
Return to Work Following Low Back Pain
Tanti Ajoe Kesoema
Department of Physical Medicine and Rehabilitation, Dr. Kariadi General Hospital,
Faculty of Medicine, University of Diponegoro, Semarang, Indonesia
Tantiajoe68@gmail.com
Keywords: Return to Work, Low Back Pain, Work Hardening
Abstract: Low back pain (LBP) is a highly prevalent cause of disability and one of the most expensive health
conditions. Along with personal suffering, LBP can result in decreased productivity and absenteeism. It is
also one of the leading causes of lost work time. Rather than viewing work resumption as a discrete event,
returning to work after an episode of work disability can be viewed as process that encompasses a series of
events, transitions, and phases, and includes interactions with other individuals and the environment. The
return to work (RTW) process is conceived of as the process workers go through to reach, or attempt to
reach, their RTW goal (typically a return to their pre-disability work participation). The process is thought
of as beginning at the onset of work disability and concluding when a satisfactory long-term outcome has
been achieved. A successful RTW coordination seems more based on ergonomics job accommodation,
communication, and conflict resolution rather than on medical or purely biomechanical knowledge. It is
very substantial for Rehabilitation Medicine to pay attention to this need to achieve the goal of LBP clients
to RTW successfully.
1 INTRODUCTION
In industrialized countries, a musculoskeletal
disorder of the back or low back pain is among the
leading causes of occupational injury and disability.
Even though in most cases patients make a full
recovery from an episode of low back pain (60-70 %
recover within 6 weeks, 70-90 % within 12 weeks)
this still adds up to a large amount of lost time from
work. Besides, the recurrence rate for low back
disorders is also very high. In one year, the
recurrence rate is between 20% - 44% and over a
lifetime recurrence of up to 85% is reported. It is
important to remember that once injured, the back
becomes more susceptible and re-injury is likely to
develop if there are risk factors in the workplace that
are not corrected.
Low back disorders include spinal disc problems
such as hernias and spondylolisthesis, muscle and
soft tissue injuries. In addition to the normal
degenerative aging process, epidemiological studies
reveal that poor ergonomic factors in the workplace
contribute to low back disorders in a healthy back or
accelerate existing changes in an already damaged
back. Poor ergonomic work factors increase the load
or strain on the back. This may arise from many
situations, for example, lifting, twisting, bending,
awkward movements, stretching, and static postures.
Tasks include physical work, manual handling and
vehicle driving (where whole-body vibration is
known to be another contributing factor).
Many reviews have been published of studies
concerning the risk factors of low back disorders,
including a multitude of physical, psychosocial
and/or personal risk factors. The evidence to link
psychosocial factors with low back disorders is
growing, especially where they occur at the same
time as the physical factors. The incidence of low
back disorders has also been strongly associated
with low job content and poor work organization.
Some work factors increase the risk of low back
disorder, one stated is physical aspects of work, such
as heavy physical work, lifting and handling of loads,
awkward posture (bending, twisting, static postures)
and whole-body vibration. While the other factor is
psychosocial work-related factors that relate to low
social support and low job satisfaction. One more
factor is work organization factors which include
poor work organization and low job content.
Workers should pay attention to these risk
factors when making an assessment and selecting
prevention measures. They include the
70
Kesoema, T.
Return to Work Following Low Back Pain.
DOI: 10.5220/0009062700700075
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 70-75
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

characteristics of the load (for example: is it heavy
or difficult to hold), physical effort required (for
example: strenuous; twisting; body in an unstable
position), characteristics of the working environment
(for example: not sufficient room or other
constraints on the posture of worker such as working
height too high or low; uneven or slippery flooring),
requirements of the activity (for example: prolonged
activity or effort; insufficient rest periods; excessive
distances to move loads; imposed work rate),
individual factors (for example: clothing etc.
restricting movement; inadequate knowledge or
training.
