
Determinants of TB-RO Affecting Confirmation Have Not Started
the Treatment
R. Kintoko Rochadi
1
, Erna Mutiara
2
and Syarifah
3
1
Department of Health Education and Behavioral Sciences, Universitas Sumatera Utara, Medan, Indonesia
2
Department of Biostatistics and Population, Universitas Sumatera Utara, Medan, Indonesia
3
Department of Health Education and Behavioral Sciences, Universitas Sumatera Utara, Medan, Indonesia
Keywords: Sociodemography, TB-RO Confirmation, Starting Treatment.
Abstract: Indonesia is 8th of the most TB-RO in the world. Indonesia for January-June 2010 there were 3.507
suspected TB-RO, 504 confirmed TB-RO and RO 377 were treated for TB. From 2012 to 2017 cases of TB-
RO in North Sumatra Province were 893 cases. A total of 717 cases (80.3%) underwent treatment, 20%
(176 Patients) did not want to undergo treatment. Cases that did not start treatment Became a source of
transmission of TB-RO in the community so that experienced Increase in TB-RO. For this reason, it is
important to know the factors that affect patients confirmed that TB-RO does not start treatment in Medan.
This type of observational research is case control design. The study population was all patients with TB-
RO in Medan City recorded in the e-TB Manager 61 patients data. Case sample was 13 people and the
control sample was 31 people. Interview of data collection using a questionnaire and analyzed by univariate
and bivariate. The results showed that many patients with TB-RO could not be met because of the
incompatibility of addresses with reviews those registered in the e-TB Manager and many had died.
Bivariate results had no relations with sociodemographic and behavioral-RO starting TB treatment.
1 INTRODUCTION
Cases of drug-resistant pulmonary TB (TB-RO) are
increasing at the global and Indonesian levels.
Currently Indonesia is ranked eighth in the order of
the most cases of TB-RO in the world (Ministry of
Health Republic of Indonesia, 2011). The main
factor causing an increase in TB-RO cases is due to
the management of TB patients not according to the
standard (ISTC) and program errors, health workers
and the community. In Indonesia from January to
June 2010 there were 3,507 suspected TB-ROs, 504
confirmed TB-ROs and 377 were treated with TB-
ROs. It is estimated that there are around 6,300 TB-
RO cases each year (Burhan, 2010).
From 2012 until 2017-RO TB cases in North
Sumatra province as many as 893 cases while it was
willing to undergo the treatment as many as 717
cases (80.3%), the rest almost 20% (176 patients)
did not want to undergo treatment. Cases that do not
want to start this treatment will be a source of
transmission of TB in the community so that the
RO-RO TB cases are increasing because it will
transmit TB-RO also to the surrounding community.
Of the patients who underwent the treatment is also
known that the dropout rate treatment from year to
year is still high, higher than the number that can be
tolerated, True i.e. 5% (provincial health office of
North Sumatra, 2018).
Medan is the region with the highest TB cases in
Sumatra RO Utara. Until November 2018-RO TB
cases that have been confirmed in the city of Medan
324, which has not yet started treatment 61 patients
(19%). More patients who already take medication
as many as 282 cases (81%), with the status of the
treatment was 119 patients (42%), more patients
with no status in the treatment (56%).
For that, we need to know the factors that affect
patients confirmed TB-RO but not initiate treatment
in Medan.
2 METHOD
The research was conducted in the city of Medan.
Using a case-control study design that is examining
factors that influence TB treatment RO. Population
case study of all patients who have no TB-RO
Rochadi, R., Mutiara, E. and Syarifah, .
Determinants of TB-RO Affecting Confirmation Have Not Started the Treatment.
DOI: 10.5220/0010014102130217
In Proceedings of the 3rd International Conference on Social and Political Development (ICOSOP 3 2019) - Social Engineering Governance for the People, Technology and Infrastructure in
Revolution Industry 4.0, pages 213-217
ISBN: 978-989-758-472-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
213
treatment and registered and have a valid address
corresponding e-TB Manager that is 13 people.
Population control TB-RO that has been treated with
a ratio of 3: 1, the total population of the cases
obtained 31 respondents. Collecting data using
interviews using questioner. the sample was 44 cases
and control. Analyze data by univariate and chi-
square test, the variables with P <0.05 to be related.
