
The Comparison of Sarcopenia Prevalence between
Elderly in Community Dwelling and Nursing Home
Based on Indonesian Young Adult Cut-Off Point
Maria Regina Rachmawati
1,2,3
, Siti Annisa Nuhonni
4
, Tirza Z. Tamin
3,4
, Magdalena Wartono
1
, Dian
Mediana
1
, Debora Pranata
3
, Qraxina Chaidir
3
1
Faculty of Medicine, University of Trisakti, Jakarta Barat
2
Faculty of Medicine, University of Gunadarma, Depok
3
Research and Development of Indonesian Association of Physical Medicine and Rehabilitation (PERDOSRI)
4
Faculty of Medicine, University of Indonesia, Jakarta; Cipto Mangunkusumo National Hospital, Jakarta
Keywords: Sarcopenia, Elderly, Appendicular Skeletal Muscle Mass, Handgrip Strength, Gait Speed
Abstract: Sarcopenia is a progressive loss of skeletal muscle mass and strength that can decrease quality of life. This
study aimed to find a cut-off point of appendicular skeletas muscle mass (ASM), hand grip strength (HGS),
and gait speed (GS) from young adult, as a based value to defined the Sarcopenia in elderly; and to find the
differences values of sarcopenia between elderly in community dwelling and nursing home. Subjects
recruited by simple random sampling and convenience sampling. There were 369 young adults (44% male,
56% female), 183 elderly (47% male, 53% female) on community dwelling, and 62 elderly (40% male, 60%
female) on nursing home. Cut-off point from young adult for ASM, HGS, and GS for male and female were
8,1 and 5,6 Kg/m
2
, 32 and 20 Kg, and 1,2 and 1,17 m/sec. The value of ASM, HGS, and GS in male from
community dwelling were higher (8,8 vs 7,5 Kg/m
2
(p<0,001), 25,9 vs 17,7 Kg (p<0,001), and 1,5 vs 0,8
(p<0,001), while the value of GS in female from community dwelling were higher 1,3 vs 0,73 m/sec
(p=0,008), and similar on ASM and HGS. The percentage of lower ASM, HGS, and GS in male were all
higher on elderly from nursing home; 28% vs 60% (p<0,026), 82% vs 99% (p<0,001), and 28% vs 88%
(p<0,001), as well as in female 5% vs 5,4% (p<0,001), 70% vs 86,2% (p<0,001), and 34% vs 100%
(p<0,001). There were cut-off point based on Indonesian young adult to determination the sarcopenia in
elderly, and the elderly from nursing home have a lower muscle mass and performance, especially in male.
1 INTRODUCTION
Sarcopenia is a major clinical problem and a quite
commonly treatable geriatric condition (Moreira,
Perez and Lourenço, 2019;! Shafiee et al., 2017). It
defined as an age related loss muscle accompanied
by a reduction in muscle strength and function
(Rodríguez-Rejón et al., 2019; Abe et al., 2011;
Milanović et al., 2013). Progressive loss of skeletal
muscle mass and strength as the individual gets
older often contribute to numerous negative health
outcomes, such as disability, functional impairment,
increased risk of falls, hospitalisation, decreased
quality of life and increased risk of mortality
(Santilli et al., 2014,!Lees et al., 2019).
In addition, sarcopenia is a potentially modifiable
risk factor for health status, risk of falls, and
fractures in elderly. So, an early detection of
sarcopenia is important to prevent progressive
reduction in skeletal muscle mass and function
(Yeung et al., 2019;!Lees et al., 2019).
