and all-cause mortality
was VO2peak. Values of <15, 15 to 22, and >22
mL·kg-1·min-1 yielded respective hazard ratios of
1.00, 0.62, and 0.39 for cardiac deaths and 1.00,
0.66, and 0.45 for all-cause deaths. Additionally, the
mortality rate might decrease by 9% for each 1
mL·kg-1·min-1 increase of VO2peak. (Kavanagh T
et al, 2002)
Furthermore, exercise training also improves
cardiac function after surgery. Nakai et al. reported
the effects of exercise training on the recovery of
cardiac function and graft patency in 115 patients
after CABG. The patients were divided into Group I
(n = 60) and Group II (n = 55) without a CR
program. The rate of graft patency was 98% in
Group I and 80% in Group II. After training, the
exercise stroke index increased significantly in
Group I, but not in Group II. The result suggested
that physical exercise training should be started as
early as possible after CABG to improve graft
patency and recovery of cardiac function. Study by
Brügemann et al.also showed physical training
improves quality of life of patients, by comparing
two types of cardiac rehabilitation: physical training
plus information ('Fit' program) during 6 weeks or
comprehensive CR which, on top of the Fit-program,
included weekly psycho-education sessions and
relaxation therapy ('Fit-Plus' program) for 8 weeks.
The results showed that quality of life improved in
both treatment groups with time up to 9 months after
training, and there was no difference between the
two types of CR. (Brugemann J et al., 2007) Based
on many studies in multicentre of cardiology,
cardiac rehabilitation programs have evolved to be
an integral part of the standard of care in modern
cardiology. (Brugemann J et al., 2007; Eagle KA et
al., 2004)
2 DISCUSSION
Based on recommendation EACPR Committee
2010, in post-cardiac surgery, cardiac rehabilitation
in patients after coronary artery and valve heart
surgery should be consist of: (recommendation class
I, level evidence C)(Eagle KA et al., 2004; Vahanian
A et al., 2007; Butchart EG et al., 2005)
Physical activity counseling:
o Assess exercise capacity to guide exercise
prescription.
o Submaximal exercise stress test as soon as
after surgery. A maximal exercise test after
surgical wound stabilization.
o Recommended physical activity counseling
according to wound healing and exercise
capacity.
Exercise training recommendation
o Exercise training can be started early in-
hospital.
o Programs should last 2 – 4 weeks for in-
patient or up to 12 weeks for out-patient
settings.
o Upper-body training can begin when the
sternal wound is stable.
o Exercise training should be individually
tailored according to the clinical condition,
baseline exercise capacity, ventricular
function, and different valve surgery (after
mitral valve replacement exercise tolerance is
much lower than that after aortic valve
replacement, particularly if there is residual
pulmonary hypertension).
The following points are established/general
agreed on issues in exercise training applicable to all
clinical conditions : (Piepoli MF et al., 2010)
Assess exercise capacity by symptom-limited
stress testing, either on bicycle ergometer or on
a treadmill. In the routine clinical setting, this
is not always applicable, particularly in the
presence of left ventricular dysfunction
(ejection fraction 40%) or after recent surgical
intervention (because of the surgical wounds)
and therefore sub-maximal exercise evaluation
and/ or 6 min walk test should be considered.
Advise individualized exercise training after
careful clinical evaluation, including risk
stratification.
Recommend as general advice sub-maximal
endurance aerobic.
Educate on the recognition of symptoms
induced by effort. Appropriate behavior and re-
definition of exercise training target should be
discussed for the individual patient.
Expected outcomes: increased
cardiorespiratory fitness and enhanced
flexibility, muscular endurance, and strength;
reduction of symptoms, attenuated physiologic
Exercise Training after Cardiac Surgery
77

responses to physical challenges, and improved
psychosocial well-being.
Program settings. During the initial phases
supervised in-patient or hospital-based exercise
training programs may be recommended in
high-risk cardiovascular patients, i.e. those
with impaired systolic left ventricular function,
those with severe co-morbidities, leading to
significant disability, and in those with recent
(1 week) clinical destabilization. This will
verify individual responses and tolerability in a
safe clinical setting and will promptly identify
signs and symptoms indicating to modify or
terminate the program. The supervision should
include physical examination, assessment of
exercise-related symptoms or arrhythmias, and
monitoring of heart rate and blood pressure
before, during, and after exercise training. The
supervised period should be prolonged in
patients with new symptoms, clinical signs of
decompensation, blood pressure abnormalities,
and increased supraventricular or ventricular
arrhythmia during exercise.