3 RESULT
3.1 Effect of Age with TB-RO
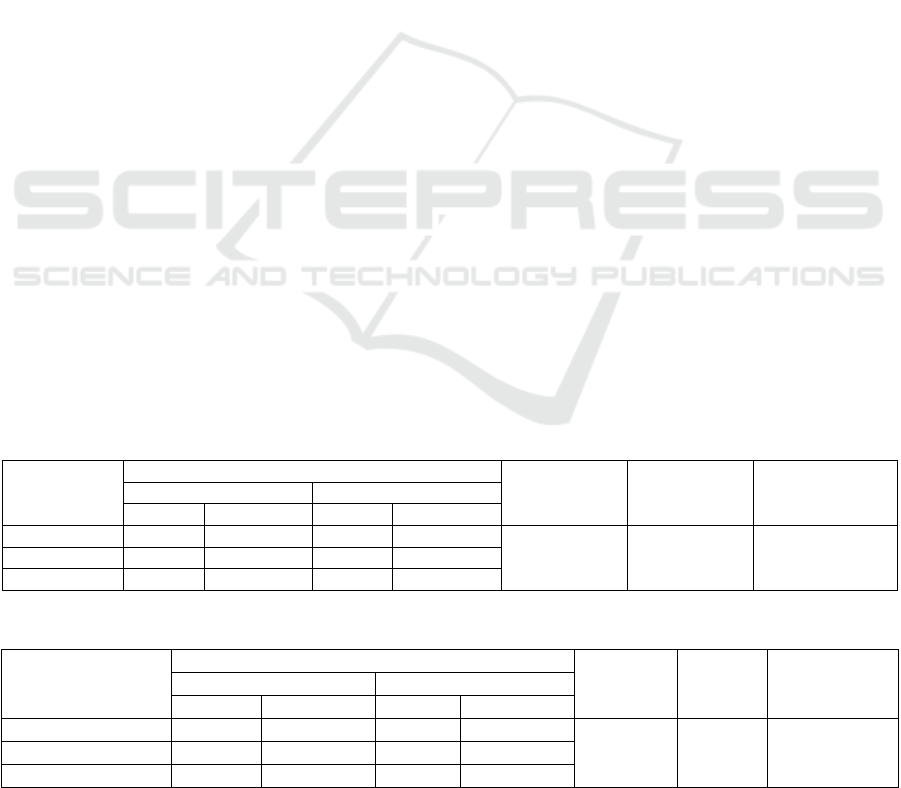
Based on Table 1, the proportion of respondents
aged ≤40 years in the case group as much as 30.8%
lower than the control group 41.9%. While
respondents aged> 40 years in the case group as
much as 69.2% greater than the control group
58.1%. Results using chi-square analysis showed
that it contained no significant effect between age
and treatment of TB-RO status (p = 0.723> 0.05).
Value OR = 1.61, indicating the status of TB-RO
treatment 1.6 times the tendency occurred on the
respondents were aged ≤ 40 years versus> 40 years.
The study is in line with research Yusi, et al
(2018) in Semarang obtained a value of p = 0.098,
which means there is no significant effect between
age determinant Treatment. Research Dessisa et al in
East Shoa, Ethiopia (2018) obtained by value p =
0,700 which means there is no effect between age
and treatment of TB-RO.At age range before
entering old age, a person is less able to adjust to the
problems encountered. In developmental age on
psychosocial aspects, someone who is considered to
have entered the middle to late adult life adjustment
skills of adaptation in which a person diagnosed
with TB disease will be having a good attitude and
behavior in achieving recovery to resolve the
problems faced. In contrast to the theory on the
results of the study, the prevalence of age> 40 years
higher than the ≤40 years.
3.2 Effect of Gender with TB-RO
Based on Table 2, the proportion of respondents who
sex men in groups of 8 cases (61.5%) and control
group of 20 people (64.5%). While respondents were
female in a case group of five people (38.5%) and a
control group of 11 people (35.5%). Results of
analysis using the chi-square test showed that in this
study there was no significant effect between the
sexes with RO TB treatment status (p = 1.000>
0.05). Value OR = 1.136, indicating the status of TB
treatment RO 1-time tendency occurred on the
respondents were male sex than women.
The study is in line with research Wulandari
(2015), that shows the value of p = 0.592, which
means there is no influence of gender with
medication adherence in patients with advanced lung
TB. Backed by research Anderson et al. (2013)
obtained the value p = 0.256, which means there is
no influence of gender with TB treatment success
RO.
In this case, each patient with TB has the
motivation to achieve recovery. Their motivation to
start treatment and regularly OAT drinking
behaviors will increase the likelihood of successful
treatment. The chances of success of TB treatment
between men and women are equal because TB
treatment programs do not discriminate based on
gender.
Table 1: Effect of age with status treatment.
