
The Role of Hearing in Aging and Hearing Rehabilitation Technology
with an Outlook on Future Applications
Lukas H. B. Tietz and Gabrielle H. Saunders
Eriksholm Research Centre, Rørtangvej 20, 3070 Snekkersten, Denmark
Keywords: Hearing, Hearing Loss, Ehealth, Tele-health, Hearing Aids, Rehabilitation.
Abstract: The purpose of this position paper is to raise awareness about the negative impacts of age-related hearing loss
and the importance of providing good hearing healthcare. We also provide an overview of state-of-the-art
hearing aids - the standard rehabilitative technology for hearing loss – along with some thoughts about the
future of hearing healthcare. Provision of hearing intervention is critical because untreated age-related hearing
loss is associated with numerous negative impacts on the health and well-being, such as increased odds of
falling, social isolation and cognitive decline. We suggest that, hearing technologies that combine intelligent
computer systems with user centred approaches to hearing healthcare provision will ensure that hearing aids
result in improved quality of life for those with hearing loss.
1 INTRODUCTION
Age-related hearing loss (ARHL) is one of the top 5
contributors to years lived with disability. ARHL has
broad negative psychosocial impacts and, perhaps
more alarmingly, untreated ARHL is known to be
associated to cognitive decline and dementia (GBD
2015 Disease and Injury Incidence and Prevalence
Collaborators, 2016) Gerontologists and others with
an aging clientele therefore need to be aware of
options for audiological rehabilitation of their aging
patients.
The purpose of this position is to describe the
impacts of untreated hearing loss on the individuals
and their family, to discuss the role of audiological
care, and to make the case that gerontologists need to
adjust their practice if a client has untreated hearing
loss. Additionally, this work provides an overview of
state-of-the-art hearing aids (HAs) - the standard
rehabilitative technology for hearing loss – along with
some thoughts about the future of hearing healthcare,
so that the reader knows the options available to those
with ARHL.
2 IMPACTS OF ARHL
Hearing loss is a chronic condition, the prevalence of
which is strongly associated with age.
Epidemiological studies indicate that approximately
25-50% of people have a bilateral hearing loss of 30
dB or more by age 70 years, which increases to
between 40% and 75% by age 80 years, (Roth et al.,
2011, Feder et al., 2015; Goman and Lin, 2016). The
rate of onset of hearing loss increases at faster pace
yet in those aged 80 years and older (Wattamwar et
al., 2017).
Untreated hearing loss has many negative impacts
– it limits the ability to conduct activities of daily
living (Gopinath et al., 2012) and increases the odds
of falling (Jiam et al., 2016), as well as increasing
utilization of healthcare services and hospitalization
rates (Green and Pope, 2001; Genther et al, 2013). At
a psychosocial level, hearing loss is associated with
social isolation, loneliness, and depression (Sung et
al., 2016; Mick et al., 2014; Hay-McCatcheon et al.,
2018). Further, data are rapidly accumulating that
show a robust link between hearing loss and cognitive
decline (Dawes et al., 2015; Amieva et al., 2015, Lin
et al., 2013).
The mechanisms of the above associations are not
always clear, although hearing loss as a mediator
between use of healthcare services and other
conditions has certainly been demonstrated. For
example, in a study by Crealey and O’Neill (2018),
hearing loss was found to consistently predict aspects
of cognition, autonomy, mobility and memory, which
in turn, predicted frequency of GP visits. On a
positive note, whether directly or indirectly, use of
Tietz, L. and Saunders, G.
The Role of Hearing in Aging and Hearing Rehabilitation Technology with an Outlook on Future Applications.
DOI: 10.5220/0007760603050310
In Proceedings of the 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2019), pages 305-310
ISBN: 978-989-758-368-1
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
305

hearing aids seems to moderate some of these
negative effects (Amieva et al., 2015; Crealey and
O’Neill, 2018; Hay-McCutcheon et al., 2018; Ray et
al., 2018; Weinstein et al., 2016).
