
Effect of Lifestyle Modification and Metformin on Fetuin-A and
Transforming Growth Factor-ß (TGF- ß) in Metabolic Syndrome
Melati Silvanni Nasution
1
, Dharma Lindarto
1*
1
Department of Internal Medicine, Faculty of Medicine, Universitas Sumatera Utara,
H. Adam Malik Hospital, JalanBunga Lau No 17, Medan 20136, Indonesia.
Keywords: Metabolic syndrome, lifestyle modification, fetuin-A, TGF- ß
Abstract: Fetuin-A is a liver-synthesized protein that is secreted into the serum. Transforming growth factor-β (TGF-
β) is a polypeptide member of the TGF-β superfamily of cytokines. The purpose of this study is to evaluate
the effects of lifestyle modification and metformin on fetuin-A and Transforming Growth Factor-ß (TGF- ß)
in metabolic syndrome (MetS). Forty MetS subjects were randomly assigned to treatment with placebo
(n=20) or metformin (n=20) in addition to lifestyle modification for 12 weeks. All 40 participants completed
the study. After 12 weeks, both groups had significant reductions in weight, body mass index (BMI), waist
circumference (WC), systolic blood pressure (SBP) and diastolic blood pressure (DBP) (all p<0.001). The
placebo group also had significant improvement in fasting plasma glucose (FPG) and C-reactive protein
(CRP) (p<0,001 ; p<0.05 respectively). Weight, BMI, WC, FPG, 2-hour postprandial glucose (2h-PPG),
high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), fetuin-A and TGF- ß in the metformin
group decreased significantly compared to the placebo group. Reduction of plasma fetuin-A was
significantly associated with TG in the metformin group. Lifestyle modification and treatment with
metformin for 12 weeks improved cardio-metabolic risk factors in Mets and reduced fetuin-A levels.
1 INTRODUCTION
The Metabolic Syndrome (MetS) represents a
combination of cardio-metabolic risk factor
determinants including central adiposity, insulin
resistance, glucose intolerance, dyslipidemia, non-
alcoholic fatty liver disease (NAFLD) and
hypertension. It is rapidly increasing in prevalence
worldwide as a consequence of the obesity
epidemic. As a result, the Mets will have a
considerable impact on the global incidence of
cardiovascular disease and type 2 diabetes (T2DM)
(Bruce et al., 2009). Insulin resistance is thought to
be the primary underlying abnormality leading to
Mets (Reaven, 1988).
Fetuin-A (also known as human protein alpha-2-
Heremans-Schmid-glycoprotein, AHSG) and other
circulating proteins have been shown to be involved
in the regulation of insulin sensitivity. Fetuin-A is a
liver-synthesized protein that is secreted into the
serum. It can bind the insulin receptor and inhibit
insulin signaling in skeletal muscle and hepatocytes,
inhibiting insulin signal transduction and resulting in
insulin resistance in the target tissues (Srinivas et al.,
1993). In humans, higher levels of fetuin-A are
associated with higher TG, low-density lipoprotein
cholesterol (LDL-C), BMI, and insulin resistance
(Stefan et al., 2006). Higher fetuin-A concentrations
were associated with the accumulation of visceral
adipose tissue, a major component of the Mets (Ix et
al., 2009). The link between fetuin-A, obesity,
insulin resistance, NAFLD, and Mets in humans is
less clear. Some studies in adults have reported
significant associations between fetuin-A, NAFLD
and insulin resistance (Mori et al., 2006). Most of
these studies were cross-sectional and limited by
many confounders. Longitudinal studies are
preferable to clarify these metabolic relationships.
Transforming growth factor-β (TGF-β) is a
polypeptide member of the TGF-β superfamily of
cytokines. The TGF-β superfamily consists of TGF-
β, activins, inhibins, growth differentiation factors,
and bone morphogenetic proteins (BMPs). The
TGF-β superfamily proteins share common
sequences and motifs to exert their various
biological actions, including cell growth,
differentiation, proliferation, migration, adhesion,
Nasution, M. and Lindarto, D.
Effect of Lifestyle Modification and Metformin on Fetuin-A and Transforming Growth Factor-ß (TGF- ß) in Metabolic Syndrome.
DOI: 10.5220/0010018704650472
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 465-472
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
465

apoptosis, and extracellular matrix (ECM)
production. Metabolic syndrome is mostly
characterized as visceral fat obesity with multiple
cardiovascular risk factors, including elevated blood
pressure, hyperglycemia, and dyslipidemia.
Therefore, an understanding of the molecular
mechanism by which visceral obesity is promoted is
essential for preventing cardiovascular events in
individuals with MetS (Ken-ichiet al., 2011).
Lifestyle modifications (LSM) to address
overweight, physical inactivity and an atherogenic
diet have been recommended as a foundation for the
management ofMetS(Eckel et al., 2005). However,
LSM alone is often unable to achieve clinically
meaningful weight loss (UKPDS, 1998).
