
e-Health Solutions for Aging in Place with Cognitive Impairment:
Preliminary Results of a Systematic Review
Samantha Dequanter
1 a
, Marie-Pierre Gagnon
2,3 b
, Mame-Awa Ndiaye
2
, Jessica Dion
2
,
Ellen Gorus
4
, Anne Bourbonnais
5 c
, Anik Giguère
2,6
, Samira Abbasgholizadeh Rahimi
2
,
Maaike Fobelets
1 d
and Ronald Buyl
1 e
1
Faculty of Medicine and Pharmacy, Department of Public Health Sciences, Vrije Universiteit Brussel, Belgium
2
Institute of Health and Social Services in Primary Care,
Research Center on Healthcare and Services in Primary Care of Laval University (CERSSPL-UL), Québec, Canada
3
Faculty of Nursing Sciences, Université Laval, Québec, Canada
4
Faculty of Medicine and Pharmacy, Department of Gerontology, Vrije Universiteit Brussel, Belgium
5
Faculty of Nursing Sciences, Université de Montréal, Montréal, Canada
6
Faculty of Medicine, Université Laval, Québec, Canada
mame-awa.ndiaye.ciussscn@ssss.gouv.qc.ca, jessica_dion267@hotmail.com, anne.bourbonnais@umontreal.ca,
anik.giguere@fmed.ulaval.ca, samira.abbasgholizadeh-rahimi.1@ulaval.ca
Keywords: e-Health, Information and Communication Technology, Gerontechnology, Aging, Cognitive Impairment,
Dementia, Caregivers, Systematic Review.
Abstract: Worldwide, the proportion of older adults (60+) is growing very fast, increasing the prevalence of cognitive
disorders such as Mild Cognitive Impairment and dementia. Recent literature shows a clear preference of
older adults towards Aging in Place (AIP). In order to realize AIP in cognitively impaired older adults,
appropriate measurements regarding safety and practical feasibility need to be taken. In answer to this issue,
various e-Health solutions have been developed in the last decade, targeting support of memory, social contact,
daily activities and personal safety. Much attention has also been given to solutions for caregivers of
cognitively impaired older adults. Since the field of e-Health research is expanding at fast pace, implementing
effective e-Health solutions based on research evidence constitutes a challenge. Therefore, this systematic
review aims to review recent study findings in the field of e-Health research regarding community-dwelling
cognitively impaired older adults and their informal caregivers. We also consider potential adverse effects of
adoption of these solutions. An initial search led to 12999 potentially relevant citations. First-level title-
screening of citations was completed in January 2019. Third-level full-text screening is targeted for April
2019. If possible, effect sizes for each type of e-Health intervention will be calculated.
1 INTRODUCTION
The worldwide proportion of individuals aged 60 and
above is growing faster than ever (World Health
Organization [WHO], 2018). Even the oldest-old (85+
years) are substantially growing in number in Europe
and in the U.S. and this evolution is projected to
continue for several more decades (Eurostat, 2018;
Vincent and Velkoff, 2010). Advanced age is a well-
a
https://orcid.org/0000-0001-7566-3093
b
https://orcid.org/0000-0002-0782-5457
c
https://orcid.org/0000-0002-6823-4044
d
https://orcid.org/0000-0002-8316-6422
e
https://orcid.org/0000-0002-6598-9505
known risk factor for cognitive disorders such as Mild
Cognitive Impairment and dementia (Alzheimer’s
Association, 2016; Artero et al., 2008). In turn, these
conditions, along with the functional decline and
increased dependency they entail, result in a four- to
six-fold risk of admission in a nursing home as
compared to cognitively healthy older adults
(Banaszak-Holl et al., 2004; Gnjidic et al., 2012;
Löfqvist et al., 2013). However, older adults usually
tend to have a reluctant and avoiding attitude towards
Dequanter, S., Gagnon, M., Ndiaye, M., Dion, J., Gorus, E., Bourbonnais, A., Giguère, A., Rahimi, S., Fobelets, M. and Buyl, R.
e-Health Solutions for Aging in Place with Cognitive Impairment: Preliminary Results of a Systematic Review.
DOI: 10.5220/0007746402670273
In Proceedings of the 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2019), pages 267-273
ISBN: 978-989-758-368-1
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
267

relocation. Attachment to the home and the
neighbourhood, as well as the fear of losing autonomy
appear to be important explaining factors (Ahn et al.,
2019; Löfqvist et al., 2013). This hesitation and
aversion is not completely indefensible, since recent
findings point out negative effects associated with
relocation of older adults with dementia. High
emotional distress and decline in overall well-being
appear to be the most prominent (Ryman et al., 2018).
