
Effect of High Frequency Transcranial Magnetic Stimulation on
Upper Extremity Motoric Function in Subacute Stroke Ischemic
Patient at Dr. Soetomo General Hospital Surabaya
Bastianus Alfian Juatmadja, Meisy Andriana, Yudith Dian Prawitri
Department of Physical Medicine and Rehabilitation, Dr. Soetomo General Hospital, Faculty of Medicine,
University of Airlangga, Surabaya, Indonesia
Keywords: Transcranial Magnetic Stimulation, Neuroplasticity, Fugl-Meyer Assessment, Upper Extremity Motoric
Function.
Abstract: Stroke cause motoric function disturbances that can decrease quality of life. Damaged brain caused by stroke
have an ability to repair itself which is called neuroplasticity. Transcranial Magnetic Stimulation (TMS) was
introduced as a non-invasive tool that could stimulate damaged brain hemisphere to increase neuroplasticity.
This study aimed to prove and determine the effect of Repetitive Transcranial Magnetic Stimulation (rTMS)
on upper extremity motoric function in subacute stroke ischemic patient. Eighteen subjects included in
inclusion criteria, divided into 2 groups, control and intervention group. Control group had conventional
therapy for 5 days consecutively and intervention group had conventional therapy and rTMS for 5 days
consecutively. Upper extremity motoric function was evaluated with Fugl-Meyer Assessment (FMA). It was
done before and after the intervention had completed. There were increasing of FMA score in control group
53.2 to 57.4 (p=0,012) and intervention group 40.3 to 54.1 (p=0,000). The increasing of FMA score in
intervention group was higher 13.7 vs 4.2 (p=0,000). Combination of conventional and TMS therapy
improved upper extremity function better than single conventional therapy in subacute stroke ischemic
patient.
1 INTRODUCTION
Stroke by definition is rapidly developing clinical
signs of focal (or global) disturbance of cerebral
function, lasting more than 24 hours or leading to
death, with no apparent cause other than that of
vascular origin. Stroke is the third caused lead to
death after cardiac disease and cancer. The
American Heart Association estimate there are
780.000 stroke patients per year. Stroke is the most
disabled disease. According to National Stroke
Association about 10% stroke may fully recovered
without sequelae, 25% may have sequelae, 40% may
have moderate to severe handicap (Zorowits, 2010;
Jauch et al., 2013).
Stroke prevalence according to Riset Kesehatan
Dasar (Riskesda) Health Ministry of Republic
Indonesia was increasing from 8.3 per 1000 people
at 2007 become 12.1 per 1000 people at 2013
(Riskesdas, 2013).
The brain has ability to “plastic” and able to
reorganize itself up to a certain degree of damage.
Many studies have documented the changes in
cortical organization that occur after motor stroke,
particularly on the side of the lesion. In addition,
there is a balance of function between the two
hemispheres that is controlled by interhemispheric
inhibition. The stroke affected hemisphere can be
doubly disabled, by the stroke itself and by an
imbalanced inhibition from the non-stroke
hemisphere (Khedr et al., 2009; Khedr et al., 2010).
Transcranial magnetic stimulation (TMS) was
introduced as a non-invasive tool for the
investigation of the motor cortex. TMSisbasedon
an electromagnetic coil applied to the scalp
producing an intense, localized magnetic field
which either excites or inhibits a focal cortical
area. The repetitive application (rTMS), causing
longer lasting effects, was used to study the
influence on a variety of cerebral functions. Low‐
frequency (≤1 Hz) rTMS is likely to cause
32
Juatmadja, B., Andriana, M. and Prawitri, Y.
Effect of High Frequency Transcranial Magnetic Stimulation on Upper Extremity Motoric Function in Subacute Stroke Ischemic Patient at Dr. Soetomo General Hospital Surabaya.
DOI: 10.5220/0009061800320036
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 32-36
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

inhibition of neuronal firing in a localized area,
whereas high‐frequency (≥1 Hz) rTMS inversely
leadstoneuronaldepolarizationunderthe
stimulatingcoil and to indirectly affect areas being
connected (Guse et al., 2009).