Based on International Working Group on
Sarcopenia (IWGS) and Asian Working Group for
Sarcopenia (AWGS), sarcopenia is defined as low
muscle mass and low muscle strength, and/or low
physical performance, that can be measured by
appendicular muscle mass divided by the height
squared, the handgrip strength, and/or gait
speed.(Chumlea et al., 2011,!Chen et al., 2014)
The definitions of sarcopenia provided by
EWGSOP, IWGS, and AWGS were based on
different methods and different cut-off points to
define loss of muscle mass, reduction in muscle
strength, and low gait speed (Chumlea et al., 2011;
Chen et al., 2014; Carvalho do Nascimento, Poitras
and Bilodeau, 2018). The measurement of muscle
Rachmawati, M., Nuhonni, S., Tamin, T., Wartono, M., Mediana, D., Pranata, D. and Chaidir, Q.
The Comparison of Sarcopenia Prevalence between Elderly in Community Dwelling and Nursing Home based on Indonesian Young Adult Cut-Off Point.
DOI: 10.5220/0009035500050011
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 5-11
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
5

mass along with muscle performance were assessed
using hand grip strength and gait speed.Muscle mass
were measured using Body Impedance Analysis
calculated in (Kg)/body height (m
2
), hand grip
strength were evaluated using Jamar Hand Grip (kg),
and gait speed were calculated by measuring gait
speed (second) on four meter track of gait (m/sec)
(Cruz-Jentoft et al., 2010;!Bahat et al., 2016; Yeung
et al., 2019)
The elderly population in the world, as well as in
Indonesia, continues to grow throughout the
following years and decades. Based on the statistic
data, elderly population in Indonesia on 2010 took
up as much as 7.6% of the total population,
increasing up to 8.5% in 2015, and the population
were estimated to have expected increase up to a
total of 10% in 2020 (Depkes RI, 2016). However,
research on the prevalence of sarcopenia in
Indonesia is still limited, as well as the lack of
further research to determine the cut-off point for
skeletal muscle mass, muscle strength, and/or gait
speed in Indonesia. Since the cut-off point of muscle
mass, handgrip strength and gait speed varies among
countries and populations, the measurement on
young adult is necessary to be done as a standard in
every country. (Chen et al., 2014; Bahat et al., 2016;
Yeung et al., 2019)
Determination of sarcopenia in elderly were
based on – 2 standard deviation or lowest quartile of
normal value of muscle mass, hand grip strength,
and gait speed in young adult. Young subjects as the
standard value are required to be in perfect health,
without history or current chronic disease or chronic
drug usage as a reference population for assessing
muscle mass (Bahat et al., 2016).
Based on previous study on Asian working group
for sarcopenia in elderly population above 65 years,
diagnosis of sarcopenia in Taiwan were established
based on skeletal muscle index (SMI) 2 SD below
normal young adult were <8,87Kg/m
2
( 23,6%
male); <6,42 Kg/m
2
(18,6% female), while in Japan
it was established based on Appendicular skeletal
muscle (ASM) 2 SD below young adult values were
< 7,0 Kg/m
2
(11,3% male); <5,8 Kg/m
2
(10,7%
female); ≤ 6,42 Kg/m
2
(22,1% female), and in Korea
based on ASM were 6,75 Kg/m
2
(21,8% male);
<5,07 Kg/m
2
(22,1% female) (Chen et al., 2014).
The value of hand grip strength (HGS) based on
lowest quartile in young adult in Japan were 30,3 Kg
(male), and 19,3 kg (female), while HGS value
based on Asian Working Group of Sarcopenia in
<18 kg for females and <26 kg for males were
considered as cut-off points for the definition of
sarcopenia. In Taiwan, HGS value based on
European Working Group of Sarcopenia (EWGSOP)
recommendation and adjusted according to Asia data
were <22,4 Kg (male), and <14,3 Kg (female). (6,9)
The physical performance quality assessed by
measurement of gait speed (GS) in Japan, based on
the lowest quartile of study group were measured
within the standard of <1,27m/s (11,3% male);
<1,19 m/s (10,7% female); ≤ 1,22 m/s (22,1%
female). In Taiwan, the standard used are ≤ 1 m/s, be
it for male or female (Chen et al., 2014).