There are a recommendation of exercise training
that generally applicable for secondary prevention in
patients with heart disease: (Piepoli MF et al., 2010)
Mode: Continuous endurance: walking,
jogging, cycling, swimming, rowing, stair
climbing, elliptical trainers, and aerobic
dancing.
Duration: At least 20–30 min (preferably 45–
60 min).
Most days (at least 3 days/week and preferably
6 – 7 days/ week.
Intensity: 50–80% of peak oxygen
consumption (close to the anaerobic threshold)
or peak heart rate or 40 – 60% of heart rate
reserve; 10/20–14/20 of the Borg Rating of
Perceived Exertion.
There are some differences in prescription in
patients after cardiac surgery. The following general
criteria should be considered in planning exercise
testing modality for exercise prescription in patients
after cardiac surgery: (Piepoli MF et al., 2010)
Safety
Co-morbidities: hemoglobin concentration
(Hb) values; muscular-skeletal discomfort,
healing issues at the incision sites
Associated factors: deconditioning due to
prolonged hospitalization, sedentary habits,
orthopedic limitations, occupational and
recreational needs.
Incomplete revascularization after CABG
surgery.
2.1 Exercise Prescription in Patients
After CABG.
Exercise prescription methodology is generally the
same as that used with CAD patients. Initially, some
patients may need lower-intensity or modified
exercise because of musculoskeletal discomfort or
healing issues at their incision sites, including not
only the chest but possibly also legs and arms.
Specifically, patients should completely refrain from
upper-extremity aerobic exercise training, for
example, arm ergometry and resistance training, for
4–6 weeks post-surgery to ensure the stability of the
sternum and sternal wound healing. The exception is
appropriate upper and lower body stretching and
flexibility exercises to promote mobility. In patients
with previous CABG, several aerobic training
intensities have proven effective the choice of which
will depend on both the level of exercise-related risk
and the patient's clinical condition. In this regard, it
must be borne in mind that, among patients entering
a rehabilitation program after a recent acute cardiac
event, those with recent CABG have been found to
have the lowest peak VO2. (Ades PA et al., 2006)
Because of the possibility of graft closure,
program staff should be alert for new patient
complaints of angina pectoris or angina-equivalent
symptoms or signs, such as exercise intolerance or
new ECG signs of myocardial ischemia. Patients
should also be educated regarding these possibilities.
Recognizing whether the revascularization was
complete or incomplete is valuable in this regard as
the latter may increase the likelihood of postsurgical
signs and symptoms of residual myocardial ischemia
during exercise, which may significantly affect the
results of the rehabilitation process.
2.2 Exercise Prescription in Patients
After Valve Repair/ Replacement
The exercise prescription and training of patients
with recent valve replacement or repair is very
similar to that used with CABG surgery patients.
However, the physical activity of some valvular
heart disease patients may have been very restricted
for an extended period before the surgical
intervention. Consequently, the resulting low
functional capacity may require these patients to
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
78
initiate, and proceed with, an exercise in a
conservative fashion, especially during the early
stages of the exercise training program. Exercise
intensities in the light to moderate and moderate to
high domains have been used in patients with recent
heart valve replacement or repair and balloon
valvuloplasty, demonstrating significant effects on
exercise capacity and quality of life. Preliminary
data also indicate a possible reverse left ventricular
remodeling effect of prolonged aerobic training in
patients with previous aortic valve replacement.
Anticoagulation therapy is very common in patients
who have undergone valve surgery; consequently,
this necessitates caution for exercise-related injuries
and subsequent bleeding. Staff should frequently
remind patients undergoing exercise training of the
increased risk of such events.
2.3 How to Define Exercise Intensity
Training intensity can be defined based on the
results of an exercise stress test. This should yield
maximal heart rate, maximal exercise load in watts,
possible ischemic threshold, and blood pressure
response to exercise. These data will form the basis
for determining the individual training load and
training heart rate. A complete cardiovascular
examination or more specific therapy has to take
place if cardiac complaints and/or symptoms arise
during the exercise stress test.