With these arguments in mind, the preference for
aging at home seems justifiable. This phenomenon is
referred to as Aging In Place (AIP) (Centers for
Disease Control and Prevention, 2009). It is defined as
the possibility “to continue living in one’s own home
and community in a safe, independent and
comfortable way, regardless of age or ability level”.
Although it is clear that AIP is desirable for many
reasons, its implementation in practice can be
challenging. This is particularly the case for older
adults living with cognitive impairments, as the
functional limitations they face may gradually lead to
loss of independence in major life domains (Lau et al.,
2015). In addition to engagement in daytime activities,
memory support and social company are also
important need areas (van der Roest et al., 2009).
Furthermore, the caregiver burden is also important,
as symptoms of distress and depression in caregivers
are common and interact negatively with the ability of
the care-receiver to age in place (Afram et al., 2014).
To address these needs and support AIP, many
innovative approaches have been developed.
Amongst them are those emerging from the research
field of e-Health. The latter is an overarching term
covering the various uses of Information and
Communication Technology (ICT) in the sphere of
health care and health promotion (WHO, 2019).
Development of e-Health solutions for cognitively
impaired older adults has particularly been focused on
the support of memory, social contact, daily activities
and safety (Kim et al., 2017).
The solutions that compensate for impaired
memory and planning abilities consist of electronic
memory aids, voice prompting devices and cognitive
training programs delivered through mobile
applications or online websites. These solutions are
reported to enhance quality of life through increasing
task performance and overall independence
(Blackman et al., 2016; Kim et al., 2017; Meiland et
al., 2017; Tyack and Camic, 2017).
Various e-Health solutions also have the ability to
support social engagement, mood and well-being of
older adults with cognitive impairment (Lorenz et al.,
2017; Meiland et al., 2017; Tyack and Camic, 2017).
Firstly, simplified pre-programmed video or
telephone solutions aim to keep these older adults
connected to their social network (Lauriks et al.,
2007). Secondly, social competence training is made
possible through the use of simulated virtual social
environments (Tyack and Camic, 2017). These
environments are often integrated in virtual games,
e.g. in which players are guided through the process
of going shopping. With regard to facilitating
communication and overall social interaction with
caregivers, social robot therapy could potentially be
of benefit, as well as using digital multimedia for art
and music expression and for facilitating reminiscing
(Lauriks et al., 2007; Lorenz et al., 2017; Meiland et
al., 2017; Tyack and Camic, 2017).
With regard to support of activities of daily living
(ADL) and safety of cognitively impaired older
adults, smart home technology is increasingly gaining
attention. This type of e-Health technology is part of
the Ambient Assisted Living (AAL) technology and
refers to the networked connection of the home with
the world beyond, in which sensors play an important
role and can be monitored remotely (Balta-Ozkan et
al., 2013; Blackman et al., 2016). The benefits of this
technology lie in the unobtrusive automatic
registration of activity and behaviour of residents,
which enables continuous monitoring as well as
disease management (Marikyan et al., 2019). These
systems have the ability to automatically generate
alarm responses in predetermined conditions. This
can be of importance for detection of potentially
major safety incidents, e.g. flooding or a house fire,
as well as detection of changes in ADL routines,
indicating potential cognitive deterioration
(Blackman et al., 2016). Regarding safety concerns,
the passive detection of wandering of older adults
with dementia is also possible through use of sensors
in door posts or fences, or by means of geotracking
through Global Positioning System (GPS)-enabled
systems that are integrated in wearables or mobile
telephones (Blackman et al., 2016; Kim et al., 2017;
Meiland et al., 2017). Moreover, localization
applications have the potential to support autonomous
spatial orientation, and thus, to support the
independence of these individuals (Kim et al., 2017).
Literature also identified positive effects of e-
Health solutions for caregivers of cognitively
impaired older adults. Mobile applications, online
websites and video conferences delivering education
and stress management training are only a few
examples (Kim et al., 2017). Positive effects of these
interventions on caregiver self-efficacy, anxiety and
depression levels, and disease knowledge have been
observed (Parra-Vidales et al., 2017). Moreover,
solutions concerning art viewing or music playing that
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
268

target the caregiver and care-receiver dyad are
reported to result in lower perceived burden, better
communication and higher quality of the dyadic
relationship (Tyack and Camic, 2017). Furthermore,
e-Health interventions that directly target the
psychological needs of caregivers also show
promising results. In a recent study, technology-based
equivalents of Cognitive Behavioural Therapy (CBT)
showed positive effects on caregiver depression that
were comparable to the face-to-face intervention
(Scott et al., 2015).
In conclusion, many different e-Health
technologies for cognitively impaired older adults
and caregivers have been developed and studied.