Metformin, a biguanide oral antidiabetic agent,
has been shown to reduce weight, hyperinsulinemia,
and hyperglycemia in adult patients with T2D. It is
recommended as first-line pharmacotherapy in
overweight and obese T2D patients (Shroff et al.,
2010). While metformin has been found to attenuate
the insulin-sensitizing effect of exercise, it has been
found to have beneficial effects on inhibition of
platelet aggregation, antioxidant activity, weight
reduction, lipid parameters (total cholesterol, HDL-
C, LDL-C and TG) and arterial hypertension
(Glueck et al., 2001, Wulffeléet al., 2004, Pasquali
et al., 2000). Metformin can be given safely to
euglycemic patients, as it does not induce
hypoglycemia (Linet al., 2000). Furthermore, in
ob/ob mice, a model of hepatic steatosis, metformin
reversed hepatomegaly, hepatic fat accumulation,
and ALT abnormalities by reducing hepatic tumor
necrosis factor-α (TNF-α) expression (WHO, 2004).
The aim of this study was to assess the effect of
LSM on cardio-metabolic risk factors, fetuin-A and
TGf-ß levels with or without metformin in relation
to the improvement of insulin sensitivity in patients
with the Mets.
2 MATERIALS AND METHODS
Study subjects who met the 2006 IDF definition of
the metabolic syndrome were recruited from the
nurse of H. Adam Malik Hospital in Medan,
Indonesia. The criteria included central obesity (WC
of ≥ 90 cm in men and ≥ 80 cm in women of Asian
ethnicity) plus any 2 of the following 4 factors:
elevated triglycerides (≥ 150 mg/dL) or specific
treatment for this lipid abnormality, reduced HDL-C
(< 40 mg/dL in men and < 50 mg/dL in women) or
specific treatment for this lipid abnormality, elevated
BP blood pressure (SBP ≥130 mmHg or DBP ≥ 85
mmHg) or treatment of previously diagnosed
hypertension, and elevated FPG (≥ 100 mg/dL) or
previously diagnosed type 2 diabetes (WHO, 2004,
IDF, 2006). Exclusion criteria included smoking,
known cardiovascular disease or any major illness,
and use of medication that could affect laboratory
test results. Forty subjects gave their full informed
consent to participate and undergo LSM for 12
weeks. They were assigned randomly to treatment
with either placebo or metformin.
Each participant was advised to take one capsule
three times a day after meal. For the placebo group,
the capsule contained calcium gluconate 500 mg.
For the metformin group, the capsule contained
metformin 500 mg. No vitamins or other nutritional
supplements were prescribed. Prior to initiation and
during the study, all the participants discussed LSM
including diet and physical activity with a trained
health nurse. To facilitate behavior change, each
participant received an instructional leaflet and a
diary to record behavioral performance, diet,
physical activity, WC and weight. Every week, all
participants attended a follow-up meeting for
confirmation of compliance and monitoring of any
health and safety problems related to behavioral
changes and treatment.
2.1 Anthropometric and Body
Composition Measurements
Baseline anthropometric measures were taken. The
following BMI categories appropriate for Asians
were used: underweight, BMI < 18.5 kg/m
2
; normal,
18.5 to 22.9 kg/m
2
; overweight, 23.0 to 24.9 kg/m
2
;
obese class I, 25.0 to 29.9 kg/m
2
; obese class II BMI
≥ 30.0 kg/m
2
(Misra et al., 2007). BMI was
measured every week to assess the immediate effect
of LSM.
2.2 Diet and Exercise Regimen
For 12 weeks, all subjects followed a weight
maintenance diet (total calories per day divided into
55 to 60% carbohydrate, 15 to 20% protein and 20 to
25% fat) and moderate exercise in accordance with
recommendations from the Endocrinology
Association of Indonesia (Perkeni, 2011). All
subjects were free-living and consumed self-selected
foods from a list of food replacements made
according to their individual dietary habits. The
dietitian reviewed the participants' diet on a weekly
basis to ensure compliance.
The exercise program consisted of moderate
aerobic exercise at least 3 times per week, with a
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
466
minimum of 30 minutes for each session (Perkeni,
2011). Each session included 5 minutes of warm-up,
20 minutes of main exercises, and 5 minutes of
relaxation exercises. Each training session was
supervised by a physiotherapist.
2.3 Blood Pressure and Blood Sample
Analysis
Blood pressure was averaged from two
measurements using a mercurial
sphygmomanometer after a 10-minute rest. All
subjects reported for blood sampling in the morning
after an overnight fast. Blood samples were
centrifuged for 15 minutes, after which plasma- and
serum-containing tubes were stored at -20
°
C until
analysis. Blood glucose was measured by
photometer autoanalyzer Modular P800. Plasma
HDL-C, LDL-C, and TG were measured using
ARCHITECT ci8200 (Abbott Diagnostics, USA).