2 DISCUSSION
2.1 The Clinical Examination Of
Workers With LBP Complaints
A primary goal of the initial evaluation is to
distinguish low back pain/strain, which is generally
self-limited and is not associated with neurological
dysfunction, from the disorders of the low back
which are associated with neurological signs and
symptoms. The interview should obtain complete
occupational and medical history. Special emphasis
should be placed on the characteristic of the pain,
previous response to treatment if any. Work
modifications also should be explored, subjects may
be asked to fill in a standardized questionnaire for
screening.
The assessment should include an investigation
of the signs and symptoms of spinal abnormalities
and movement dysfunctions, especially of the lower
back, utilizing standardized approaches and tests.
When a series of positive so-called "Waddell signs"
should prompt the examiner to investigate
psychological problems or psychosomatic disorder.
2.2 RTW Prognosis
Many studies results indicated that it is important to
recognize patients who may be at risk of long-term
disability and failure to RTW. Definitions of long-
term disability and failure to RTW are important
from this point of view. Psychological and
occupational factors have a direct impact on RTW.
Female gender, lower educational level, longer
hospitalization period, greater BMI, biological age
exceeding 40 years, employment in manual labor,
lack of encouragement by the physician to RTW,
being in pain at the time of phone interview,
negative expectations about the outcome of surgery
preoperatively, and low work satisfaction were
associated with higher frequency of delayed RTW
and failed RTW. Appropriate strategies and
teamwork involving the patient, surgeon,
rehabilitation therapist, occupational medicine
specialist, and an employer could enhance RTW.
However, further investigations are required in this
respect.
To get a more detail acknowledgment of the
work-risk factor, a scheme was developed using a
different color of flags.
Figure 1: Synthesis of red, yellow, blue and black flags for
low back pain workers.
The purely biomedical model is insufficient to
explain the complexity of persistent LBP. Thus,
some so-called ‘‘psychosocial'' factors seem to be
frequently associated with LBP progressing to
chronicity. Furthermore, individual, occupational
and organizational factors influence the risk of
progressing towards long-term incapacity and never
returning to work. It is also recommended to
evaluate prognostic factors, i.e. psychological and
behavioral factors (‘yellow flags') that could
influence the progression to chronicity as well as
socio-economic and occupational factors (‘blue' and
‘black' flags), which could impact long-term work
incapacity and delay the RTW (Fig. 1). This
assessment may require several consultations or
interviews in complex cases and must be coupled
with a thorough search for clinical symptoms of
LBP severity (‘red flags') regardless of the LBP
stage: acute, subacute or chronic.
In Netherland, a systematic review was set out to
help find pieces of information about RTW
prediction. The goal was to answer this question:
What factors affect the time until RTW among
workers who are at the beginning of sick leave
related to low-back pain? A review team included 4
researchers from the Institute for Work & Health
Return to Work Following Low Back Pain
71

(IWH) and a fifth from a university in The
Netherlands. The researchers involved in the recent
review looked for articles related to prognosis, back
pain and return to work in 3 databases, published up
to April 2011. The initial search yielded 4,449
research papers. In the end, 30 papers from 25
different studies were considered relevant to the
systematic review question. The quality of each of
these studies was then assessed using a rating system.
Five studies were rated as high quality, 13 as
moderate quality and seven as lower quality.
The main findings were there was strong
evidence showing that the following
factors influence RTW among those with acute low-
back pain (as the synthesis model scheme above):
Workers' recovery expectations/beliefs (i.e.
their predictions about how likely it is they will
return to work and/or how long it will be
before they can return);
Workers’ interactions with health-care
providers (i.e. type of health-care provider seen
and nature of care received);
Workers’ self-reported pain and functional
limitations;
Presence of radiating pain (an indication of the
severity of the injury); and
Work-related factors, including physical
demands of the job, job satisfaction and the
offer of modified work.
The conclusions revealed workers’ recovery
expectations are the strongest predictor of return to
work, being supported by the most high-quality
studies. That is, those who expect to recover and
return to work more quickly, will do as expected.
Therefore, a simple question asking about recovery
expectations during the screening or assessment of
workers in the early stages of acute low-back pain
could help identify those at high risk of long work
absences and, in need of extra attention to help them
recover and return to work more quickly.