This study aimed to find the cut-off point of
skeletal muscle mass, handgrip strength, and gait
speed in Indonesian young adult, as a reference for
determining the prevalence of sarcopenia, and also
the differences between elderly who lived in
community dwelling and nursing home.
2 METHODS
The method design of this study was cross-sectional.
The community dwelling elderly were recruited
from an outpatient setting in one of the private
hospital on South Tangerang, and elderly subjects
who lived in nursing home were recruited from a
social nursing home located in Cengkareng, West
Jakarta. All subjects were male and female above 60
years old who were able to walk without walking
aid, able to grip, and in good health. Subjects with
cardiac failure, chronic obstructive pulmonary
disease, acute asthma were excluded.
The young adult group were recruited from one
of the private university in West Jakarta. Inclusion
criteria for the subjects of the young adult group
includes: age range between 17-25 years old, with
good health condition, are able to walk without
walking aids, able to grip, no history of chronic
disease, and did not consume any drugs.
Ethical clearance were previously approved by the
ethics committee with 128/KER/FK/III/2018 ethical
clearance number. Data collection was conducted
between June 2018 and December 2018.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
6

Figure 1: Body Impedance Analysis data sampling.
Figure 2: HGS data sampling.
Figure 3: Gait speed data sampling.
All included subjects agreed to perform several
tests; the measurement of appendicular skeletal
muscle mass (ASM) in Kg/m
2
using “TANITA”
body impedance analysis, hand grip strength (HGS)
in Kg using Jamar Hand Grip, and gait speed (GS) in
m/sec evaluated by measuring the time on four
meter gait test using stopwatch.
3 RESULTS
There were 369 young adult subjects included in the
study. The subjects consisted of 163 male (44%) and
206 female (56%), and for the elderly subjects
group, there were 183 elderly subjects from
community dwellings with 86 male (47%) and 97
female (53%); and 62 elderly subjects from nursing
home consisted of 25 male (40%) and 37 female
(60%). The characteristic of the young adult and
elderly subjects are listed on the table 1.
The cut-off value of ASM, HGS, and GS based
on young male listed in table 2 were 8,1 Kg/m
2
; 32
Kg; and 1,2 m/sec, while cut-off value of ASM,
HGS, and GS based on young female were 5,6
Kg/m
2
; 20 Kg; and 1,17 m/sec.
Table 3 showed that the value of ASM, HGS,
and GS of elderly male subjects from nursing home
were significantly lower (p= <0,001, p<0,001,
p<0,001). The value of ASM and HGS were quite
similar between the elderly female subjects groups
(p=0,1 and p=0,9), while the GS value of the nursing
home elderly female subjects group were
significantly lower compared to the community
dwelling elderly subjects group (p=0,008).
The data listed in Table 4 have shown percentage
of lower values of ASM, HGS, and GS male and
female from nursing home were higher (p=0,026,
p<0,001, p<0,001), examined by Mc Nemar test.