High-sensitivity CRP was measured by sensitive
immunoassay using Immulite® 1000 Analyzer
System (Siemens Healthcare, Germany). HbA1c
measurement was done by high-performance liquid
chromatography (HPLC) using D-10™ (Bio-Rad,
USA). Homeostatic model assessment of insulin
resistance (HOMA-IR) was computed using the
formula:
HOMA-IR = FPG x fasting serum insulin / 22.5
where FPG is expressed in mmol/L and fasting
serum insulin in mU/L. Fetuin-A determination was
performed by human fetuin-A enzyme immunoassay
and TGF-ß also by enzyme immunoassay
2.4 Statistical Analysis
Data were presented as mean ± SD. The normality
assumption of data from the placebo group and the
metformin group was evaluated and confirmed using
the Shapiro-Wilk normality test. Differences
between and within groups were tested using the
dependent t-test and independent sample t-test.
Abnormal data were tested using the Mann-Whitney
U test, Wilcoxon test, and Spearman's correlation
coefficient test. Two-sided p-values of less than 0.05
were regarded as statistically significant. The data
were analyzed using SPSS software.
The local Ethics Committee approved the study.
3 RESULTS
All 40 participants completed the study for 12
weeks. Analysis of baseline characteristics showed
no significant differences in selected cardio-
metabolic risk factors and fetuin-A (Table 1). After
12 weeks, both groups had reductions in weight,
BMI, WC, SBP, and DBP. Reduction in CRP was
also found in the placebo group; fetuin-A was
reduced in the metformin group. Compared to
placebo, weight, BMI, WC, FPG, 2h-PPG, HDL-C,
and TG had decreased significantly in the metformin
group (Table 2).
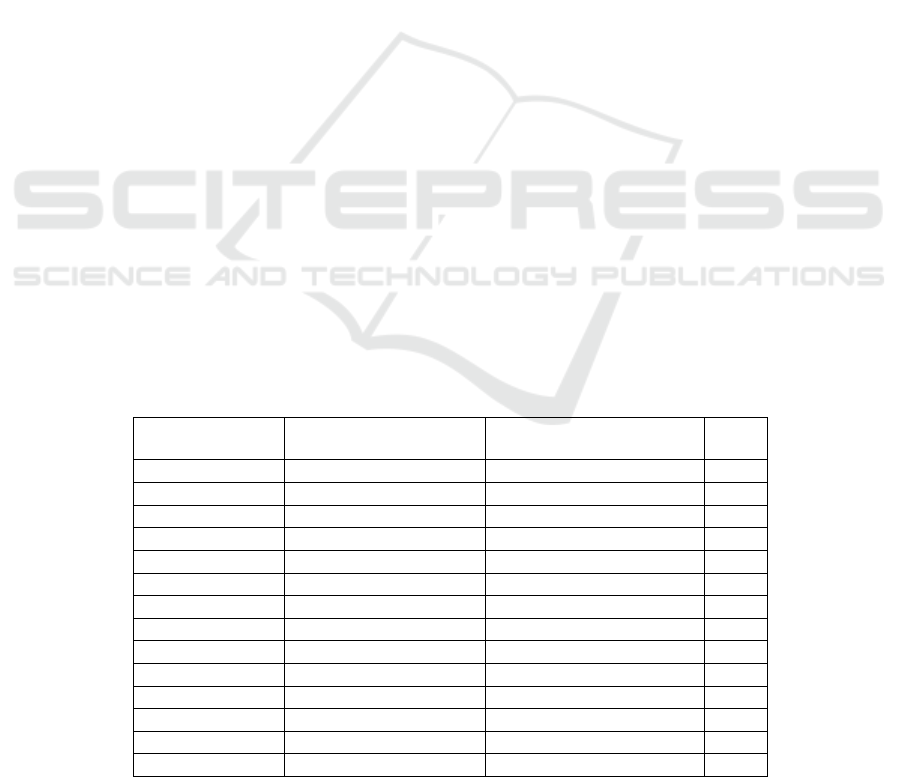
Table 1. Baseline Characteristic
Characteristicts Placebo group (n = 20)
Mean (SD)
Metformin group (n = 20)
Mean (SD)
P
Age, yr
40.1 (5.78) 42.7 (5.2)
0.149
Weight, kg
77.6 (11.0) 81.4 (14.6)
0.354
BMI, kg/m²
32.1 (4.1) 34.2 (5.6)
0.180
WC, cm
95.7 (7.3) 97.9 (11.5)
0.449
SBP, mmHg