The next factor supported by strong evidence is
the nature of treatment care workers receive for their
acute low-back pain. In other words, the type of
health-care provider (and, thus, the type of care
provided) matters. For example, some studies show
that seeking care from a chiropractor result in a
shorter time on disability.
There is strong evidence to show workers’
reports about their pain intensity and functional
limitations are predictive of return to work: the
greater the self-reported pain and physical
limitations, the slower the return to work. Since both
can be easily measured in several ways with well-
validated questionnaires, they should be included in
assessments to determine those at high risk of long-
duration absences.
There is strong evidence to show that the
presence of radiating pain is associated with longer
periods off from work. However, radiating pain—
often used as a measure of injury severity—is
usually considered to be a "red flag" during clinical
assessments, an indication of potential neurological
problems that warrant further medical investigation.
For that reason, some people view this more as a
screening factor for more specific, less benign low-
back pain.
A few work-related factors are supported by
strong evidence as being predictive of return to
work. Physical job demands, as determined by
occupation, is one of them. That is, workers with
acute low-back pain who work in more physically
demanding jobs, such as construction or
manufacturing, are slower to return to work.
Job satisfaction is another work-related factor
shown to be predictive of RTW; the higher the
satisfaction, the more likely the return. Although job
satisfaction is probably related to any number of
factors at work, a simple question asking about job
satisfaction can be used at the very start of a work
disability process to identify those at high risk and in
need of extra attention.
The offeror availability of modified duties or
workplace accommodations is another work factor
associated with improved RTW outcomes.
Interestingly, it seems the offer of modified work,
not its actual implementation, predicts the likelihood
of a return to work.
The evidence did not point to depression as a
factor affecting RTW following acute low-back pain.
Neither did it point to pain catastrophizing. It could
be that both are not predictive of return to work until
back pain becomes chronic (long-term).
Finally, opioid use for pain management has been a
factor of great interest recently. However, it had not
yet been studied enough to show up as a predictive
factor in systematic reviews.
2.3 Functional Evaluation
Patients' perception of their incapacity is closely
related to the barriers involved in resuming activities,
especially RTW. Absence or low progression of the
patient's incapacity perception might mean that
obstacles to resuming activities and RTWdo exist
and need to be identified to be dealt with. Therefore,
it is recommended to evaluate early on and
repeatedly: pain, functional incapacity, and their
impact, as well as the main factors of work-related
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
72
long-term incapacity. Evaluating the functional pain
status of LBP patients enables, not only to quantify
the physical, social and occupational consequences
of LBP but also helps appreciate treatment
effectiveness. The impact of non-specific LBP can
be identified via pain self-evaluation and perceived
functional incapacity questionnaires but also using
functional capacities assessment tests (Table 1). Of
note, these parameters are related to each other in a
subtle manner and are influenced by multiple factors
and only a complete evaluation of the different pain
components can lead to a global vision of the pain
itself. Therefore, it is recommended to use the VAS
(Visual Analog Scale) (Table 1). It is also important
to periodically assess the workers' progress, give
them information back and above all support and
encourage them.
There is great variability in the objectives and
content of questionnaires evaluating the functional
impact and quality of life alterations related to LBP,
but only some are acceptable and validated: the
Roland-Morris questionnaire, the Oswestry and
Dallas questionnaires, the Quebec scale and SF-36
quality of life questionnaire (Table 1). Finally, the
evaluation of functional capacities validated by
physical tests can help write appropriate advice in
regards to the right time when patients may resume
work and/or which advice should be shared with
them. This functional capacity assessment should be
conducted each time a significant decrease in
activity or absenteeism can be suspected during the
progression of LBP. Several specific tools have been
developed but only a limited number of them have
been scientifically studied to document their
metrological properties, which vary according to
each tool (Blankenship System, ERGOS Work
Simulator, Ergo-Kit, Isernhagen Work System).