Unfortunately, the use and uptake of hearing aids
among individuals with ARHL is low. Data suggest
that people wait on average 7-10 years after noticing
hearing problems before seeking help (Davis et al.,
2007), and that just 15-30% of people who would
benefit from hearing aids obtain and use them (Chien
and Lin, 2012; NIDCD, 2016). Explanations for low
help seeking and uptake of hearing healthcare include
a lack of awareness of hearing loss because of its very
gradual onset, stigma associated with hearing loss and
hearing aids, the cost of hearing aids and a lack of
access and/or knowledge of how to access services
(Wallhagen and Reed, 2018; Wallhagen, 2010;
Saunders et al., 2018).
Primary care is an important entry way to almost
all health care services. Unfortunately, screening for
ARHL in primary care is uncommon with overall
rates found to be about 23% (Abrams and Kihm,
2015). Of even greater concern are reports from older
patients that their primary care practitioners (PCPs)
do not view ARHL as a health-related issue, or as a
priority during office visits (Chou et al., 2011). More
alarmingly yet, is the finding that even when issues
related to ARHL are raised by individuals seeking
care, practitioners often negate the concern, and/or
view hearing aids as stigmatizing or ineffective
(Wallhagen, 2010). It is thus important bring
awareness of the impacts of untreated hearing loss to
practitioners who provide services to the elderly, and
to educate them as to how hearing loss can be
managed.
3 TECHNOLOGY FOR HEARING
REHABILITATION
This section describes state-of-the-art hearing aid
technology and provides some ideas about the future
of hearing healthcare which will allow for novel
functionalities and possibilities in rehabilitation,
service delivery, and research.
3.1 Current Technologies
A traditional hearing aid consists of a microphone to
pick up external sounds, an amplifier to increase the
incoming signal gain and some form of transducer to
transfer sound from the amplifier to the ear canal.
However, today’s devices incorporate many
additional features that provide signal enhancement
via digital signal processing. These features include
the following:
Multiple channels
Directional microphone systems
Noise reduction
Feedback management
Wireless connectivity
Data logging
Learning features
Binaural processing
Multiple programs
Current developments are also focussing on
increasing the processing power of the built-in
computing units, while reducing the power
consumption overall. It is important that the audio
processing happens as fast as possible to reduce the
time delay between the picked-up signal at the
microphones and the transmitted signal at the
speaker.
3.1.1 Multiple Channels
A channel is essentially a filter that breaks out a broad
band signal into discrete bands of frequencies.
Signals within a frequency band or channel are
analysed and processed independently from signals in
other bands. Parameters that are typically analysed
and processed within a band are gain (for overall
amplification, feedback and output control), noise
reduction processing and directional microphone
polar patterns. Broadly, the advantage of multiple
channels is customization of the hearing aid output to
a specific configuration of hearing loss.
3.1.2 Directional Microphone Systems
Almost all of today’s hearing aids are equipped with
multiple microphones, that enable incoming signals
to be differentially amplified depending on their
source relative to the microphone ports. Directional
microphones aim to provide greater amplification for
signals arriving from the front than for signals
arriving from the left, right or behind, thus improving
the signal-to-noise ratio of signal from the front that
are delivered to the ear of the hearing aid user. Most
hearing aids today automatically adjust the
directionality of the microphones in response to the
environmental input. This is generally beneficial for
the user, but it has its limitations if the hearing aid
software misclassifies an incoming signal or if the
user wants to listen to a sound source that is not
located in front of them.
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
306
3.1.3 Noise Reduction
The most common complaint of hearing aid users is
difficulty hearing in a noisy environment. Noise
reduction algorithms were thus implemented into
hearing aids to decrease the annoyance caused by
noise, and to improve speech understanding. Noise
reduction algorithms have generally been shown to be
effective at the former, but not the latter (Brons et al.,
2015). Digital noise reduction algorithms vary greatly
across hearing aids and new signal processing
approaches are continually being developed.
Wind noise, caused by the vibration of the
microphone membranes due to wind turbulence
around the microphone inlets is another problem for
hearing aid user, so noise reduction algorithms
targeting wind noise have been developed with some
success.