The Comparison of Sarcopenia Prevalence between Elderly in Community Dwelling and Nursing Home based on Indonesian Young Adult
Cut-Off Point
7
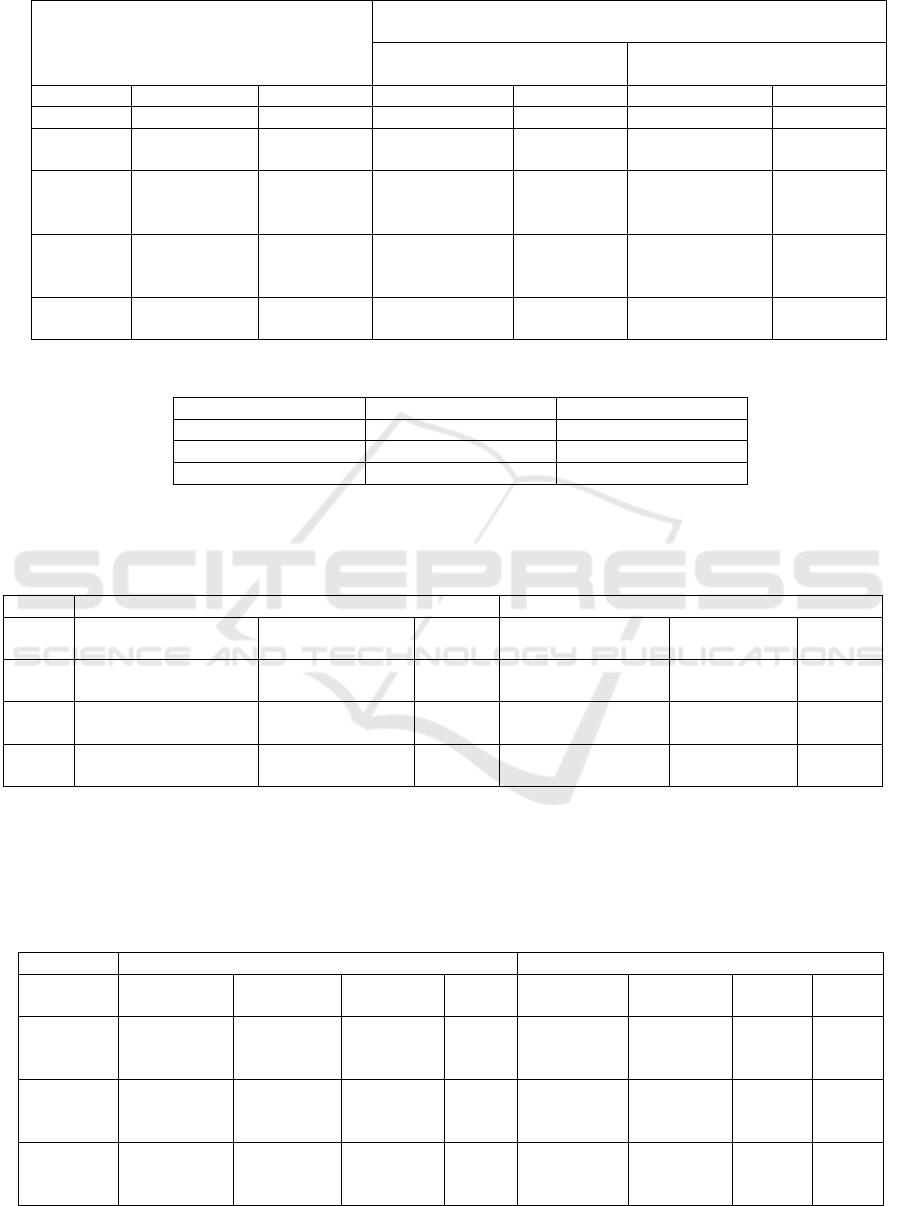
Table 1: Characteristics of the young adult and elderly subjects.
Young adult
N=369
Elderly
Community dwellings
N=183
Nursing home
N= 62
Male
Female
Male
Female
Male
Female
Total
163 (44%)
206 (56%)
86 (47%)
97 (53%)
25 (40%)
37 (60%)
Age
(years)
20
(17-24)
19
(17-25)
68,5
(60-87)
67
(60-87)
62,6±
9,5
65±10
Body
weight
(Kg)
69,6 ± 12,6
55,6 ± 10,9
67±
12,2
60,6±
9,8
55±12
50±9
Body
height
(cm)
169,3±6
156±5,7
165 (142-183)
152 (141-
165)
153,6±9,2
141±
7,2
BMI
(Kg/m
2
)
24,3±4
22 (15,5-
37,6)
24,9 (16,7-40,9)
26,9 (17,6-
45,9)
22,2±
4,5
25±4.1
Table 2: The Cut-off Values of Appendicular Muscle Mass, Hand Grip Strength, and Gait Speed in young adult subjects.