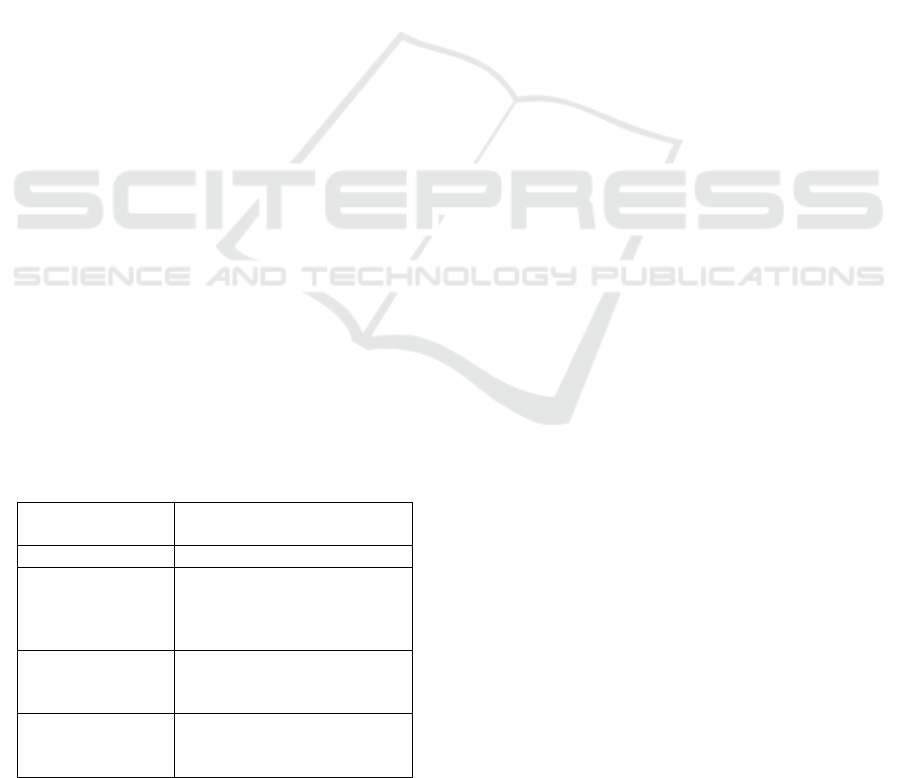
Table 1: Recommended tools for the assessment of low
back pain-related functional incapacity.
Assessed
parameters
Recommended tools
Pain
Visual Analog Scale (VAS)
Occupational
factors of
prolonged
incapacity
O¨rebro Musculoskeletal
Pain Screening Questionnaire
(O¨ MPQ)
Functional
incapacity
Roland-Morris Disability
Questionnaire and Dallas
Pain Questionnaire
Low back pain
worker’s beliefs
Work subscale of the Fear-
Avoidance Beliefs
Questionnaire
2.4 Coordination Of Intervention
Multidisciplinary Biopsychosocial Rehabilitation
(MBR) was defined as an intervention that involves
a physical component (for example an exercise
program) and at least one other element from the
biopsychosocial model, that is psychological or
social and occupational. The intervention program
had to have been delivered by clinicians from
different disciplines, which is a minimum of two
healthcare professionals from different professional
backgrounds who had to be involved in the
intervention delivery. The different components of
the intervention had to be offered as an integrated
program involving communication between the
providers responsible for the different components.
It is expected a full team which would include a
physiatrist, psychologists, physiotherapists, social
workers, occupational therapists, and orthotist.
Most recently, the interventions have focused on
the workplace environment to improve the support
of upper management and colleagues or reduce
work-related physical constraints. A successful
RTW coordination seems more based on ergonomics
job accommodation, communication, and conflict
resolution rather than on medical or purely
biomechanical knowledge. The pre-RTW
consultation(s) are precisely the right means to
promote dialogue between all actors involved and
the coordination of their actions.
2.5 Work Hardening
Work hardening is a work-oriented treatment
program that has an outcome that is measured in
terms of improvement in the client's productivity.