Safety is an important consideration because
rTMS could induce potential adverse effects such as
headaches and seizures. Twelve of the studies
reported that all patients tolerated the intervention
well without any adverse events; only 1 study
reported 4 subjects with mild, benign side effects of
headaches (2 subjects), anxiety (1 subject), and
fatigue (1 subject) (Lopez-Ibor et al., 2008; Hsu et
al., 2012).
Several trials have investigated the effect of
rTMS on upper limb motor function in patients with
stroke. High frequency rTMS over the primary
motor cortex (M1) in the affected hemisphere could
improve motor learning performance in patients with
chronic stroke and have a positive, long-term effect
on motor recovery in acute and subacute patients
with stroke (Khedr et al., 2010; Hsu et al., 2012).
However, other reports did not show measurable
therapeutic effects of rTMS on motor function after
stroke. There were inconsistent findings and
methodological discrepancies across these trials,
there is a lack of consensus regarding the effect of
rTMS on motor
recovery in patients with stroke
(
Chang et al., 2010; Hsu et al., 2012).
The Aim of this study is to prove and determine
the effect of Transcranial Magnetic Stimulation
(TMS) on upper extremity motoric function in
subacute stroke ischemic patient. The hypothesis of
this study is TMS may increase upper extremity
motoric function in subacute stroke ischemic patient.
2 METHODS
This study is an experimental randomized clinical
trial with two group design. Subjects were 18
subacute stroke ischemic patient who fulfilled
inclusions criteria that come to Physical Medicine
and Rehabilitation Outpatient Clinic Dr. Soetomo
General Hospital. The inclusions criteria were
subacute ischemic stroke, hemiparesis, willing to
follow instructions, willing to participate in this
study and signed an inform consent form. Exclusion
criteria were instability condition, seizure history,
brain injury history, pregnancy, aphasia, occipital
lobe lesion, wrist or hand contracture, metallic
medical equipment user. Drop out criteria were
unwilling to participate in this study, instability
condition while participating, headache along this
study and increase with rTMS intervention, Wong
Beker Pain Faces Scale > 4. Randomization was
done to divide subjects into 2 groups. 9 subjects in
control group did conventional therapy. 9 subjects in
intervention group did conventional therapy +
repetitive Transcranial Magnetic Stimulation.
Conventional therapy for 5 days. Repetitive
Transcranial Magnetic Stimulation for 5 days with
Neuro-MS/D, 8-shape coil, 10Hz, 100% Motor
threshold, 750 pulses per day, placed in primary
motor cortex area (M
1
).
Motoric function of upper extremity evaluated
with Fugl-Meyer Assessment (FMA) before and
after intervention had done (day-0 and day-5). The
Data from control and intervention group will be
evaluated intra-group and inter-group and analyze
with SPSS version 20. Intra-group data will be
analyzed with normality and homogeneity test. Intra-
group data will be analyzed with normality and
homogeneity test. If the data has normal distribution
and homogenous, paired t test will be used,
otherwise Wilcoxon Signed Rank Test. Inter-group
data will be analyzed with normality and
homogeneity test. If the data has normal distribution
and homogenous, independent t test will be used,
otherwise, Mann-Whitney test will be used. All
participants signed an informed consent form
approved by the Dr. Soetomo General Hospital
human subjects’ committee prior to participation in
the study.
3 RESULTS
The eighteen subacute stroke ischemic patients
fulfilled inclusions criteria were randomized and
divided into control and intervention group. All
subjects completed all sessions. Control and
intervention groups’ age and gender means in table
1. The FMA score before intervention between 2
groups showed in table 2. The analysis showed no
difference at subjects’ demographic data and FMA
score before intervention.
FMA score at control and
intervention group increased after intervention and
statistically significant intragroup. Intervention
group FMA score more significantly increased
compare to control group.