123.5 (11.4) 127.0 (20.3)
0.989
DBP, mmHg
82.2 (10.5) 80.8 (11.0)
0.495
HDL-C, mg/dL
46.4 (8.5) 48.9 (16.4)
0.968
TG, mg/dL
147.5 (30.6) 152.3 (66.9)
0.799
FPG, mg/dL
83.4 (10.6) 84.9 (8.9)
0.341
2h-PPG, mg/dL
114.9 (35.4) 105.1 (22.4)
0.602
HOMA-IR
1.13 (0.94) 1.0 (0.6)
0.700
CRP, mg/dL
3.6 (2.5) 3.9 (2.4)
0.699
Fetuin-A, µg/mL
461.4 (74.6) 459.0 (62.8)
0.911
TGF-ß1, pg/mL
47479,34 (6942.01) 45272.06 (3711.22)
0.380
Effect of Lifestyle Modification and Metformin on Fetuin-A and Transforming Growth Factor-ß (TGF- ß) in Metabolic Syndrome
467
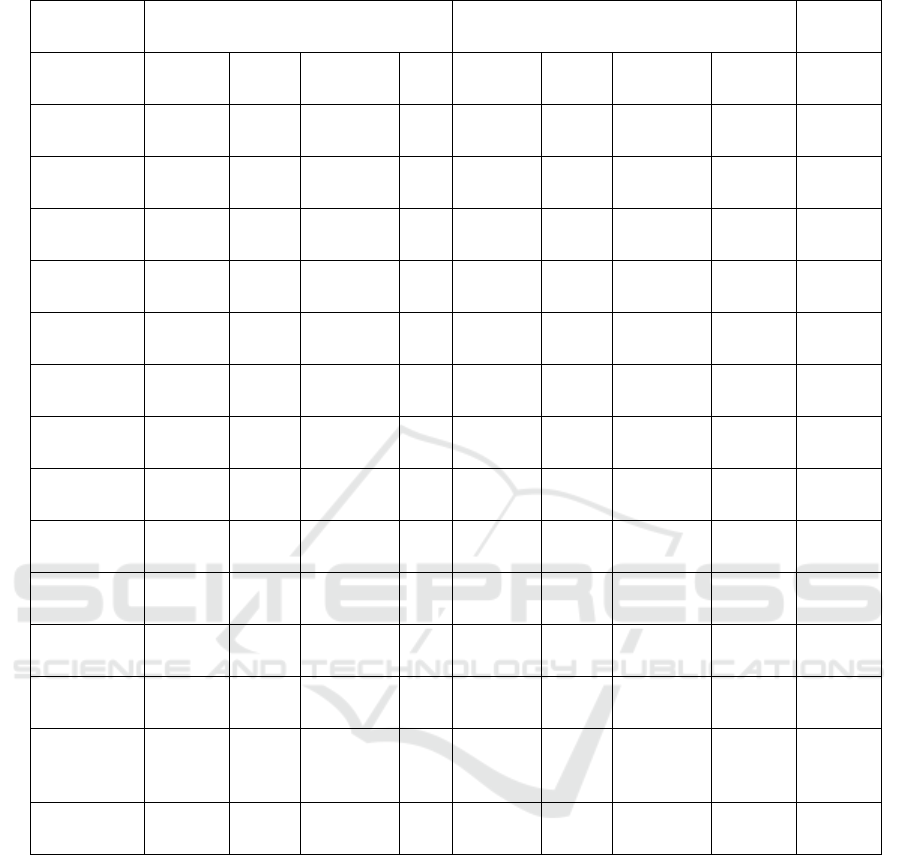
Table 2. Change in selected cardio-metabolic risk factors from baseline and at 12 weeks, N= 40.
Parameter
Placebo group
(n=20)
Metformin group
(n=20)
P
Baseline
12
weeks
Difference P Baseline
12
weeks
Difference P
Weight (SD),
kg
77.6
(11.0)
75.2
(10.8)
-2.3
0.00
1**
81.4
(14.6)
77.4
(14.5)
-3.9 0.001** 0.001**
BMI (SD),
kg/m²
32.1 (4.1)
30.9
(4.1)
-1.1
0.00
1**
342 (5.6)
32.4
(5.6)
-1.8 0.001** 0.002**
WC (SD), cm
95.7 (7.3)
89.9
(7.5)
-5.8
0.00
1**
97.9
(11.5)
91.8
(10.7)
-6.2 0.001** 0.047*
SBP (SD),
mmHg
123.5
(11.4)
114.0
(8.2)
-9.5
0.00
7**
127.0
(20.3)
112.8
(8.5)
-14.3 0.001** 0.160
DBP (SD),
mmHg
82.2
(10.5)
69.0
(5.5)
-31.8
0.00
1**
80.6
(11.0)
67.5
(7.2)
-13.3 0.001** 0.089
HDL-C (SD),
mg/dL
46.4 (8.5)
45.3
(10.0)
-1.1
0.62
8
489 (16.4)
45.5
(9.8)
-2.4 0.653 0.043*
TG (SD),
mg/dL
147.5
(50.5)
153.3
(67.9)
5.8
0.63
4
152.3
(66.9)
149.0
(102.4)
-3.3 0.147 0.045
FPG (SD),
mg/dL
83.4
(10.6)
91.7
(20.6)
8.3
0.00
1**
84.9 (8.9)
87.7
(10.7)
2.8 0.305 0.013*
2h-PPG
(SD), mg/dL
114.9
(35.4)
112.5
(37.7)
-2.5
0.71
7
105 (22.4)
102.3
(19.3)
-2.8 0.491 0.007**
HOMA-IR
(SD)
1.13
(0.94)
1.68
(0.25)
-0.5
0.61
0
1.03
(0.61)
1.03
(0.4)
0 0.956 1.000
CRP (SD),
mg/dL
3.6 (2.5)
3.0
(2.2)
-0.6
0.04
8*
3.9 (2.4)
3.5
(1.9)
-0.6 0.327 0.133
Fetuin-A
(SD), µg/mL
461.4
(74.6)
42.6
(84.8)
-34.8
0.15
8
459.0
(62.8)
398.1(
101.4)
-610 0.005** 0.477
TGF-ß1
(SD), pg/mL
47479.34
(6942.01)
47346.