Age
Status Treatment
P OR 95% Cl
Case Control
N % n %
≤40 years 4 30.8 13 41.9
0.723 1.625
0.410
to
6.449
>40 years 9 69.2 18 58.1
Total 13 100 43 100
Table 2: Effect of gender in medicine status.
Gender
Status Treatment
P OR 95% Cl Case Control
n % n %
Male 8 61.5 20 64.5
1,000 1.136 0.298 to 0.693 Female 5 38.5 11 35.5
Total 13 100 31 100
ICOSOP 3 2019 - International Conference on Social Political Development (ICOSOP) 3
214
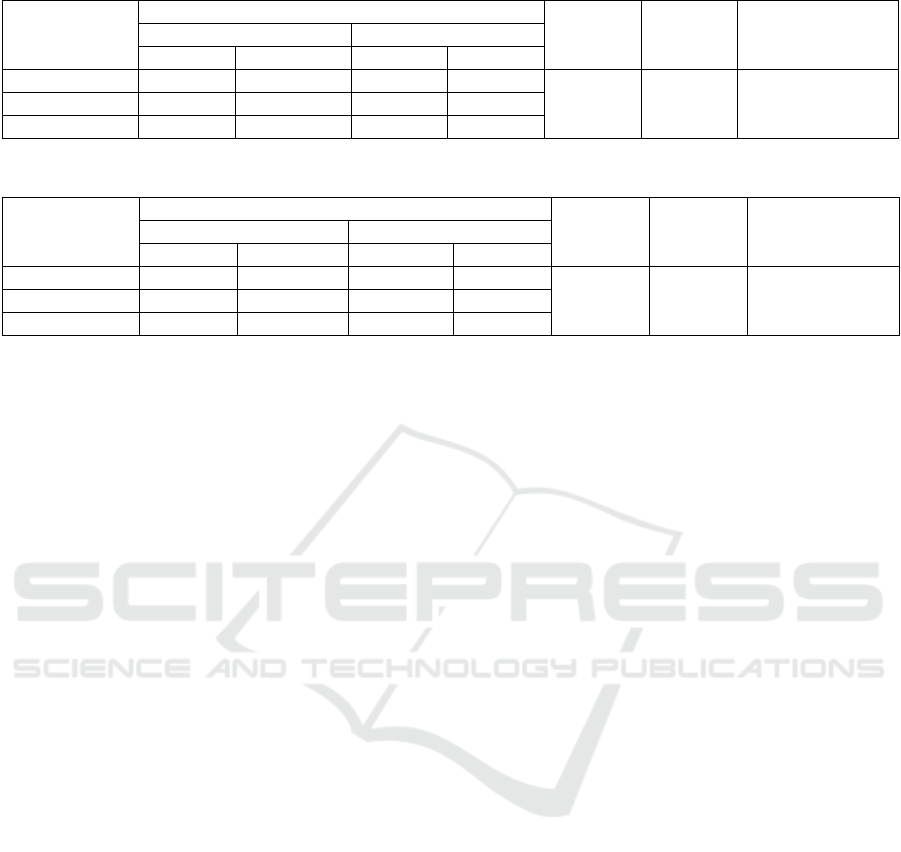
Table 3: Effect of education with treatment status.
Education
Status Treatment
P OR 95%Cl
Case Control
n % n %
Low 5 38.5 14 45.2
0.940 1,318 0.351 to 4.945 High 8 61.5 17 54.8
Total 13 100 33 100
Table 4: Effect of work by status of respondents.
Occupation
Status Treatment
P OR 95%Cl Case Control
n % n %
Not Employed 9 69.2 19 61.3
0.738
0.704
0.177-2.802
Employed 4 30.8 12 38.7
Total 13 100 31 100
3.3 Effect of Education with TB-RO
According to the Table 3, the proportion of
respondents with low education in case group as
much as 38.5%, lower than in the control group as
much as 45.2%. While the highly educated
respondents in the case group as much as 61.5%, the
rate is higher than in the control group as much as
54.8%. Results using chi-square analysis showed
that there is no influence of this research study with
TB-RO treatment status (p = 0.940> 0.05). Value
OR = 1.318, indicating the status of TB treatment
RO 1.3 times the tendency to occur in less educated
respondents compared educated.
This study is in line with Rusman and Basri
(2019) in the Health Center Indramayu Jatisawit
obtained p = 0.082 which means there is no
influence of education with pulmonary TB
treatment. According to Green, education is a major
factor forming behavior. OAT adherence is one of
the behaviors that can be assessed by both
observation and recall. In general, the higher a
person's education, the better their behavior
(Notoadmojo, 2010). The results of the above cross-
tabulation obtained by those who have not started
treatment was higher in the lower than the higher
education, so the results prove that education is not a
determinant of treatment TB-RO.