Male
Female
ASM (Kg/m
2
)
2SD: 8,1
25% percentile: 5,6
HGS (Kg)
25% percentile: 32
25% percentile: 20
GS (m/sec)
25% percentile: 1,2
25% percentile: 1,17
Table 3: Value difference of the Appendicular Skeletal Muscle Mass, Hand Grip Strength, and Gait Speed on elderly
subjects between community dwelling and nursing home settings.
Male
Female
Community Dwelling
N=86
Nursing home
N=25
p
Community Dwelling
N=97
Nursing home
N=37
p
ASM
(Kg/m
2
)
8,8
(5.6-14.9)
7,5 ± 1,4
<0,001*
6,8
(4,9-11)
6,6
(4,9-10)
0,1
HGS
(Kg)
25,9 ± 6,8
17,7± 5,6
<0,001**
18 (8-31)
11,8 ± 5,8
0,9
GS
(m/sec)
1,5 ± 0,4
0,84± 0,24
<0,001**
1,3 ± 0,3
0,73 ± 0,2
0,008**
* Mann-Whitney Test
** T-test
Table 4: The percentage differences of lower ASM, HGS and GS between elderly in community dwelling and nursing
home.
Male
Female
Cut-off
Value
Community
Dwelling
Nursing
home
P
Cut-off
Value
Community
Dwelling
Nursing
home
P
ASM
(Kg/ m
2
)
2SD:
8,1
28%
60%
<0,026
25%
percentile:
5,6
5%
5,4%
<0,001
HGS
(Kg)
25%
percentile :
32
82%
99%
<0,001
25%
percentile:
20
70%
86,2%
<0,001
GS
(m/ sec)
25%
percentile:
1,2
28%
88%
<0,001
25%
percentile:
1,17
34%
100%
<0,001
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
8

4 DISCUSSION
This study found that the value of – 2 SD of the
ASM from the young male were 8,1 Kg/m
2
, which
is a bit lower than the ASM of the young male in
Taiwan (8,82 Kg/m
2
), and higher than Japan (7,0
Kg/m
2
) and Korea (6,75 Kg/m
2
). While the lowest
quartile of the ASM from the young female were 5,6
Kg/m
2
, that was lower than Taiwan (<6,42 Kg/m
2
)
and Japan (< 5,8 Kg/m
2
), and higher than Korea (<
5,07 Kg/m
2
). The lowest quartile of HGS in young
male was 32 Kg, higher than Japan (30,3 Kg) and
EWGSOP to Asia data (22,4 Kg). Furthermore, the
lowest quartile of HGS in young female from this
study was 20 Kg, higher than Japan (19,3 Kg) and
EWGSOP recommendation (14,3 Kg). The study
result of the lowest quartile of the GS in young male
was 1,2 m/sec, is a bit lower than in Japan (1,27
m/sec), yet still higher than the Taiwan study (< 1
m/sec). The lowest quartile of the GS in young
female from this study was 1,17 m/sec, slightly
lower than Japan (1,19 m/sec) and a bit higher than
Taiwan (1 m/sec) (Chen et al., 2014).
The value of ASM, HGS, and GS of elderly male
subjects from community dwelling home were
significantly higher; 8,8 (5,6-14,9) vs 7,5 ± 1,4
Kg/M
2
(p<0,001); 25,9 ± 6,8 vs 17,7± 5,6 Kg (p<
0,001, and 1,5 ± 0,4 vs 0,84± 0,24 m/sec (p<0,001).
However, the ASM and the HGS in elderly female
subjects were shown slightly higher in female from
community dwelling home, but statistically no
difference between community dwelling and nursing
home subjects; 6,8 (4,9-11) vs 6,6 (4,9-10) Kg/m
2
(p=0,1); 18 (8-31) vs 11,8 ± 5,8 kg (p=0,9) , while
the GS of elderly female subjects in community
dwelling settings was higher; 1,3 ± 0,3 vs 0,73 ± 0,2
m/sec (p=0,008).