69
(6654.
11)
-132.65
1.00
0
45272.06
(3711.22)
4458.7
1
(8232.
4)
-1013.35 0,661 0.353
4 DISCUSSION
Obesity is the most common risk factor for MetS
and NAFLD (Reinehet al., 2008). As suggested by
novel evidence, hepatocytes from fatty liver release
factors called hepatokines (e.g., fetuin-A, sex
hormone-binding globulin) into the circulation that
are directly involved in local pathogenesis, systemic
inflammation and hepatic insulin resistance (Reaven
et al., 1988). The fetuin-A levels of obese children
are apparently similar to those of adults (Ohkawaraet
al., 2007). A study by Mori and colleagues did not
find a significant association between fetuin-A and
insulin resistance in type 2 diabetic subjects (Mori et
al., 2006).In contrast, other studies demonstrated a
relationship between fetuin-A and insulin resistance
in adults without T2D (Stefan et al., 2006).Fetuin-A
concentrations decreased significantly in obese
children after substantial weight loss after 1 year but
were apparently unchanged in those who did not
lose weight (Ohkawaraet al., 2007). Our study found
that fetuin-A decreased significantly with LSM and
metformin treatment for 12 weeks, possibly
associated with weight reduction.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
468

A recent systematic review showed a dose-response
effect of aerobic exercise on visceral adiposity, but
the ability of exercise to reduce visceral adipose
tissue was less robust in those with metabolic
disorders (Wing et al., 2001). It remains unclear if
the same dose-response effect on central adiposity
will also be seen in those with MetS. Nevertheless,
during weight maintenance, regular exercise still has
an important role in abdominal fat loss and may help
prevent weight regain in those who have
successfully lost weight (Ross et al., 2004).
However, even in the absence of weight loss,
exercise has been shown to reduce visceral adipose
tissue (Stone et al., 2005). Our study demonstrated
that weight, BMI and WC decreased significantly in
the course of 12 weeks of LSM in both groups.
The National Cholesterol Education Program
Adult Treatment Panel III (NCEP: ATP-III)
recommends LDL-C reduction as the primary
treatment goal for CVD risk reduction. Therapeutic
lifestyle changes, particularly improvement in
physical activity and weight management, need to be
instituted in those individuals with the Mets to
address elevated TG and low HDL-C (Kelley, 2007).
Although aerobic exercise training has generally
been shown to increase HDL-C and decrease TG, its
effects on LDL-C has been mixed (Kodama et al.,
2007, Stefanick et al., 1998). Beneficial effects of
exercise training on lipids and lipoproteins may have
an additional impact when combined with dietary
modification and weight loss (Whelton et al., 2002).
Our study demonstrated HDL-C and TG did not
decrease significantly in the course of 12 weeks of
LSM on both groups.
A recent meta-analysis of randomized controlled
trials studying the effect of aerobic exercise on BP
showed a reduction in systolic and diastolic BP by
approximately 3.8 and 2.6 mmHg, respectively
(Bacon et al., 2004). Although the effect of aerobic
exercise on blood pressure is small and not
consistently observed in all studies, there may be
additional benefit when combined with dietary
modification and/or weight loss (Cornier et al.,
2008). Our study demonstrated significant
reductions in systolic and diastolic BP in both
groups in the course of 12 weeks of LSM.
Insulin resistance is another core component of
the Mets that requires careful attention. Weight loss
and LSM can lead to clinically meaningful
improvements in insulin sensitivity and should be
considered the primary therapeutic options for
treating insulin resistance. The difficulties and
frustrations associated with weight loss efforts and
LSM have driven the demand for using
pharmaceutical agents that target insulin resistance
in a more direct fashion. The exact role for these
agents is less clear. Several randomized controlled
trials have shown that agents targeting insulin
resistance can help prevent the progression to T2D
in individuals with impaired glucose tolerance
(IGT). These studies did not directly target
individuals with the Mets. It is unclear whether these
agents truly prevent progression to T2D or simply
treat glucose intolerance or mild hyperglycemia. In
addition, studies have not clearly shown whether
these agents improve cardiovascular outcomes. As
with weight loss medications, the goals for the use
of agents targeting insulin resistance must be clear
(Henniger al., 2008). Our study demonstrated
HOMA-IR did not decrease significantly in both
groups.