If complaints or symptom limitations persist,
despite maximal therapeutic efforts, it is crucial to
keep the exercise load at a level free of symptoms
and ischemia. It is generally recommended that the
training intensity should be clearly below the
ischemic threshold
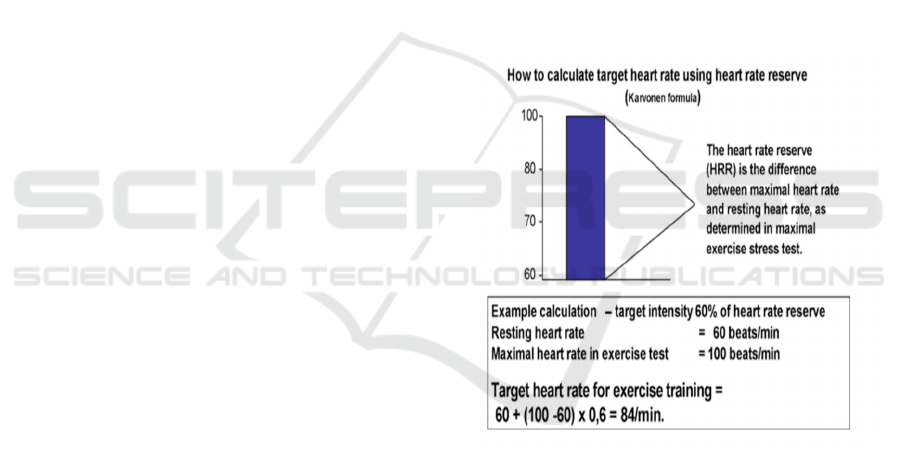
The heart rate is an objective, easily determined
parameter used to regulate and control exercise load
in cardiac rehabilitation. The maximal heart rate
(HRmax) is the highest heart rate achieved before
the termination of an incremental exercise tolerance
test due to subjective exhaustion or objective
indications. In cardiac rehabilitation, a training heart
rate of 60–75% HFmax (maximal heart rate) is
recommended. It is important to keep in mind that
only the heart rate response to an exercise stress test
performed under the patient’s actual medication can
be used for exercise prescription. This applies
especially to the use of ß-receptor blockers The
training heart rate can also be determined
mathematically by using the Karvonen formula, in
which the heart rate reserve (HRR) is calculated. In
cardiac patients, training heart rate of 40–60% of
heart rate reserve is recommended. The heart rate
reserve method should especially be used in patients
with chronotropic incompetence. The training heart
rate should always be determined clearly below the
ischemic threshold (i.e., 10 beats/min).
Maximal exercise capacity measured in watt is a
reliable and reproducible parameter to regulate
exercise training performed on a bicycle ergometer.
In cardiac rehabilitation, exercise intensity at 40–
60% (if tolerated up to 70–80%) of maximal load
(watt) achieved in a symptom-limited exercise test is
recommended. In patients with very low exercise
tolerance, very low heart rate reserve as well as with
the inability of the sinus node to react adequately to
exercise stress by increasing heart rate (patients with
chronotropic incompetence, atrial fibrillation,
pacemakers, and post-heart transplant) training
intensity should be controlled according to exercise
load in watts and by using the Borg scale.
Figure 2: How to determine the target heart rate for
exercise training in cardiac rehabilitation using the
Karvonen formula.
The Borg Scale (rate of perceived exertion, RPE)
is used to subjectively assess how the individual
perceives the intensity of the performed exercise on
a scale from 6 to 20. It is not advisable, however, to
solely rely on the Borg scale to regulate training load
as it contains too many influencing factors from the
patient’s perspective (i.e., unfamiliar method, poor
body awareness, over motivation, and peer
pressure). The Borg scale can be used as a
supplement to other training regulation options, as
well as to facilitate developing body awareness to
Exercise Training after Cardiac Surgery
79

the exercise load. Target values are RPE 11–14,
comparable to light to moderate exercise intensity.
Figure 3: The Borg- Scale
Maximal oxygen consumption (VO2peak)
reached during an exercise stress test and the oxygen
consumption at the anaerobic threshold (VO2-AT)
are meaningful parameters in regulating exercise
load during training. The latter can also be
determined during submaximal exercise testing,
independent of the individual's motivation level. If a
cardiopulmonary exercise test is used to determine
aerobic training intensity, then 40–70% of VO2peak
(up to 80% if tolerated) should be targeted, close to
the individual's anaerobic threshold.
Before doing exercise training in cardiac
patients, there are some contraindications for aerobic
endurance training that should be aware of some
conditions listed in table 1.
Table 1: Exercise Contraindication in Cardiac Patients.