The percentage of the lower ASM, HGS, and GS
in elderly male from community dwellings were
lower; 28% and 60% (p<0,026); 82% and 99%
(p<0,001); 28% and 88% (<0,001). As well as in
elderly female subjects, the percentage of the lower
ASM, HGS, and GS from community dwellings
were lower than in nursing home; 5% and 5,4%
(<0,001); 70% and 86,2% (p<0,002); 34% and 100%
(p<0,002).
The prevalence of sarcopenia increases in a
nursing home setting. The results of this study are
consistent with previous studies, showing that there
is a close association between the degree of
sarcopenia and the degree of dependence among
residents (Buckinx et al, 2017). This results also
consistent with one of the multi-center study from
Spanish, stating that sarcopenia is a frequent
condition in elderly population who lived in a
nursing home, especially among female. (Salvà et
al., 2016). Although, in this study, elderly male in
nursing home have lower value of ASM, HGS and
GS, while elderly female in nursing home only have
lower value in GS.
Elderly skeletal muscle performance is regulated
by some factors, such as nervous, muscular, and
skeletal systems. These factors are influenced by
lifestyle, biological, and psychosocial factors.
Lifestyle factors including physical activity and
nutritional intake; biological factors including
genetics, hormones, and low-grade inflammation;
psychosocial factors including fear of falling,
psychological resiliency, self-efficacy, and
loneliness (Tieland, Trouwborst and Clark, 2017).!
Based on systemic review and meta-analysis study
conducted by Shen Y, et al, the review also said that
malnutrition was quite common in nursing home
setting, and it appeared to be an independently
associated factor of sarcopenia (Shen et al., 2019).
This study found that the prevalence of sarcopenia
was higher in nursing home than in the community
dwelling. It can be caused by low physical activity
in nursing home, low nutrition intake, and some
other psychological problem, because nursing home
usually don’t have any family that can support them,
so they usually lacking motivation to be active.
The percentage of the lower ASM in elderly
male subjects from community dwellings (28%) and
nursing home (60%) were significantly higher than
previous study in Taiwan (23,6%), Japan (11,3%),
and Korea (21,8%). While the lower ASM in elderly
female subjects from community dwellings (5%)
and nursing home (5,4%) were lower than earlier
study in Taiwan (18,6%), Japan (10,7% and 22,1%),
and Korea (22,1%) (Chen et al., 2014).
The prevalence of the lower physical
performance by measuremalet of gait speed in this
study of elderly male subjects from community
dwellings (28%) and in nursing home setting (88%)
were higher than the Japanesestudy (11,3%). As well
as the lower gait speed in elderly female subjects
from community dwellings (34%) and nursing home
(100%) were higher than elderly female subjects in
the Japanese study (22,1%) (Chen et al., 2014).
The limitations of this study were each group of
the adult and elderly subjects were recruited only
from one location.
The Comparison of Sarcopenia Prevalence between Elderly in Community Dwelling and Nursing Home based on Indonesian Young Adult
Cut-Off Point
9

5 CONCLUSIONS
Based on this study, Sarcopenia in Indonesia can be
determined by cut-off point from young adult values
for the ASM; <8,1 Kg/M
2
(male) and <5,6 Kg/M
2
(female), the HGS; < 32 Kg (male) and <20 Kg
(female), and the GS; < 1,2 M/sec (male) and < 1,17
(female).
The values of the ASM, HGS, and GS in elderly
male subjects from community dwelling were higher
than values obtained from subjects in nursing home
setting. While the ASM and HGS results in elderly
female subjects were quite similar between both
location, however, elderly female subjects from
community dwelling group have higher GS
compared to the elderly female subjects in the
nursing home. The percentage of the lower ASM in
elderly male and female subjects were significantly
higher in nursing home setting than community
dwelling home.