Most studies demonstrated substantial benefits for
both parties in this dyad. However, these study
findings should be interpreted with caution since
many of the studies have poor methodological quality
as reflected in small sample sizes, uncontrolled study
designs and inadequate outcome measures (Meiland
et al., 2017). Moreover, the tenability of the reported
findings is debatable. Everyday new innovative
technologies are developed, which render study
findings outdated at a fast pace. Therefore we believe
that there is a need to revisit the literature and to cover
the current state of play in the field of e-Health
solutions for AIP with cognitive impairment.
2 OBJECTIVES
This systematic review aims to identify empirically
validated e-Health solutions for community-dwelling
seniors living with cognitive impairment and their
informal caregivers. Moreover, we will analyse and
evaluate the effectiveness of these solutions in terms
of relevant health and well-being outcomes. Potential
adverse effects related to adoption of these solutions
will also be considered.
3 METHODS
3.1 Search Strategy
We conducted a literature review of six electronic
databases including PubMed, CINAHL, the
Cochrane Library, PsycINFO, Web of Science,
Embase and Sociological Abstracts. The search
strategy incorporated search terms that were related
to target populations or types of interventions. The
strategy that was entered in PubMed is listed in Table
1. Adaptations to this search strategy were made in
order to guarantee compatibility with the entry
formats of the different other databases. A publication
date filter was used to exclude articles published
before 2013, thereby minimizing irrelevant or
outdated references.
3.2 Study Selection
The study selection process started in October 2018
after importing the titles and abstracts of the citations
using the Rayyan software (Ouzzani et al., 2016). The
final selection of articles comprised publications from
January 2013 until the date of search, which is October
2018. The selection process follows a multi-level
method in which title, abstract and full-text of articles
are consecutively screened (Mateen et al., 2013).
First-level screening of title was independently
conducted by four researchers working in pairs by
January 2019. One pair of reviewers screened
reference titles published from 2013 until 2015 (SD
and MAN) and one pair of reviewers screened
reference titles published from 2016 until 2018 (MPG
and JD). Screening conflicts will be resolved through
discussion, or if necessary with the help of a third
reviewer (RB). After title-screening conflict
resolution, second- and third-level screening will be
executed in February 2019 and April 2019
respectively.
To be considered for inclusion, references have to
adhere to a set of inclusion criteria. Firstly, studies
should contain at least one e-Health solution situated
in the field of telehealth, telemedicine and telecare,
ambient/active assisted living (AAL) or (robotic)
assistive technology. Additionally, these e-Health
solutions need to be developed for or tested with
informal caregivers of community-dwelling
cognitively impaired older adults, or with the latter
themselves. Articles that do not comply with this
criterion but that contain an e-Health solution that is
recognized as being memory supportive or of benefit
for one of the described target groups, will be
considered for inclusion. Older people are defined as
having the chronological age of 65 years or more.
Informal caregivers have to be 18 years or older. The
community-dwelling characterization is
operationalized by the condition of living at home or
in an independent living facility. Studies that
exclusively describe e-Health solutions for
institutional settings such as nursing homes will be
excluded. Furthermore, articles need to be written in
English, French, Dutch or Spanish to be included. All
study designs, interventional and non-interventional,
are considered for inclusion, though editorials,
comments, letters to the editor and technical notes
e-Health Solutions for Aging in Place with Cognitive Impairment: Preliminary Results of a Systematic Review
269
will be excluded. Articles reviewing e-Health
solutions and measuring their effectiveness will be
excluded from analysis, but will be reviewed for
additional references (snowballing).
Articles meeting the inclusion criteria will be
assessed by two independent reviewers (SD and
MAN) for methodological quality using the Cochrane
Risk of Bias tool (Higgins and Green, 2011) in case
of an intervention study, or checklists F, G and H
provided by the National Institute of Health and Care
Excellence for other study designs (NICE). Any
disagreements that arise between the reviewers will
be resolved through discussion, or with the help of a
third reviewer.