This is achieved through increased work tolerances,
improved work rate, mastery of pain (through the
effective use of symptom control techniques),
improved work habits, increased confidence, and
proficiency with work adaptations or assistive
devices. Work hardening involves the client in
highly structured, simulated work tasks in an
environment where expectations for basic worker
behaviors (e.g., timeliness, attendance, and dress)
are in keeping with workplace standards. The
ultimate goal of work hardening is to help the client
achieve a level of productivity that is acceptable in
the competitive labor market. This productivity
improvement is achieved at various levels through
the following techniques:
A decrease in secondary impairment effects.
Impairment is often magnified through disuse.
Return to Work Following Low Back Pain
73

Work hardening improves strength, flexibility,
and endurance.
A decrease in functional limitations. The
client's style of work and the quality of his or
her work behavior often increases the
functional decrement due to the impairment.
Work hardening helps the client learn effective
adaptive behaviors.
A decrease in disability. Disability is the
impact of functional impairment on the client's
societal roles, among which work roles are
prominent. Work hardening helps the client
reestablish many of these roles. Improvement
in these other areas generalizes to work roles
and results in a concomitant decrease in work-
related disability.
Improvement of vocational feasibility.
Feasibility, which is the client's acceptability as
an employee, is a key issue in work hardening.
Most clients with chronic industrial injuries
have not worked for several months. Thus,
work hardening identifies and remediates
potential problems with productivity, increases
safety in the workplace, and strengthens
interpersonal relations.
Improvement of employability. Employability,
which is the probability that the client will
achieve employment, is a consequence of the
levels of the client's work tolerances (e.g.,
ability to lift, carry, and stand) compared with
the tolerances of other workers in the general
labor market. Work hardening identifies and
develops these work tolerances.
A decrease in vocational handicap. The match
between the client and job can be improved by
increasing the client's level of function and by
modifying the job's critical work demands.
The role of the rehabilitation team in the WH
program should be made in uniform treatment
planning and patient management. The rehabilitation
team (which comprises the physiatrist and therapist
involved, at a minimum) is responsible for
assessment, treatment planning – including the
global and weekly goals – and therapy. The team
approach must also guarantee the"unité de
doctrine"[uniform doctrine] regarding the method
and program structure as well as the information that
is given to the client.
2.6 Symptoms of Negotiation Training
Many clients with chronic back pain cannot
"negotiate" effectively with their symptoms or cope
with their pain. They experience their symptoms as
being more or less beyond their control. As they
cannot predict the pain behavior, they feel unable to
exert control over their pain, themselves and their
environment. This, in turn, increases the lack of self-
efficacy. Symptom negotiation training is, therefore,
an important training element for these clients in a
WH program. It is based on the following principle:
when symptoms can be predicted, they can be better
controlled. To achieve this, the therapist must create
situations in which the symptoms appear predictably
and for which prediction and control by the client
are facilitated. The most important strategies for
symptom negotiation training are:
Graded activity
This approach is based on a task presenting a
gradually increased activity level. The starting point
and the increment are set by the therapist in such a
way that a clear relationship between activity and
symptoms can easily be felt by the client. For
example, in a progressive lifting test, load, lifting
height, speed or rate can be increased. The purpose
of this exercise is not, however, to evaluate lifting
performance, but to clarify the connections between
stress level of the ask and symptoms. Some clients
have initially to learn to differentiate pain levels as
shades of grey rather than as black-or-white (i.e.,
either no pain or catastrophic pain).
Graded exposure to eared movements
This method resembles the"graded activity", but
clients are exposed as realistically as possible to the
specific physical stress that they are afraid of: "For
example, if the patient fears the spinal compression
produced by riding a bicycle on a bumpy road, then
the graded exposure should include an activity that
mimics that specific activity, and not just a
stationary bicycle. Such an approach allows the
individual to correct inaccurate predictions about the
relationship between activities and harm".
Pacing
Clients with painful disabilities often function
according to an"on/off" principle ("Yes, I can"or"No,
I can't"). They should experience that by adjusting
their working pace there are intermediate options:
e.g., doing things slower, making short breaks, doing
some stretching, loosening up or relaxing exercises
in between, alternating work activities, etc.
Modification of working techniques, tools or
workplace. Many clients with pain-related
disabilities have not yet learned to appreciate the
value of working smart rather than working hard.