3.1.4 Feedback Management
Acoustic feedback occurs when the sound that has
been amplified by the hearing aid re-enters the
microphone and is amplified again, causing a high
pitch whistle or ringing. Feedback can be a problem
in hearing aids because the receiver and microphone
are physically close together and thus acoustic
leakage can easily occur. Leakage can also occur
when the speaker is not properly inserted into the ear.
Signal processing algorithms to combat feedback
have been successfully developed. Typically, these
systems work by limiting the output from a hearing
aid channel when feedback is detected in that channel
or in newer hearing aids, by introducing an oscillating
signal that cancels out the feedback signal
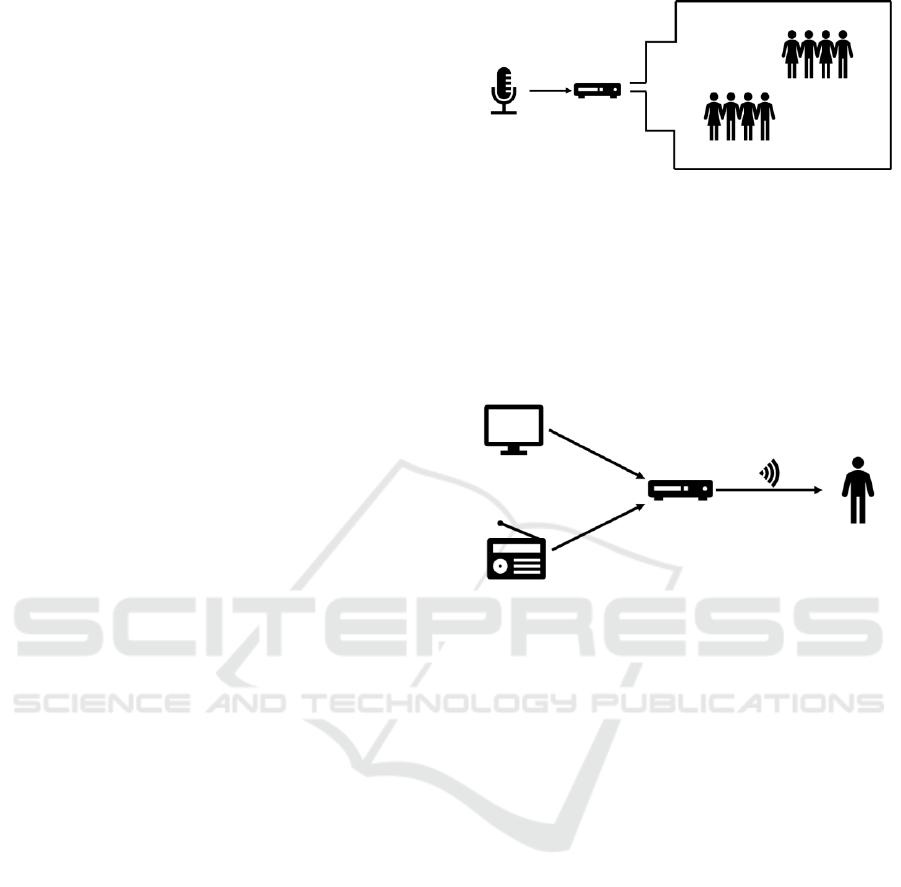
3.1.5 Wireless Connectivity
Telecoil systems allow the hearing aid to pick up
signals from compatible electromagnetically looped
systems. These systems are typically found in
auditoriums, churches or larger meeting rooms where
external microphones are utilised by a speaker. The
telecoil system transmits the recorded voice signal via
an induction loop directly to the hearing aid. The
principle is shown in figure 1.
The signal then is processed by the digital sound
processor and fed to the speakers of the HA. This way
the microphones of the HA are bypassed, which
increases the signal-to-noise ratio and should enhance
speech understanding. This system allows a large
group of hearing aid users to receive the same signal.
A different wireless solution is a FM based system,
where an external audio signal is picked up by an
amplifier and transmitter device – called streamer –
Figure 1: A telecoil system consists of an external
microphone, an amplifier and an induction coil that is
placed in the room around the HA users.
and then transmitted via radio frequency to an
antenna in the HA. Thereby the signal is bypassing
the integrated microphone and is processed directly
by the sound processor. The principle for streamer
functionality can be seen in figure 2.