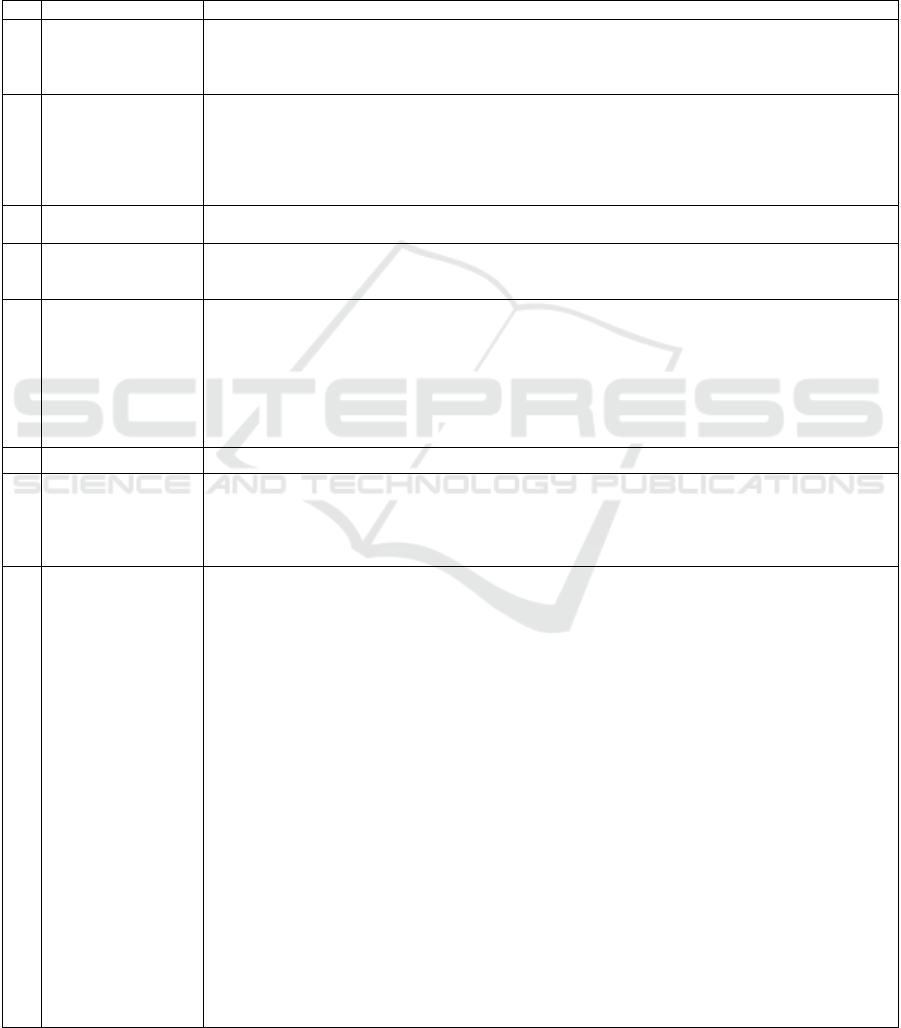
Table 1: Search strategy as used in PubMed.
No.
Concepts
Concept equations
1
Dementia or Cognitive
Impairment
(Controlled
vocabulary)
"Dementia"[Mesh] OR "Alzheimer Disease"[Mesh] OR "Neurodegenerative Diseases"[Mesh] OR
"Cognitive Dysfunction"[Mesh] OR "Frontotemporal Dementia"[Mesh] OR "Huntington Disease"[Mesh]
OR "Parkinsonian Disorders"[Mesh] OR "Prion Diseases"[Mesh]
2
Dementia or Cognitive
Impairment (Free text)
alzheimer*[Title/Abstract] OR dementi*[Title/Abstract] OR cognitive impairment*[Title/Abstract] OR
neurocognitive disorder*[Title/Abstract] OR neurodegenerative[Title/Abstract] OR cognitive
dysfunction*[Title/Abstract] OR cognitive decline*[Title/Abstract] OR frontotemporal
degeneration*[Title/Abstract] OR huntington’s disease*[Title/Abstract] OR huntington
disease*[Title/Abstract] OR lewy body disease*[Title/Abstract] OR Parkinson*[Title/Abstract] OR prion
disease*[Title/Abstract] OR senility[Title/Abstract]
3
Dementia or Cognitive
Impairment
#1 OR #2
4
e-Health Technology
(Controlled
vocabulary)
"Telemedicine"[Mesh] OR "Remote Consultation"[Mesh] OR "Telepathology"[Mesh] OR
"Telerehabilitation"[Mesh] OR "Telenursing"[Mesh]
5
e-Health Technology
(Free text)
econsult*[tiab] OR e-consult*[tiab] OR ediagnos*[tiab] OR e diagnos*[tiab] OR mobile health*[tiab] OR
mhealth*[tiab] OR m health*[tiab] OR telehealth*[tiab] OR tele health[tiab] OR remote consult*[tiab] OR
"remote patient monitoring"[tiab] OR teleconsult*[tiab] OR tele consult*[tiab] OR telenursing[tiab] OR tele
nursing[tiab] OR telediagnos*[tiab] OR tele diagnos*[tiab] OR telemedic*[tiab] OR tele medic*[tiab] OR
telemonitor*[tiab] OR tele monitor*[tiab] OR ehealth*[tiab] OR e health*[tiab] OR telecare[tiab] OR tele
care[tiab] OR digital health[tiab] OR telecounsel*[tiab] OR tele counsel*[tiab] OR remote counsel*[tiab]
OR distance consult*[tiab] OR distance counsel*[tiab] OR distant consult*[tiab] OR telehomecare*[tiab]
OR telepatholog*[tiab] OR health technolog*[tiab] OR medical technolog*[tiab]
6
e-Health Interventions
#4 OR #5
7
Technology
(Controlled
vocabulary)
"Electronic Mail"[Mesh] OR "Telefacsimile"[Mesh] OR "Modems"[Mesh] OR
"Videoconferencing"[Mesh] OR "Computer Communication Networks"[Mesh] OR "Internet"[Mesh] OR
"User-Computer Interface"[Mesh] OR "Multimedia"[Mesh] OR "Cell Phone"[Mesh] OR "Computers,
Handheld"[Mesh] OR "Mobile Applications"[Mesh] OR "Minicomputers"[Mesh] OR
"Microcomputers"[Mesh]
8