Acute coronary syndrome (ACS)
Malignant hypertension with systolic blood
pressure >190 mmHg during exercise training
despite exhaustive antihypertensive medication
therapy
Drop-in systolic blood pressure by 320 mmHg
during exercise, in particular in patients with
coronary heart disease (CHD)
Severe secondary mitral valve insufficiency or
more specifically moderate mitral valve
insufficiency with evidence of increased
regurgitation during exercise
Heart failure NYHA IV
Supraventricular and ventricular arrhythmias
causing symptoms or hemodynamic compromise,
continual ventricular tachycardia
Frequent ventricular extra-systoles, known
continual ventricular tachycardia in advanced left
ventricular dysfunction or more specifically after
myocardial infarct as well as in response to
exercise or during the post-exercise regeneration
phase
Cardiovascular diseases that have not been risk
evaluated according to 4.1.3, and that have not
been treated according to guideline requirements in
terms of best possible prognosis outcome (i.e.,
Beta-blocker in patients with CHD, angiotensin-
converting enzyme-inhibitor in patients with heart
failure), or more specifically, hemodynamic
control (i.e., maximal medication therapy for blood
pressure regulation in severe arterial hypertension).
Patients with contraindications to exercise training
due to malignant arrhythmias, on the other hand,
can be introduced to a training program after
antiarrhythmic measures have been taken (i.e.,
implantable cardio de brillator (ICD), proven
efficacy of medication therapy)
3 CONCLUSION
Based on many studies, the clinical effect of
exercise training for patients after cardiac surgery
has benefits in improving exercise capacity,
increasing muscular strength, improving graft
patency and recovery of cardiac function after
surgery. Thus cardiac rehabilitation programs must
be given in advanced to patients who underwent
cardiac surgery. The programs are generally
exercised based and prescribed individually
according to the patient's special condition which
varies one another. According to that the cardiac
rehabilitation programs exercise’s prescription
which determined by exercise testing particularly is
safe.
Cardiac rehabilitation programs have become an
integral part of the standard of care in modern
cardiology. Their scope has shifted from the
emphasis on exercise therapy to a comprehensive
exercise measured approach that has many benefits
in supporting cardiac surgery patient outcomes. Each
cardiac rehabilitation programs are tailored
individually according to the clinical condition. In
most current guidelines of cardiovascular societies
worldwide cardiac rehabilitation is a class I
recommendation.
REFERENCES
Lavie CJ, Thomas RJ, Squires RW, et al, 2009. Exercise
training and cardiac rehabilitation in primary and
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
80

secondary prevention of coronary heart disease. Mayo
Clin Proc. 84(4):373–83.
Taylor RS, Brown A, Ebrahim S, et al, 2004. Exercise-
based rehabilitation for patients with coronary heart
disease: systematic review and meta-analysis of
randomized controlled trials. Am J Med. 116(10):682–
92. DOI: 10.1016/j.amjmed.2004.01.009.
Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N,
Ebrahim S. 2001. Exercise-based rehabilitation for
coronary heart disease. Cochrane Database Syst Rev
Update. (1): CD001800: Update Software.
Kavanagh T, Mertens DJ, Hamm LF, et al., 2002.
Prediction of long-term prognosis in 12,169 men
referred for cardiac rehabilitation. Circulation106:666-
71
Brügemann J, Poels BJ, Oosterwijk MH, et al. 2007. A
randomized controlled trial of cardiac rehabilitation
after revascularization. Int J Cardiol. 119:59-64.
Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy
GA, Gardner TJ, Hart JC, Herrmann HC, Hillis LD,
Hutter AM Jr, Lytle BW, Marlow RA, Nugent WC,
Orszulak TA, Antman EM, Smith SC Jr, Alpert JS,
Anderson JL, Faxon DP, Fuster V, Gibbons RJ,
Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA,
Jacobs AK, Ornato JP. 2004. ACC/AHA 2004
guideline update for coronary artery bypass graft
surgery: a report of the American College of
Cardiology/American Heart Association Task Force
on Practice Guidelines. 110:340 – 437.
Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R,
Filippatos G, Flachskampf F, Hall R, Iung B,
Kasprzak J, Nataf P, Tornos P, Torracca L, Wenink A,
2007. Guidelines on the management of valvular heart
disease: The Task Force on the Management of
Valvular Heart Disease of the European Society of
Cardiology. Eur Heart J. 28:230 – 268.
Butchart EG, Gohlke-Barwolf C, Antunes MJ, Tornos P,
De Caterina R, Cormier B, Prendergast B, Iung B,
Bjornstad H, Leport C, Hall RJ, Vahanian A. 2005.
Recommendations for the management of patients
after heart valve surgery. Eur Heart. 26:2463– 2471.
Piepoli MF et al. 2010. Secondary prevention through
cardiac rehabilitation: physical activity counseling and
exercise training. Eur Heart J. 31(16):1967-74.
Ades PA, Savage PD, Brawner CA, et al. 2006. Aerobic
capacity in patients entering cardiac rehabilitation.
113: 2706–2712.
Exercise Training after Cardiac Surgery
81