Figure 2: The FM system consists of an external signal
source like TV or radio and an amplifier and transmission
device that directly couples to the patients HAs.
The difference to the telecoil system is that here
the signal is transmitted to one single pair of hearing
aids. This connectivity method can also be used to
utilize a portable external microphone that can be
handed to a conversation partner.
Bluetooth connectivity gains more popularity
these days as it allows for direct connection with
smartphones and other certified Bluetooth audio
devices. Sound can be streamed directly to the
processor of the hearing aid. This functionality also
allows the patient to handle steering inputs for the
HAs, like adjusting the volume or program. This
technology enables two-way data communication,
which is important for some of the future
technologies, that will be described further on. Newer
Bluetooth standards are allowing for less energy
consumption, while the connection is active.
3.1.6 Datalogging
The internal digital memory space on the hearing aids
is used for data logging. When visiting the
audiologist, the data log can give insights into the
usage pattern of the devices. The internal memory can
include data on the total usage of the device, daily
The Role of Hearing in Aging and Hearing Rehabilitation Technology with an Outlook on Future Applications
307

average, average of sound pressure levels, classified
environments or program usage. The environment
classification usually differentiates between: quiet,
speech, speech in noise and noise.
3.1.7 Learning Features
Some hearing aids now offer a learning functionality,
a logic software saves the user interactions on the
hearing aid in correlation with other logged data.
Over time this can lead to less need to interact with
the HA, as the devices could automatically adjust
volume or program when detecting a known
environment. This feature is very new and holds a lot
of potential for the future, especially to increase
device usability.
3.1.8 Binaural Processing
With binaural processing capabilities, a pair of
hearing aids is communicating wirelessly with each
other. This feature is used to make program or volume
changes on both hearing aids by just using the button
on one of them. In recent years, the protocol also
allows for sound source location detection, meaning
the side from which the sound is represented can be
detected and amplified accordingly, also allowing for
a better directional effect.
3.1.9 Multiple Programs
Hearing aids provide the possibility for the
audiologist to create different programs, that suit
different auditory environments and personal
preferences. Optimised settings e.g. a high level of
directionality and high level of noise reduction can be
saved as settings in a ‘conversation program’. The
different programs can be accessed by the patient
easily and quickly on the hearing aids or through the
connected smartphone application, to suit the
patients' needs in different environments.
3.2 Future Technologies
With the implementation of smart connectivity new
opportunities present themselves as hearing aids are
now opening to be used as Internet-of-Things
activated devices. Remote monitoring as well as
changes to the personalization of the devices have
been introduced very recently. Self-monitoring
features have also gained increasing recognition.
Over-the-air firmware updates for hearing aids start
to be available from this point forward (Hoppe and
Hesse, 2017). Thanks to the low energy and high
bandwidth wireless connection, more complex signal
processing could be handled by a smartphone, as that
offers more processing power. Rechargeable batteries
have recently been introduced but they have yet to be
implemented widely in more HA models.
Applications that include data transfer could
incorporate artificial intelligence – supported
optimisations. Continuous monitoring of HA usage
via data collection in a cloud service enable usage
pattern recognition and, through machine learning,
better automated setting prediction of the device for
certain situations (Zhang et al., 2016). These could
enhance the user experience through an ‘always right’
option based on the learned preferences of the user in
certain situations.
Research in auditory fields is also transformed
through the availability of remote data collection. The
EU-project ‘EVOTION’ is utilizing the collection of
different variables from the hearing aids as well as
smartphones, health sensors and clinical repositories.
These data should then be used to find possible
success factors for hearing loss treatment and support
the formulation of hearing healthcare policies based
on real world evidence (Dritsakis et al., 2018). This
concept of evidence collection through connected
devices could also be applied to other fields of policy
making.
Additional, to the objective data collection, new
possibilities for subjective feedback would improve
the labelling of data. Giving the user the possibility to
report on the quality and functionality of hearing aids
in a current situation would provide personal labels,
which in turn could be used at later points to intervene
in challenging situations. These personal labels and
notes can also be used for improved counselling.