They keep on working as uneconomically as they
did before the accident/disease or even worse. Ways
of modifying working techniques and requirements
as well as tools and workplace should be evaluated.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
74

Coping with exacerbated pain
Exacerbation of pain during rehabilitation is a
challenge for a client's self-management and should
be used for the education of proper pain behavior.
Clients should learn to avoid panic and assess the
pain situation realistically, and to avoid, for instance,
alarmed consultations at emergency wards. They
should apply the learned self-treatments for pain
relief (e.g.cool packs, relaxation technics, the
meaningful use of medicaments) and analyze the
likely causes of the acute pain attack.
It is important to give a core message to the patient,
related to their back pain, at the beginning of the
WH program:
– Chronic pain does not mean harm! It is not
dangerous to move and stress your body when you
are in pain! This is necessary to escape from the
vicious circle of avoiding physical activity, loss of
fitness and pain;
– Chronic pain usually cannot be reduced in a short
time. However, it is possible to increase
performance capacity with intensive training despite
the pain. In many cases, a reduction in pain will then
occur in the long term;
– Some pain increase usually occurs at the start of
the program as under-used muscles and joints are
now trained, and the body has to readapt to higher
activity level. This is normal!
– In this program, the primary goal is not pain
reduction but increasing your performance capacity.
This will be measured weekly as the main criterion
for program goals. An intensive training program
creates the prerequisites for a successful return to
work.
To recommend discharge of WH program with a
return to a specific job, the team has to demonstrate,
based on results of FCE (Functional Capacity
Evaluation) tests, that the worker has reached the
goals stated in the plan or a plateau in his/her
functional levels. For those clients with a specific
job to return to, the care providers must document
the worker's ability about the job requirements, and
the discharge recommendations may consist of the
following options: return to work with full duty,
modified duty, or reasonable accommodations.
3 CONCLUSION
Studies' evidence to date shows certain factors can
be used to identify workers with acute low-back pain
who are at high risk of poor outcomes. The factors
identified in this review, such as recovery
expectations, interactions with health-care providers,
self-reported pain and physical limitations, and
physical demands of the job, could be used to screen
those workers at high risk of long-term or permanent
disability.
Work hardening is a new specialty within
rehabilitation. It is addressed by several different
disciplines among which occupational therapy has
taken a leadership position. Work hardening is an
important new approach to the rehabilitation of
injured workers and others whose entry into the
workforce is under consideration.
RTW is ultimately a social phenomenon that
requires a supportive social policy that will enable
all the players to work together. Although proper
individualized RTW coordination is useful and
important, it cannot overcome policies that
marginalize workers or interfere with safe and
sustainable RTW.
Because many of the analyzed studies have some
methodical shortcomings and multidisciplinary
return-to-work programs are expensive and need to
demonstrate their cost-effectiveness also in the long
term (to demonstrate their benefit and justify
reimbursement), there is still the need for high-
quality trials in this field to address issues such as
patient selection, the optimal intensity and duration
of programs, and the most effective treatment
components.
REFERENCES
De Beeck LR, Hermans Veerle Dr, 2000. Research on
work-related low back disorders. European Agency for
Safety and Health at Work, p. 4-6, 12-23. Available at
http://europa.eu.int
A. Petit, S. Rozenberg, J.B. Fassier, S. Rousseau e, P.
Mairiaux, Y. Roquelaure, 2015. Pre-return-to-work
medical consultation for low back pain workers. Good
practice recommendations based on systematic review
and expert consensus. Annals of Physical and
Rehabilitation Medicine 58.p. 298–304.
Lechner DE, 1994. Work Hardening and Work
Conditioning: Do they affect disability? Physical
therapy,p 74.
Darphin LE 1995 Work-Hardening and Work-
Conditioning Perspectives. In: The Comprehensive
Guide to Work Injury Management. (Ed. Susan J,
Isernhagen P).Gaithersburg, Maryland, Aspen
Publishers, p 443-62.
Return to Work Following Low Back Pain
75