Technology (Free text)
telefacsimile*[Title/Abstract] OR cell phone*[Title/Abstract] OR video-conferen*[Title/Abstract] OR
videoconference*[Title/Abstract] OR videophone*[Title/Abstract] OR video-phone*[Title/Abstract] OR
computer*[Title/Abstract] OR Internet[Title/Abstract] OR iphone*[Title/Abstract] OR
smartphone*[Title/Abstract] OR information technolog*[Title/Abstract] OR communication
technolog*[Title/Abstract] OR mobile technolog*[Title/Abstract] OR mobile application*[Title/Abstract]
OR phone application*[Title/Abstract] OR tablet*[Title/Abstract] OR mobile phone*[Title/Abstract] OR
healthcare robotics[Title/Abstract] OR assistive technology[Title/Abstract] OR
gerontechnology[Title/Abstract] OR gerontotechnology[Title/Abstract] OR intelligent
system*[Title/Abstract] OR networked technolog*[Title/Abstract] OR virtual reality[Title/Abstract] OR
(("app"[Title/Abstract]) NOT ("amyloid precursor protein"[Title/Abstract])) OR "apps"[Title/Abstract] OR
world wide web*[Title/Abstract] OR webportal*[Title/Abstract] OR web portal*[Title/Abstract] OR
ipad[Title/Abstract] OR ipads[Title/Abstract] OR text messag*[Title/Abstract] OR "ussd"[Title/Abstract]
OR laptop*[Title/Abstract] OR palmtop*[Title/Abstract] OR palm top*[Title/Abstract] OR interactive
voice response*[Title/Abstract] OR multimedia[Title/Abstract] OR android[Title/Abstract] OR
digital[Title/Abstract] OR online[Title/Abstract] OR on-line[Title/Abstract] OR texting[Title/Abstract] OR
minicomputer*[Title/Abstract] OR microcomputer*[Title/Abstract] OR mobile device*[Title/Abstract] OR
ambient assisted living[Title/Abstract] OR active assisted living[Title/Abstract] OR e-
learning[Title/Abstract] OR elearning[Title/Abstract] OR wayfinding[Title/Abstract] OR
geotracking*[Title/Abstract] OR geo-tracking*[Title/Abstract] OR global positioning
system*[Title/Abstract] OR GPS track*[Title/Abstract] OR GPS device*[Title/Abstract] OR GPS
technolog*[Title/Abstract] OR GPS navigation*[Title/Abstract] OR GPS logging device*[Title/Abstract]
OR electronic mail*[Title/Abstract] OR cellular phone*[Title/Abstract] OR geographic information
system*[Title/Abstract] OR telecommunication*[Title/Abstract] OR e-mail[Title/Abstract] OR
fax[Title/Abstract] OR "self-help device*"[Title/Abstract] OR "patient portal*"[Title/Abstract] OR
modem*[Title/Abstract]
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
270
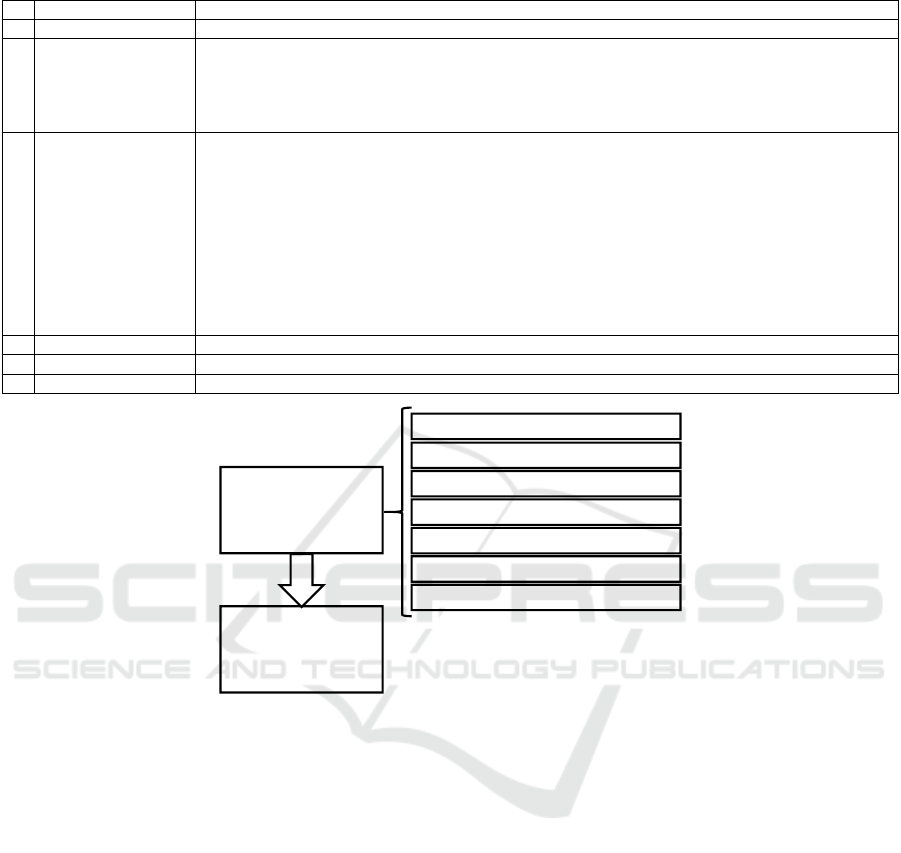
Table 1: Search strategy as used in PubMed(cont.).