4 CONCLUSIONS
In conclusion, ARHL has numerous negative impacts
on life, thus limiting the ability to conduct activities
of daily living. Furthermore, increased odds of
falling, social isolation as well as a strong connection
with cognitive decline are significant indicators that
an ARHL should be treated. A hearing loss, that is
recognised and treated, is battling these and other
negative impacts. Hearing health as a part of general
health is an important factor for aging well and should
be recognized by the science of gerontology and
research into this area is worthwhile as well as
important.
Hearing aids are the standard rehabilitative
technology for hearing loss and modern HAs offer a
large number of features that should help increase
speech intelligibility and usability. Wireless
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
308

connectivity and software enhancements have a great
impact on the usability and versatility of the devices
and can lead to better rehabilitation in the future. In
combination with artificial intelligence, data
collection and powerful computer systems as well as
user centred approaches, the rehabilitation with these
devices can have a positive impact on the quality of
life of those living with ARHL.
REFERENCES
Abrams H.B. and Kihm J. An introduction to MarkeTrak
IX: A new baseline for the hearing aid market. Hearing
Review. 2015;22(6):16.
Amieva H., Ouvrard C., Giulioli C., Meillon C., Rullier L.
and Dartigues J.F. (2015). Self-Reported Hearing Loss,
Hearing Aids, and Cognitive Decline in Elderly Adults:
A 25-Year Study. J Am Geriatr Soc., 10):2099-2104
Brons I., Houben R. and Dreschler W.A. (2015) Acoustical
and perceptual comparison of noise reduction and
compression in hearing aids. Journal of Speech,
Language, and Hearing Research 58: 1363–1376.
Chou R., Dana T., Bougatsos C., Fleming C. and Beil T.
Screening adults aged 50 years or older for hearing loss:
a review of the evidence for the U.S. preventive
services task force. Ann Intern Med. 2011;154(5):347-
355.
Chien, W., and Lin, F.R. (2012). Prevalence of hearing aid
use among older adults in the United States. Archives
of Internal Medicine, 172(3), 292–293.
https://doi.org/10.1001/archinternmed.2011.1408
Crealey G.E. and O'Neill C. (2018). Hearing loss, mental
well-being and healthcare use: results from the Health
Survey for England (HSE). J Public Health (Oxf), Nov
27
Dawes P., Emsley R., Cruickshanks K.J., Moore D.R.,
Fortnum H., Edmondson-Jones M., McCormack A. and
Munro K.J. (2015). Hearing loss and cognition: the role
of hearing AIDS, social isolation and depression. PLoS
One, 10(3):e0119616.
Davis, A., Smith, P., Ferguson, M., Stephens, D. and
Gianopoulos, I. (2007). Acceptability, benefit and costs
of early screening for hearing disability: a study of
potential screening tests and models. Health
Technology Assessment, 11(42).
https://doi.org/10.3310/hta11420
Dritsakis, G., Kikidis, D., Koloutsou, N., Murdin, L., Bibas,
A., Ploumidou, K., Laplante-Lévesque, A.,
Pontoppidan, N.H. and Bamiou, D. (2018). Clinical
validation of a public health policy-making platform for
hearing loss (EVOTION): protocol for a big data study,
1–9. https://doi.org/10.1136/bmjopen-2017-020978
GBD 2015 Disease and Injury Incidence and Prevalence
Collaborators. (2016). Global, regional, and national
incidence, prevalence, and years lived with disability
for 310 diseases and injuries, 1990-2015: a systematic
analysis for the Global Burden of Disease Study 2015.
Lancet (London, England), 388(10053), 1545–1602.
https://doi.org/10.1016/S0140-6736(16)31678-6
Genther, D.J., Frick, K.D., Chen, D., Betz, J., and Lin, F.R.
(2013). Association of hearing loss with hospitalization
and burden of disease in older adults. JAMA - Journal
of the American Medical Association. American
Medical Association.
https://doi.org/10.1001/jama.2013.5912
Goman, A.M., and Lin, F.R. (2016). Prevalence of Hearing
Loss by Severity in the United States. Am J Public
Health, 27(4), 1812–1818.
https://doi.org/10.1353/hpu.2016.0164
Gopinath B., Schneider J., McMahon C.M., Teber E.,
Leeder S.R. and Mitchell P. (2012). Severity of age-
related hearing loss is associated with impaired
activities of daily living. Age Ageing. 2012
Mar;41(2):195-200.