The physical performance in this study presented
by gait speed was better in elderly who lived in
community dwelling home in both gender.
ACKNOWLEDGEMENT
This study was support by Research Institution of
Trisakti University. The authors subsequently
present their sincere gratitude to the Director of Sari
Asih Hospital Ciputat Tangerang, The Head of
Budhi Mulya 2 Social Care Institution Cengkareng
for facilitating this study, and also the highest
appreciation to all of the students from the
university, the elderly subjects from the community
dwelling group and the elderly subjects from the
nursing home who participated in this study.
REFFERENCES
Moreira, V.G., Perez, M. and Lourenço, R.A. 2019.
Prevalence of sarcopenia and its associated factors: the
impact of muscle mass, gait speed, and handgrip
strength reference values on reported frequencies.
Clinics (Sao Paulo, Brazil), [online] 74, p.e477.
Available at:
https://www.ncbi.nlm.nih.gov/pubmed/30994709.
Shafiee, G., Keshtkar, A., Soltani, A., Ahadi, Z., Larijani,
B. and Heshmat, R. 2017. Prevalence of sarcopenia in
the world: a systematic review and meta- analysis of
general population studies. Journal of Diabetes &
Metabolic Disorders, [online] 16(1). Available at:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5434
551.
Rodríguez-Rejón, A.I., Ruiz-López, M.D., Wanden-
Berghe, C. and Artacho, R. 2019. Prevalence and
Diagnosis of Sarcopenia in Residential Facilities: A
Systematic Review. Advances in nutrition (Bethesda,
Md.), [online] 10(1), pp.51–58. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/30668619.
Abe, T., Sakamaki, M., Yasuda, T., Bemben, M.G.,
Kondo, M., Kawakami, Y. and Fukunaga, T. 2011.
Age-related, site-specific muscle loss in 1507 Japanese
men and women aged 20 to 95 years. Journal of sports
science & medicine, [online] 10(1), pp.145–50.
Available at:
https://www.ncbi.nlm.nih.gov/pubmed/24149307.
Milanović, Z., Pantelić, S., Trajković, N., Sporiš, G.,
Kostić, R. and James, N. 2013. Age-related decrease
in physical activity and functional fitness among
elderly men and women. Clinical interventions in
aging, [online] 8, pp.549–56. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/23723694.
Santilli, V., Bernetti, A., Mangone, M. and Paoloni, M.
2014. Clinical definition of sarcopenia. Clinical cases
in mineral and bone metabolism : the official journal
of the Italian Society of Osteoporosis, Mineral
Metabolism, and Skeletal Diseases, [online] 11(3),
pp.177–80. Available at:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4269
139/.
Lees, M.J., Wilson, O.J., Hind, K. and Ispoglou, T. 2019.
Muscle quality as a complementary prognostic tool in
conjunction with sarcopenia assessment in younger
and older individuals. European Journal of Applied
Physiology, 119(5), pp.1171–1181.
Yeung, S.S.Y., Reijnierse, E.M., Pham, V.K.,
Trappenburg, M.C., Lim, W.K., Meskers, C.G.M. and
Maier, A.B. 2019. Sarcopenia and its association with
falls and fractures in older adults: A systematic review
and meta-analysis. Journal of cachexia, sarcopenia
and muscle, [online] 10(3), pp.485–500. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/30993881.
Chumlea, W.C., Cesari, M., Evans, W.J., Ferrucci, L.,
Fielding, R.A., Pahor, M., Studenski, S., Vellas, B.
and International Working Group on Sarcopenia Task
Force Members. 2011. Sarcopenia: designing phase
IIB trials. The journal of nutrition, health & aging,
[online] 15(6), pp.450–5. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/21623466.