Fetuin-A induces low-grade inflammation, which
is also associated with MetS and an atherogenic lipid
profile (Reiner et al., 2008, Ridker, 2001).
Inflammation assessed by elevated CRP
measurements has been linked to excess
cardiovascular risk and Mets (Ridker et al., 2003,
Gonzálezet al
., 2006). CRP is a general marker of
inflammation, making it suitable to assess in
individuals with metabolic syndrome. Elevated
levels of CRP are associated with increased WC,
insulin resistance, BMI and hyperglycemia; and in
the presence of more components of the Mets
(Deepa et al., 2006, Guldikenet al., 2007, Bahia et
al., 2006, Gonzálezet al., 2006, Clearfield, 2005).
Because Mets have been linked with a greater
chance of future cardiovascular events, CRP levels
may be an important independent predictor of
unfavorable outcomes in those already with Mets
(Van Dillen et al., 2004). There are, however, no
currently recommended direct therapies targeting
inflammation. LSM and weight loss result in
decreased CRP concentrations, as does the treatment
of the other associated comorbidities such as
dyslipidemia, elevated blood pressure, insulin
resistance and hyperglycemia (Devaraj, 2007,
Knowles et al., 2002). Our study observed CRP
decreased significantly only in the placebo group.
It has not been determined how the Pro 10
variant form of the TGF-β1 protein is linked to
visceral adiposity and elevated levels of circulating
insulin, there is a possibility that TGF-β1 is involved
in the insulin resistance with obesity. Since
macrophage infiltration into adipose tissue causes
insulin resistance and since coculture experiments
with human adipocytes and macrophages have
shown that downstream effectors of TGF-β such as
PAI-1, collagen VI, and phosphorylated Smad were
Effect of Lifestyle Modification and Metformin on Fetuin-A and Transforming Growth Factor-ß (TGF- ß) in Metabolic Syndrome
469

increased in both macrophages and adipocytes,
TGF-β has the potential for increasing insulin
resistance (Ken-ichi, 2011).
In experimental animal studies, Samad et al.
reported enhancement of gene and protein
expression of TGF-β1 in two strains of genetically
obese mice (ob/ob and DB/DB) compared with that
in lean mice(Samad, 1997) and Raju et al. showed
that an obese state increases levels of TGF-β1 but
not TGF-β2 in platelets of Zucker rats, recognized as
an experimental model of Mets (Raju, 2006).
Moreover, Sciarretta et al. showed that serum levels
of inflammatory markers, including C-reactive
protein, tumor necrosis factor-alpha, and TGF-β, in
hypertensive patients with MetS were significantly
higher than those in patients without MetS (Ken-
ichi, 2011).
5 CONCLUSION
LSM decreased CRP, human fetuin-A
concentrations, TGF-ß and selected cardio-metabolic
risk factors in this 12-week study. These findings
raise the possibility that fetuin-A may directly
promote the Mets phenotype in humans and there is
a possibility that TGF-ß is involved in the insulin
resistance with obesity. The selected cardio-
metabolic factors significantly improved with
metformin to the same degree as with the LSM.
Longitudinal and larger scale studies are needed to
evaluate the direction of the observed associations,
the regulatory factors that alter serum fetuin-A
concentrations, its effects on cardiovascular events,
and the long-term effects of metformin on selected
cardio-metabolic risk factors.
CONFLICT OF INTERESTS
The authors declare that there is no conflict of
interests regarding the publication of this paper.
REFERENCES
Bacon SL, Sherwood A, Hinderliter A, Blumenthal J.
2004. Effects of exercise, diet and weight loss on high
blood pressure. Sports Med. 34(5):307-16.
Bahia L, Aguiar LG, Villela N, Bottino D, Godoy-Matos
AF, Geloneze B, et al. 2006. Relationship between
adipokines, inflammation, and vascular reactivity in
lean controls and obese subjects with metabolic
syndrome. Clinics (Sao Paulo). 61(5):433-40.
Bruce KD, Byrne CD. 2009. The metabolic syndrome:
Common origins of a multifactorial disorder. Postgrad
Med J. 85(1009):614-21.
Clearfield MB.2005. C-reactive protein: A new risk
assessment tool for cardiovascular disease. J Am
Osteopath Assoc. 105(9):409-16.
Cornier MA, Dabelea D, Hernandez TL. 2008. The
metabolic syndrome. Endocrine Rev. 29(7):777-822.
Deepa R, Velmurugan K, ArvindKet, Sivaram P, Sientay
C, Uday S, et al. 2006. Serum levels of interleukin 6,
C-reactive protein, vascular cell adhesion molecule 1,
and monocyte chemotactic protein 1 in relation to
insulin resistance and glucose intolerance—The
Chennai Urban Rural Epidemiology Study (CURES).
Metabolism. 55(9):1232-8.
Devaraj S, Rogers J, Jialal I. 2007. Statins and biomarkers
of inflammation. CurrAtheroscler Rep. 9(1):33-41.