9
Technology
#7 OR #8
10
e-Health Technology
#6 OR #9
11
Intervention
(Controlled
vocabulary)
"Remote Consultation"[Mesh] OR "Counseling"[Mesh] OR "Social Support"[Mesh] OR "Self
Medication"[Mesh] OR "Self Care"[Mesh] OR "Self-Management"[Mesh] OR "Consumer Health
Information"[Mesh] OR "therapy" [Subheading] OR "Education"[Mesh] OR "education" [Subheading] OR
"Education, Distance"[Mesh] OR "Patient Education as Topic"[Mesh] OR "Pain Management"[Mesh] OR
"Self-Help Groups"[Mesh] OR "Home Care Services"[Mesh]
12
Intervention (Free text)
consult*[Title/Abstract] OR couns*[Title/Abstract] OR "follow up"[Title/Abstract] OR "follow
ups"[Title/Abstract] OR support*[Title/Abstract] OR healthcare*[Title/Abstract] OR "care"[Title/Abstract]
OR "cares"[Title/Abstract] OR self-medicat* [Title/Abstract] OR selfcar*[Title/Abstract] OR
selfmanagement [Title/Abstract] OR selfhelp [Title/Abstract] OR selfadminist*[Title/Abstract] OR
selfmonitor*[Title/Abstract] OR selfmedicat*[Title/Abstract] OR caregiving[Title/Abstract] OR
psychoeducation [Title/Abstract] OR information[Title/Abstract] OR advis*[Title/Abstract] OR
advice[Title/Abstract] OR intervention*[Title/Abstract] OR therap*[Title/Abstract] OR
program*[Title/Abstract] OR train*[Title/Abstract] OR educat*[Title/Abstract] OR manag*[Title/Abstract]
OR help[Title/Abstract] OR assist*[Title/Abstract] OR monitor*[Title/Abstract] OR
administ*[Title/Abstract] OR strategy[Title/Abstract] OR strategies[Title/Abstract]OR
project[Title/Abstract] OR projects[Title/Abstract] OR procedure*[Title/Abstract]
13
Intervention
#11 OR #12
14
Total Result
#3 AND #10 AND #13
Publication Date Filter
2013-2018
Figure 1: PRISMA flow diagram for the selection of studies.
3.3 Data Extraction and Synthesis
Articles that meet the selection criteria are compiled
into a predesigned Excel data spreadsheet detailing
primary study characteristics (authors, year, country
of origin, study design, study population, sample
size), the identified e-Health solution(s), the used data
collection methods and the outcomes of significance
for the review question. The extraction of these data
will be conducted independently by two reviewers
(SD and MAN).
Studies will be labelled in the data extraction
process in order to make a taxonomy of e-Health
solution types. After discussion, the authors agreed
upon using a deductive method consisting of the
following prefixed categories: AAL-Activities of
daily living, AAL-Wayfinding and tracking, AAL-
security and safety, (robotic) assistive technology,
telehealth and telemedicine, virtual reality,
technologies for personal organization and
technologies for psychosocial support.