Chen, L.-K., Liu, L.-K., Woo, J., Assantachai, P.,
Auyeung, T.-W., Bahyah, K.S., Chou, M.-Y., Chen,
L.-Y., Hsu, P.-S., Krairit, O., Lee, J.S.W., Lee, W.-J.,
Lee, Y., Liang, C.-K., Limpawattana, P., Lin, C.-S.,
Peng, L.-N., Satake, S., Suzuki, T., Won, C.W., Wu,
C.-H., Wu, S.-N., Zhang, T., Zeng, P., Akishita, M.
and Arai, H. 2014. Sarcopenia in Asia: consensus
report of the Asian Working Group for Sarcopenia.
Journal of the American Medical Directors
Association, [online] 15(2), pp.95–101. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/24461239.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
10

Carvalho do Nascimento, P.R., Poitras, S. and Bilodeau,
M. 2018. How do we define and measure sarcopenia?
Protocol for a systematic review. Systematic reviews,
[online] 7(1), p.51. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/29587829.
Cruz-Jentoft, A.J., Baeyens, J.P., Bauer, J.M., Boirie, Y.,
Cederholm, T., Landi, F., Martin, F.C., Michel, J.-P.,
Rolland, Y., Schneider, S.M., Topinková, E.,
Vandewoude, M., Zamboni, M. and European
Working Group on Sarcopenia in Older People. 2010.
Sarcopenia: European consensus on definition and
diagnosis: Report of the European Working Group on
Sarcopenia in Older People. Age and ageing, [online]
39(4), pp.412–23. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/20392703.
Bahat, G., Tufan, A., Tufan, F., Kilic, C., Akpinar, T.S.,
Kose, M., Erten, N., Karan, M.A. and Cruz-Jentoft,
A.J. 2016. Cut-off points to identify sarcopenia
according to European Working Group on Sarcopenia
in Older People (EWGSOP) definition. Clinical
nutrition (Edinburgh, Scotland), [online] 35(6),
pp.1557–1563. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/26922142.
Depkes RI. 2016. Situasi Lanjut Usia di Indonesia.
InfoDATIN, [online] pp.1–4. Available at:
http://www.depkes.go.id/resources/download/pusdatin
/infodatin/infodatin%20lansia%202016.pdf.
Buckinx, F., Reginster, J.Y., Brunois, T., Lenaerts, C.,
Beaudart, C., Croisier, J.L., Petermans, J. and Bruyère,
O. 2017. Prevalence of sarcopenia in a population of
nursing home residents according to their frailty
status: results of the SENIOR cohort. Journal of
musculoskeletal & neuronal interactions, [online]
17(3), pp.209–217. Available at:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5601
266/.
Salvà, A., Serra-Rexach, J.A., Artaza, I., Formiga, F.,
Rojano I Luque, X., Cuesta, F., López-Soto, A.,
Masanés, F., Ruiz, D. and Cruz-Jentoft, A.J. 2016.
Prevalence of sarcopenia in Spanish nursing homes:
Comparison of the results of the ELLI study with other
populations. Revista espanola de geriatria y
gerontologia, [online] 51(5), pp.260–4. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/27068239/.
Tieland, M., Trouwborst, I. and Clark, B.C. 2017. Skeletal
muscle performance and ageing. Journal of Cachexia,
Sarcopenia and Muscle, [online] 9(1), pp.3–19.
Available at:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5803
609.
Shen, Y., Chen, J., Chen, X., Hou, L., Lin, X. and Yang,
M. 2019. Prevalence and Associated Factors of
Sarcopenia in Nursing Home Residents: A Systematic
Review and Meta-analysis. Journal of the American
Medical Directors Association, [online] 20(1), pp.5–
13. Available at:
https://www.jamda.com/article/S1525-
8610(18)30503-6/fulltext/.
The Comparison of Sarcopenia Prevalence between Elderly in Community Dwelling and Nursing Home based on Indonesian Young Adult
Cut-Off Point
11