Eckel RH, Grundy SM, Zimmet PZ. 2005. The metabolic
syndrome.Lancet. 365(9468):1415-28.
Glueck CJ, Fontaine RN, Wang P, Subbiah MT, Weber K,
Illig E, et al. 2001. Metformin reduces weight,
centripetal obesity, insulin, leptin, and low-density
lipoprotein cholesterol in nondiabetic, morbidly obese
subjects with body mass index greater than 30.
Metabolism. 50(7):856-61.
González AS, Guerrero DB, Soto MB, et al. 2006.
Metabolic syndrome, insulin resistance and the
inflammation markers C-reactive protein and ferritin.
Eur J Clin Nutr. 60(6):802-9.
González AS, Guerrero DB, Soto MB, et al. 2006.
Metabolic syndrome, insulin resistance and the
inflammation markers C-reactive protein and ferritin.
Eur J Clin Nutr. 60(6):802-9.
Grundy SM. 2004. Obesity, metabolic syndrome, and
cardiovascular disease. J ClinEndocrinolMetab.
89(6):2595-600.
Guldiken S, Demir M, Arikan E, Turgut B, Azcan S,
Gerenli M, et al. 2007. The levels of circulating
markers of atherosclerosis and inflammation in
subjects with different degrees of body mass index:
Soluble CD40 ligand and high-sensitivity C-reactive
protein. Thromb Res. 119(1):79-84.
Hennige AM, Staiger H, Wicke C, Machiaco F, Fritsche
A, Haring HU, et al. 2008. Fetuin-A induces cytokine
expression and suppresses adiponectin production.
PLoS One. 3(3):e1765.
International Diabetes Federation. 2006. The IDF
consensus worldwide definition of the metabolic
syndrome. Brussels: International Diabetes Federation.
http://www.idf.org/webdata/docs/
IDF_Meta_def_final.pdf.
Ix JH, Wassel CL, Chertow GM, Koster A, Johnson KC,
Tylavsky FA, et al. 2009. Fetuin-A and change in
body composition in older persons. J
ClinEndocrinolMetab. 94(11):4492-8.
Kelley GA, Kelley KS. 2007. Effects of aerobic exercise
on lipids and lipoproteins in adults with type 2
diabetes: A meta-analysis of randomized controlled
trials. Public Health. 121(9):643-55.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
470

Ken-ichi A, Yasumasa I, Shusuke Y, Masashi A, and
Toshio M. 2011. Transforming growth factor-ß1 as a
common target molecule for the development of
cardiovascular diseases, renal insufficiency, and
metabolic syndrome. Cardiology research and
practice.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF,
Lachin JW, Walker EA. et al. 2002. Reduction in the
incidence of type 2 diabetes with lifestyle intervention
or metformin. N Engl J Med. 346(6):393-403.
Kodama S, Tanaka S, Saito K, Shu M, Sone Y, Onitake F,
et al. 2007. Effect of aerobic exercise training on
serum levels of high-density lipoprotein cholesterol: A
meta-analysis. Arch Intern Med. 167(10): 999-1008.
Lin HZ, Yang SQ, Chuckaree C, Kuhadja F, Ronnet G,
Diehl AM, et al. 2000. Metformin reverses fatty liver
disease in obese, leptin-deficient mice. Nat Med.
6(9):998-1003.
Mazza A, Fruci B, Garinis GA, Giuliano S, Malaguarnera
R, Belfiore A, et al. 2012. The role of metformin in the
management of NAFLD.Exp Diabetes Res.
2012:716404.
Miller WC, Koceja DM, Hamilton EJ.1997. A meta-
analysis of the past 25 years of weight loss research
using diet, exercise or diet plus exercise intervention.
Int J Obes Relat Metab Disord. 21(10):941-7.
Misra A, Misra R, Wijesuriya M. 2007. The metabolic
syndrome in South Asians. In: Mohan V, RaoGundu
HR, eds. Type 2 diabetes in South Asians.
Epidemiology, risk factors, and prevention. New
Delhi: Jaypee Bros., 76-96.
Mori K, Emoto M, Yokoyama H, Araki T, Teramura M,
Koyama H, et al. 2006. Association of serum fetuin-A
with insulin resistance in type 2 diabetic and
nondiabetic subjects. Diabetes Care. 29(2):468.
Ohkawara K, Tanaka S, Miyachi M, Ishikawa-Takata K,
Tabata I. 2007. A dose-response relation between
aerobic exercise and visceral fat reduction: Systematic
review of clinical trials. Int J Obes. 31(12):1786-97.
Orchard TJ, Temprosa M, Goldberg R, Haffner S, Rather
R, Marcovina S, et al. 2005. The effect of metformin
and intensive lifestyle intervention on the metabolic
syndrome: The Diabetes Prevention Program
randomized trial. Ann Intern Med. 142(8):611-9.