Where possible, data will be pooled in statistical
meta-analysis and effect sizes with 95% confidence
intervals will be calculated. In order to decide
whether comparison of individual studies is justified,
heterogeneity will be assessed statistically using the
standard Chi-square test and explored using subgroup
analysis based on the different included study
designs. If statistical pooling is impossible the review
findings will be presented in narrative form
4 RESULTS
Figure 1 depicts a flow diagram illustrating the
selection process of the review. After elimination of
duplicates the systematic literature review resulted in
a total of 12999 hits. First-level screening of reference
titles was completed in January 2019 and resulted in
Publications
screened
(n = 12 999)
Publications
potentially relevant
to be assessed further
(n = 999)
PubMed (n = 3 062)
CINAHL (n = 1 961)
The Cochrane Library (n = 1 125)
PsycINFO (n = 2 468)
Web of Science (n = 2 015)
Embase (n = 2 338)
Socialogical Abstracts (n = 3 062)
e-Health Solutions for Aging in Place with Cognitive Impairment: Preliminary Results of a Systematic Review
271

12000 exclusions and 999 references that are
potentially relevant. Second-level screening by
abstract is in progress. Final assessment of the
remaining publications by reading the full texts will
be completed by April 2019. Data extraction and
synthesis of the included studies is planned to be
completed by July 2019.
5 CONCLUSIONS
Aging in place is a worldwide concern urging policy
makers to expand their strategies with promising
innovative approaches. E-Health technologies seem
to offer such possibilities, even for older adults living
with cognitive impairment. Moreover, the social
burden on informal care could also potentially be
alleviated by e-Health solutions. Since development
of these solutions is accelerating in fast pace, it is
important to inform the implementation of effective
e-Health solutions based on the most recent research
evidence. This review will revisit the literature and
identify promising e-Health solutions for AIP with
cognitive impairment. Therefore, this review will
gain insight into the potential role of e-Health in the
strengthening of community care for older adults with
cognitive impairments and in the associated informal
care.
ACKNOWLEDGEMENTS
This work was made possible through funding from
the Fonds Wetenschappelijk Onderzoek (FWO,
Belgium) and Fonds de Recherche de Québec (FRQ,
Canada). The authors declare no conflicts of interest.
REFERENCES
Alzheimer’s Association. 2016. Alzheimer’s Disease Facts
and Figures. Alzheimer’s & Dementia, 12, 459-509.
Afram, B., Stephan, A., Verbeek, H., Bleijlevens, M. H. C.,
Suhonen, R., Sutcliffe, C., Raamat, K., Cabrera, E.,
Soto, M. E., Hallberg, I. R., Meyer, G. and Hamers, J.
P. H. 2014. Reasons for Institutionalization of People
with Dementia: Informal Caregiver Reports From 8
European Countries. Journal of American Medical
Directors Association, 15, 108-116.
Ahn, M., Kang, J., and Kwon, H. J. 2019. The Concept of
Aging in Place as Intention. The Gerontologist,
gny167.
Artero, S., Ancelin, M.-L., Portet, F., Dupuy, A., Berr, C.,
Dartigues, J.-F., Tzourio, C., Rouaud, O., Poncet, M.,
Pasquier, F., Auriacombe, S., Touchon, J., and Richie,
K. 2015. Risk Profiles for mild cognitive impairment
and progression to dementia are gender specific.
Journal of Neurology, Neurosurgery & Psychiatry,
79(9), 979-984.
Balta-Ozkan, N., Davidson, R., Bicket, M., and Whitmarsh,
L. 2013. Social barriers to the adoption of smart homes.
Energy Policy, 63, 363-374.
Banaszak-Holl, J., Fendrick, A. M., Foster, N. L., Herzorg,
A. R., Kabeto, M. U., Kent, D. M., Straus, W. L. and
Langa, K. M. 2004. Predicting Nursing Home
Admission: Estimates from a 7-Year Follow-up of a
Nationally Representative Sample of Older Americans.
Alzheimer Disease & Associated Disorders, 18(2), 83-
89.
Blackman, S., Matlo, C., Bobrovitskiy, C., Waldoch, A.,
Fang, M. L., Jackson, P., Mihailidis, A., Nygård, L.,
Astell, A. and Sixsmith, A. 2016. Ambient Assisted
Living Technologies for Aging Well: A Scoping
Review. Journal of Intelligent Systems, 25(1), 55-69.
Centers for Disease Control and Prevention. 2009. Healthy
places terminology: Aging in place. Retrieved from
https://www.cdc.gov/healthyplaces/terminology.htm.
Eurostat. 2018. Population structure and Ageing. Retrieved
from https://ec.europa.eu/eurostat/statistics-
explained/index.php/Population_structure_and_ageing
.
Gnjidic, D., Stanaway, F. F., Cumming, R., Waite, L.,
Blyth, F., Naganathan, V., Handelsman, D. J. and Le
Couteur, D. G. 2012. Mild Cognitive Impairment
Predicts Institutionalization among Older Men: A
Population-Based Cohort Study. PLoS ONE, 7(9),
e46061.
Higgins, J. and Green, S. 2011. Cochrane handbook for
systematic reviews of interventions, Version 5.1.0
[updated March 2011].