Effect of High Frequency Transcranial Magnetic Stimulation on Upper Extremity Motoric Function in Subacute Stroke Ischemic Patient at
Dr. Soetomo General Hospital Surabaya
33
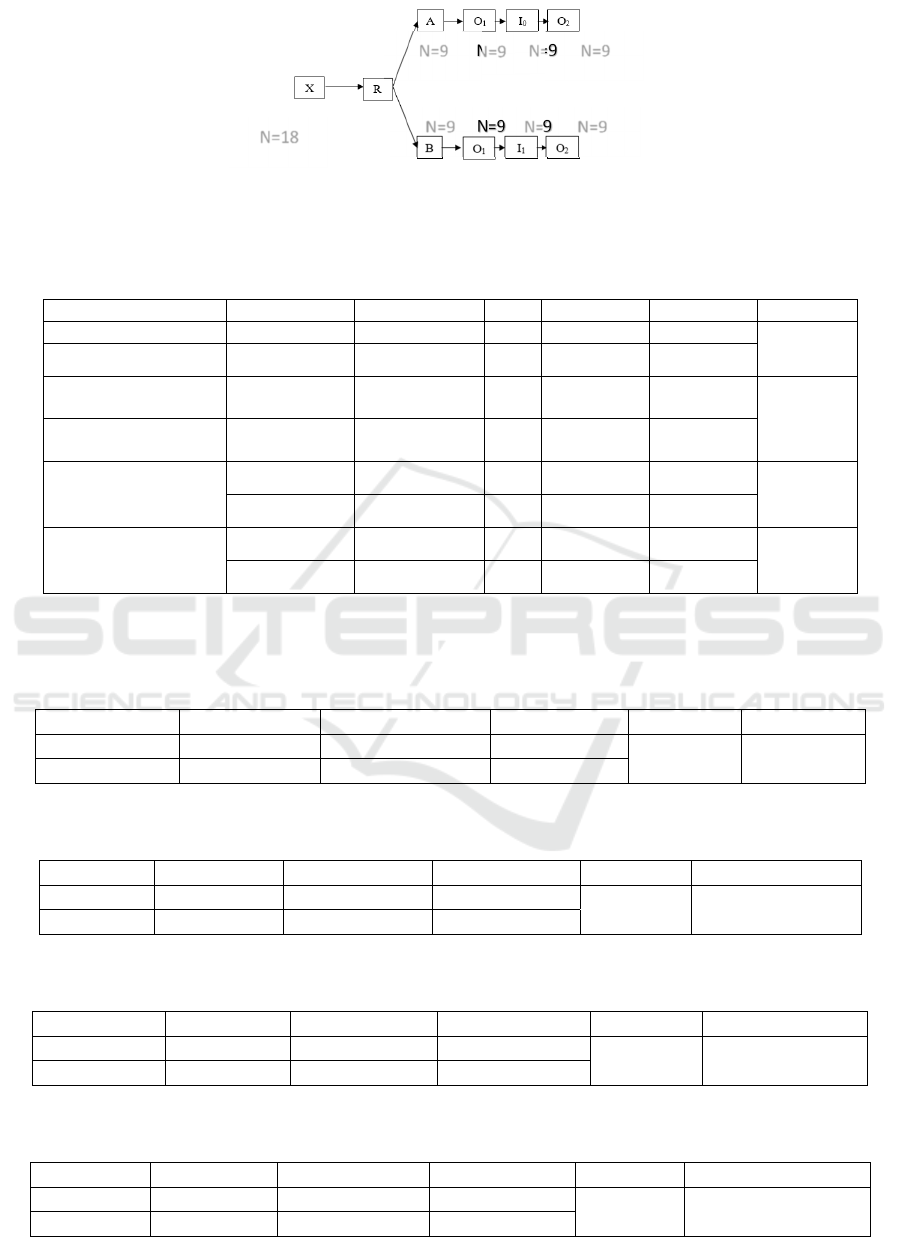
Figure 1: Study pathway. X: Subject; R: Randomization; A: Control Group; B: intervention Group; O1= First Fugl-Meyer
Assessment; O2: Final Fugl-Meyer Assessment; I0: Conventional Therapy; I1: Conventional Therapy + repetitive
Transcranial Magnetic Stimulation.
Table 1: Demographic Data.