Pasquali R, Gambineri A, Biscotti D, Viccenati V,
Gagliardi L, Colitta D, et al. 2000. Effect of long-term
treatment with metformin added to hypocaloric diet on
body composition, fat distribution, and androgen and
insulin levels in abdominally obese women with and
without the polycystic ovary syndrome. J
ClinEndocrinolMetab. 85(8):2767-74
Perkeni. 2011. KonsensusPengelolaandanPencegahan
Diabetes Mellitus Type 2 Di Indonesia.
PerkumpulanEndokrinologi Indonesia.
Raju J, Bajaj G, Chrusch J, and Bird RP. 2006. Obese state
leads to elevated levels of TGF-β and COX isoforms
in platelets of Zucker rats,"Molecular and Cellular
Biochemistry. 284(1) 19–24.
Ratner R, Goldberg R, Haffner S, Marcovina S, Orchard
T, Fowler S, et al. 2005. Impact of intensive lifestyle
and metformin therapy on cardiovascular disease risk
factors in the diabetes prevention program. Diabetes
Care. 28(4):888-94.
Reaven GM. 1988. Banting lecture 1988. Role of insulin
resistance in human disease.Diabetes. 37(12):1595-
607.
Reinehr T, Roth CL. 2008. Fetuin-A and its relation to
metabolic syndrome and fatty liver disease in obese
children before and after weight loss. J
ClinEndocrinolMetab. 93(11):4479-85.
Ridker PM. 2001. High-sensitivity C-reactive protein:
Potential adjunct for global risk assessment in the
primary prevention of cardiovascular disease.
Circulation. 103(13):1813-8.
Ridker PM, Buring JE, Cook NR, et al. 2003. C-reactive
protein, the metabolic syndrome, and risk of incident
cardiovascular events: an 8-year follow-up of 14719
initially healthy American women. Circulation.
107(3):391-7.
Ross R, Janssen I, Dawson J, et al. 2004. Exercise-induced
reduction in obesity and insulin resistance in women: a
randomized controlled trial. Obes Res. 12(5):789-98.
Samad F, Yamamoto K, Pandey M, and Loskutoff DJ.
1997. Elevated expression of transforming growth
factor-β in adipose tissue from obese mice, Molecular
Medicine, 3(1)37–48
Sharoff CG, Hagobian TA, Malin SK, et al. 2010.
Combining short-term metformin treatment and one
bout of exercise does not increase insulin action in
insulin-resistant individuals. Am J Physiol Endocrinol
Metab. 298(4): E815-23.
Srinivas PR, Wagner AS, Reddy LV, et al. 1993. Serum
alpha 2-HS-glycoprotein is an inhibitor of the human
insulin receptor at the tyrosine kinase level.
MolEndocrinol. 7(11):1445-55.
Stefan N, Hennige AM, Staiger H, et al. 2006. Alpha 2-
Heremans-Schmid glycoprotein/fetuin-A is associated
with insulin resistance and fat accumulation in the
liver in humans. Diabetes Care. 29(4):853-7.
Stefanick ML, Mackey S, Sheehan M, et al. 1998. Effects
of diet and exercise in men and postmenopausal
women with low levels of HDL- cholesterol and high
levels of LDL-C cholesterol. N Engl J Med.
339(1):12-20.
Stone NJ, Bilek S, Rosenbaum S. 2005. Recent National
Cholesterol Education Program Adult Treatment Panel
III update: adjustments and options. Am J Cardiol.
96(4A):53E-9E.
UK Prospective Diabetes Study (UKPDS) Group. 1998.
Effect of intensive blood-glucose control with
metformin on complications in overweight patients
with type 2 diabetes (UKPDS 34).UK Prospective
Diabetes Study (UKPDS) Group.Lancet.
352(9131):854-65.
Van Dielen FM, Buurman WA, Hadfoune M, Nijhuis J,
Greve JW. 2004. Macrophage inhibitory factor,
plasminogen activator inhibitor-1, other acute phase
proteins, and inflammatory mediators normalize as a
result of weight loss in morbidly obese subjects treated
Effect of Lifestyle Modification and Metformin on Fetuin-A and Transforming Growth Factor-ß (TGF- ß) in Metabolic Syndrome
471

with gastric restrictive surgery. J
ClinEndocrinolMetab. 89:4062-8.
Whelton SP, Chin A, Xin X, He J. 2002. Effect of aerobic
exercise on blood pressure: A meta-analysis of
randomized, controlled trials. Ann Intern Med.
136(7):493-503.
WHO Expert Consultation. 2004. Appropriate body-mass
index for Asian populations and its implications for
policy and intervention strategies.Lancet.
363(9403):157-63.
Wing RR, Hill JO. 2001. Successful weight loss
maintenance. Ann Rev Nutr 21:323-41.
Wulffelé MG, Kooy A, de Zeeuw D, Stehouwer CD,
Gansevoort RT. 2004. The effect of metformin on
blood pressure, plasma cholesterol, and triglycerides in
type 2 diabetes mellitus: A systematic review. J Intern
Med. 256(1):1-14.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
472