Green, C. A., and Pope, C. R. (2001). Effects of Hearing
Impairment on Use of Health Services Among the
Elderly. Journal of Aging and Health, 13(3), 315–328.
https://doi.org/10.1177/089826430101300301
Hay-McCutcheon M.J., Reed P.E. and Cheimariou S.
(2018). Positive Social Interaction and Hearing Loss in
Older Adults Living in Rural and Urban Communities.
J Speech Lang Hear Res. 61(8):2138-2145
Hoppe, U. and Hesse, G. (2017). Hearing aids: indications
, technology , adaptation , and quality control. GMS
Current Topics in Otorhinolaryngology - Head and
Neck Surgery, 16, 1–24.
Jiam N.T., Li C. and Agrawal Y. (2016). Hearing loss and
falls: A systematic review and meta-analysis.
Laryngoscope. 2016 Nov;126(11):2587-2596.
Lin F.R., Yaffe K., Xia J., Xue Q.L., Harris T.B., Purchase-
Helzner E., Satterfield S., Ayonayon H.N., Ferrucci L.
and Simonsick E.M.; Health ABC Study Group. (2013).
Hearing loss and cognitive decline in older adults.
JAMA Intern Med. 173(4):293-9
Mick P., Kawachi I. and Lin F.R. (2014). Otolaryngol Head
Neck Surg. The association between hearing loss and
social isolation in older adults. 150(3):378-84
Mroz, M. (2018). Hearing aid technology. Retrieved from
https://www.healthyhearing.com/help/hearing-
aids/technology
NIDCD (2016) Quick Statistics About Hearing. Accessed
from
https://www.nidcd.nih.gov/health/statistics/quick-
statistics-hearing#9
Ray J., Popli G. and Fell G. (2018). Association of
Cognition and Age-Related Hearing Impairment in the
English Longitudinal Study of Ageing. JAMA
Otolaryngol Head Neck Surg. 144(10):876-882.
Roth T.N., Hanebuth D. and Probst R. (2011). Prevalence
of age-related hearing loss in Europe: a review. Eur
Arch Otorhinolaryngol. 268(8):1101-1107.
Saunders G.H., Frederick M.T., Silverman S.C., Penman
T., Gardner A., Chisolm T.H., Escabi C.D., Oree P.H.,
Westermann L.C., Sanchez V.A. and Arnold M.L.
(2018). Hearing Screening in the Community. J Am
Acad Audiol. Jan 25 [Epub ahead of print].
The Role of Hearing in Aging and Hearing Rehabilitation Technology with an Outlook on Future Applications
309

Sung Y.K., Li L., Blake C., Betz J. and Lin F.R. (2016).
Association of Hearing Loss and Loneliness in Older
Adults. J Aging Health, 28(6):979-94
Wallhagen M.I. (2010). The stigma of hearing loss.
Gerontologist. 50(1):66-75
Wallhagen M.I. and Reed NS. (2018). Implications of
Hearing Care Policy for Nurses. J Gerontol Nurs.
44(9):9-14.
Wattamwar K., Qian Z.J., Otter J., Leskowitz M.J., Caruana
F.F., Siedlecki B., Spitzer J.B. and Lalwani A.K.
(2017). Increases in the Rate of Age-Related Hearing
Loss in the Older Old. JAMA Otolaryngol Head Neck
Surg. 2017 Jan 1;143(1):41-45.
Weinstein B.E., Sirow L.W. and Moser S. (2016). Relating
Hearing Aid Use to Social and Emotional Loneliness in
Older Adults. Am J Audiol., 25(1):54-61
Zhang, T., Mustiere, F., and Micheyl, C. (2016). Intelligent
Hearing Aids : The Next Revolution. 2016 38th Annual
International Conference of the IEEE Engineering in
Medicine and Biology Society (EMBC), 72–76.
https://doi.org/10.1109/EMBC.2016.7590643
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
310