Group N Mean SD P score
Age Intervention 9 55,556 ± 9,098
0,824
Control 9
54,889 ±9,892
Sex Intervention
Male
Female
6
3
6/3
0,257* /
0,576**
Control
Male
Female
8
1
8/1
Manual Muscle
Testing (Baseline)
Intervention 9
2,11 ±1,269
0,748
Control 9
2,00 ±1,323
Spasticity (Modified
Ashworth Scale)
Intervention
9 1,33 ±0,500
0,580
Control
9 1,56 ±0,726
Sample size (N); standard deviation (SD)
* Chi-Square test
** Fisher’s Exact test
Table 2: Fugl-Meyer Assessment score at control and intervention group before intervention.
Groups N Mean SD t p
Intervention
9 40.333 ±13.209
-1.969 0.067
Control
9 53.222 ±14.532
* Independent t-2 test; sampel size (N); Standar deviation (SD); p>0,05
Table 3:. Fugl-Meyer Assessment score at control group before and after intervention.
FMA Score N Mean SD t p
Before
9 53.222 ±14.532
3,223 0.012
After
9 57.444 ±11.303
* Independent t test; sampel size (N); Standar deviation (SD); p<0,05
Table 4: Fugl-Meyer Assessment score at intervention group before and after intervention.
FMA Score N Mean SD t p
Before 9 40.333
±13.209
10,271 0.000
After 9 54.111
±13.336
* Independent t test; sampel size (N); Standar deviation (SD); p<0,0001
Table 5: Increasing of Fugl-Meyer Assessment score at control and intervention group after intervention.
FMA Score N Mean SD t p
Intervention
9 13.777 ±4.024
5,096 0.000
Control
9 4.222 ±3.929
* Independent t test; sampel size (N); Standar deviation (SD); p<0,0001
N=9
N=9
N=9
N=9
N=9 N=9
N=18
N=9
N=9
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
34

4 DISCUSSIONS
There was no significantly difference Fugl-Meyer
Assessment score before intervention in both group.
This result may prevent ceiling effect bias. Not only
Fugl-Meyer Assessment score at control group after
intervention increased but also at
intervention group.
Fugl-Meyer Assessment score increase in control
group in line with other study that stated exercise
may enhance neuroplasticity. Physical training
(conventional therapy) upregulate the expression of
neurotrophic factors. It may improve neural
proliferation and survival and synaptic and axonal
plasticity by enhancing synapse formation, dendritic
growth, and remodeling. Numerous recent studies
indicated that early training promotes neuroplasticity
by acting on brain vasomotor activity and
angiogenesis, neurotrophic factor and apoptosis
marker expressions, brain inflammatory processes,
blood brain barrier (BBB) integrity, and muscle
activation control (Ploughman et al., 2009; Zhang et
al., 2013; Pin-Barre et al. Rajan et al., 2017).
Fugl-Meyer Assessment score at Intervention
group had more increase compare to control group
significantly. This study result was in line with the
other studies before. The meta-analysis study from
Hsu et al., suggests a clinically positive effect of
rTMS on motor recovery in the affected upper limb
of patients with stroke (Hsu et al., 2012).
Transcranial Magnetic Stimulation may be
capable of producing lasting changes in clinical
outcome after stroke. the combination of TMS with
conventional therapy leads to improved re-learning
of movement that produces lasting changes in the
organization of cortical motor output (Khedr et al.,
2009; Khedr et al., 2010).
Study from Rajan et al., showed that 5-day rTMS
enhances brain-derived neurotrophic factor (BDNF)
binding affinity for TrkB, BDNFTrkB signaling, and
NMDA receptor–TrkB interaction
14
. BDNF is one of
Neurotrophin that play a significant role in the
proliferation, migration, and phenotypic
differentiation of cells (neurogenesis) and ensure
their functional and structural integrity (Lasek-Bal et
al., 20015; Rajan et al., 2017).
Repetitive Transcranial Magnetic Stimulation is
safe. There was no side effect in this study. Lopez-
Ibor study on 2008 stated that only 4.5 % felt mild
and limited to transient scalp discomfort or pain.
There have been no deaths or epileptic seizures
reported in more than 10.000 treatment sessions in
published studies. The side effects are minimal and
well tolerated. There are no verified auditory or
cognitive deficits after rTMS (Lopez-Ibor et al.,
2008).
The limitations of these study are small number
of subjects and no blinded.