Kim, K.-I., Gollamudi, S. S., and Steinhubl, S. 2017. Digital
technology to enable aging in place. Experimental
Gerontology, 88, 25-31.
Lau, K. M., Parikh, M., Harvey, D. J., Huang, C.-J. and
Farias, S. T. 2015. Early Cognitively Based Functional
Limitations Predict Loss of Independence in
Instrumental Activities of Daily Living in Older Adults.
Journal of the International Neuropsychological
Society, 21, 688-698.
Lauriks, S., Reinersmann, A., van der Roest, H. G.,
Meiland, F. J. M., Davies, R. J., Moelaert, F.,
Mulvenna, M. D., Nugent, C. D., Dröes, R. M. 2007.
Review of ICT-based services for identified unmet
needs in people with dementia. Aging Research
Reviews, 6, 223-246.
Lorenz, L., Freddolino, P. P., Comas-Herrera, A., Knapp,
M., and Damant, J. 2017. Technology-based tools and
services for people with dementia and carers: Mapping
technology onto the dementia care pathway. Dementia,
0(0), 1-17.
Löfqvist, C., Granbom, M., Himmelsbach, I., Iwarsson, S.,
Oswald, F. and Haak M. 2013. Voices on Relocation
and Aging in Place in Very Old Age – A Complex and
Ambivalent Matter. The Gerontologist, 53(6), 919-927.
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
272

Mateen, F. J., Oh, J., Tergas, A. I., Bhayani, N. H., and
Kamdar, B. B. 2013. Titles versus titles and abstracts
for initial screening of articles for systematic reviews.
Clinical Epidemiology, 5, 89-95.
Marikyan, D., Papagiannidis, S., and Alamanos, E. 2019. A
systemic review of the smart home literature: A user
perspective. Technological Forecasting & Social
Change, 138, 139-154.
Meiland, F., Innes, A., Mountain, G., Robinson, L., van der
Roest, H., García-Casal, J. A., Gove, D., Thyrian, J. R.,
Evans, S., Dröes, R.-M., Kelly, F., Kurz, A., Casey, D.,
Szcześniak, D., Dening, T., Craven, M. P., Span, M.,
Felzmann, H., Tsolaki, M. and Franco-Martín, M. A.
2017. Technologies to Support Community-Dwelling
Persons With Dementia: A Position Paper on Issues
Regarding Development, Usability, Effectiveness and
Cost-Effectiveness, Deployment, and Ethics. Journal of
Medical Internet Research Rehabilitation and Assistive
Technologies, 4(1), e1.
Ouzzani, M., Hammady, H., Fedorowicz, Z. and
Elmagarmid, A. 2016. Rayyan – a web and mobile app
for systematic reviews. Systematic Reviews, 5, 210.
Parra-Vidales, E., Soto-Pérez, F., Perea-Bartolomé, M. V.,
Franco-Martín, M. A., and Muñoz-Sánchez, J. L. 2017.
Online interventions for caregivers of people with
dementia: a systematic review. Actas Españolas de
Psiquiatría, 45(3), 116-126.
Ryman, F. V. M., Erisman, J. C., Darvey, L. M., Osborne,
J., Swartsenburg, E. and Syurina, E. V. 2018. Health
Effects of the Relocation of Patients with Dementia: A
Scoping Review to Inform Medical and Policy
Decision-Making. The Gerontologist, 0(0), 1-9.
Scott, J. L., Dawkins, S., Quinn, M. G., Sanderson, K.,
Elliott, K. E., Stirling, C., Schüz, B., and Robinson, A.
2015. Caring for the carer: a systematic review of pure
technology-based cognitive behavioral therapy (TB-
CBT) interventions for dementia carers. Aging &
Mental Health, 20(8), 793-803.
Tyack, C., and Camic, P. M. 2017. Touchscreen
interventions and the well-being of people with
dementia and caregivers: a systematic review.
International Psychogeriatrics, 29(8), 1261-1280.
van der Roest, H. G., Meiland, F. J. M., Comijs, H. C.,
Derksen, E., Jansen, A. P. D., van Hout, H. P. J., Jonker,
C. and Dröes, R.-M. 2009. What do community-
dwelling people with dementia need? A survey of those
who are known to care and welfare services.
International Psychogeriatrics, 21(5), 949-965.
Vincent, G. K. and Velkoff, V. A. 2010. The Next Four
Decades, The Older Population in the United States:
2010 to 2050, Current Population Reports.
Washington, DC: U.S. Census Bureau.
World Health Organization. 2018, February 5. Ageing and
health. Retrieved from https://www.who.int/news-
room/fact-sheets/detail/ageing-and-health.
World Health Organization. 2019. eHealth at WHO.
Retrieved from https://www.who.int/ehealth/en/.
e-Health Solutions for Aging in Place with Cognitive Impairment: Preliminary Results of a Systematic Review
273