5 CONCLUSIONS
This study showed that combination of conventional
therapy and repetitive Transcranial Magnetic
Stimulation in 5 consecutive days improve upper
extremity motoric function significantly compare to
conventional therapy alone in subacute stroke
ischemic patient.
REFERENCES
Chang WH, Kim YH, Bang OY, Kim ST, Park YH, Lee
PK. 2010. Long-term Effects of rTMS on Motor
Recovery in Patients After Subacute Stroke. Journal of
Rehabilitation Medicine. 42:758 –764.
Guse B, Falkai P, Wobrock T. 2009. Cognitive Effects of
High-Frequency Repetitive Transcranial Magnetic
Stimulation: A Systematic Review. Journal of Neural
Transmission. 117 (1): 105 – 122.
Hsu WY, Cheng C, Liao K, Lee I, Lin Y. 2012. Effect of
Repetitive Transcranial Magnetic Simulation on Motor
Function in Patient with Stroke a Meta-analysis.
Journal of The American Heart Association. 43 (7):
1849 – 57.
Jauch EC, Saver JL, Adams HP, Bruno A, Connors JJ,
Demaerschalk BM, Khatri P, McMullan PW, Qureshi
AI, Rosenfield, K, Scott PA, Summers DR, Wang DZ,
Wintermark M, Yonas H. 2013. American Heart
Association. Guidelines for The Early Management of
Patients with Acute Ischemic Stroke.
Khedr EM, Abdel-Fadeil MR, Farghali A, Qaid M. 2009.
Role of 1 and 3 Hz Repetitive Transcranial Magnetic
Stimulation on Motor Function Recovery After Acute
Ischaemic Stroke. European Journal of Neurology. 16:
1323 – 1330.
Khedr EM, Etraby AE, Hemeda M, Nasef AM, Razek
AAE. 2010. Long-Term Effect of Repetitive
Transcranial Magnetic Stimulation on Motor Function
Recovery After Acute Ischemic Stroke. Acta
Neurologica Scandinavica. 121: 30–37.
Lasek-Bal A, Jędrzejowska-Szypułka H, Różycka J, Bal
W, Holecki M, Duława J, Lewin-Kowalik J. 2015.
Low Concentration of BDNF in The Acute Phase of
Ischemic Stroke as A Factor in Poor Prognosis in
Terms of Functional Status of Patients. Medical
Science Monitor. 21: 3900–3905
Lopez-Ibor JJ, Lopez-Ibor M, Pastrana J. 2008.
Transcranial Magnetic Stimulation. Current Opin in
Psychiatry. 21: 640 – 644.
Effect of High Frequency Transcranial Magnetic Stimulation on Upper Extremity Motoric Function in Subacute Stroke Ischemic Patient at
Dr. Soetomo General Hospital Surabaya
35

Pin-Barre C, Laurin J. 2015. Physical exercise as a
diagnostic, rehabilitation, and preventive tool:
influence on neuroplasticity and motor recovery after
stroke. Neural plasticity.15: 608581.
Ploughman M, Windle V, MacLellan CL, White N, Doré
JJ, Corbett D. 2009. Brain-derived neurotrophic factor
contributes to recovery of skilled reaching after focal
ischemia in rats. Stroke, 40 (4): 1490-1495.
Rajan ST, Ghilardi MF, Wang HY, Mazzon E, Bramanti
P, Restivo D, Quartarone A. 2017. Mechanism of
Action For rTMS: A Working Hypothesis Based on
Animal Studies. Frontiers in Physiology. 8: 457.
Riskesdas, 2013. Riset Kesehatan Dasar. Jakarta: Badan
Penelitian dan Pengembangan Kesehatan Kementerian
Kesehatan RI
Zhang L, Hu X, Luo J, Li L, Chen X, Huang R, Pei Z.
2013. Physical Exercise Improves Functional
Recovery Through Mitigation of Autophagy,
Attenuation of Apoptosis and Enhancement of
Neurogenesis After MCAO in Rats. BMC
neuroscience. 14 (1): 46
Zorowits RD. 2010. Stroke. In: Cuccurullo SJ: Physical
Medicine and Rehabilitation Board Review. 2nd ed.
New York: Demos medical, pp. 40-87.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
36