3.4 The influence of Jobs with TB-RO
Based on Table 4 the proportion who do not work in
the case group as much as 69,2% and in the control
group that did not work as much as 61.3%, while the
proportion of respondents who worked in the group
amounted to 30.8% of cases and the control group
by 38.7% Results of analysis using the chi square
indicates that there is no influence of this research
work to the status of TB-RO treatment (p = 0.520>
0.05). Value OR = 0.704, indicating the status of TB
treatment RO0.7 times leanings of respondents did
not work
The study is in line with research of Yusi, et al.
(2018) in Semarang obtained value of p = 0.995,
which means there is no influence between work and
determinants of treatment. Backed by research
Kuchukhidze et al. in Geogia, USA (2014) obtained
the value p = 0:11, which means there is no effect of
treatment status job.
In this case, the type of risky work that can cause
a person to be exposed to substances that can
interfere with lung function and possible work is that
someone has direct contact with a TB patient.
Traders and workers are more likely to have poor
TB treatment outcomes because traders and workers
have longer working hours and there are no definite
time limits. So it is possible to have a less
permissive attitude to start TB treatment and get less
support to start treatment from the surrounding
environment as a stimulus to increase patient
motivation in achieving healing and successful
treatment. However, it is different from the results of
research respondents who do not work have a higher
proportion of not starting treatment than those who
work, this is because respondents who used to work
are no longer able to work because of the pain
experienced.
3.5 Influence of Income with TB-RO
According to the Table 5, the proportion of income
in the case group 100% of low-income, whereas in
the control group at 93.5% low income and low
income of 6.5%. Results using chi-square analysis
Determinants of TB-RO Affecting Confirmation Have Not Started the Treatment
215

showed that it contained no significant effect
between age and treatment of TB-RO status (p =
1.000> 0.05). Value OR = -20.40, indicating the
status of TB treatment RO 1.3 times the tendency to
occur in low income compared high income.
Not meaningless variable revenue due for 100%
of the cases and more than 90% in the control to be
the subject of research, have in common is living in
families with low-income economic status UMR.
The similarity in the characteristics of family income
in case and control groups, each group has the
opportunity determinant of treatment.
3.6 Influence Knowledge with TB-RO
Based on the Table 6, the proportion of respondents
who are knowledgeable lower in the case of 6
(31.6%) and a control group of 13 people (68.4%).
While the high knowledgeable respondent group of
7 cases (28.0%) and the control group of 18 people
(72.0%). Results of analysis using the chi-square test
showed that in this study there was no significant
effect between knowledge and RO TB treatment
status (p = 1.000> 0.05). Value OR = 0.843,
indicating the status of TB treatment RO 0.8 times
the tendency to occur at low knowledgeable
respondents compared knowledge.
This study is in line with research Utami, Tunru
and Yusnita (2018) in Johar Baru sub-district health
center in Central Jakarta variable results obtained
knowledge p = 0.069, no effect of the level of
knowledge with the successful treatment of TB-RO.
3.7 Attitudes Influence with TB-RO
Based on the Table 7, the proportion of respondents
whose attitude is not good in the case group of five
people (55.6%) and control by 4 people (44.4%).
While both groups of respondents’ attitude of 8
cases (22.9%) and the control group of 27 people
(77.1%). Results of analysis using the chi-square test
showed that in this study there was no significant
effect between attitude with TB-RO treatment status
(p = 0.098> 0.05). Value OR = 0.237, indicating the
status of TB treatment RO 0.2 times the tendency
occurred on the respondents' attitude is not better
than a good attitude. The study is in line with
Mientarini, Sudarmanto, Hasan (2018) obtained the
value p = 0.321, which means there is no influence
by the gesture with medication adherence.
Differences in the characteristics of respondents
can influence the attitudes of TB patients while
undergoing Trartmen. The factors that influence
attitude is one's knowledge. The higher the person's
knowledge will contribute to the formation of a good
attitude. Attitude formation cannot be separated
from their factor- factors that influence such a
personal experience, culture, others that are
considered important, the mass media, as well as
emotional factors of the individual. It is clear that
the level of acceptance or respondents were
permissive to TB drugs will affect the behavior of
the TB treatment success to be good or vice versa
can be poor. Success to be good or vice versa can be
poor.
Table 5: Effect of income to the status of respondents.
Income
Status Treatment
P OR 95% Cl Case Control
n % n %
Low 13 100 29 93.5
1,000 20.40 0,000
High 0 0 2 6.5
Total 13 100 33 100
Table 6: Effect of income to the status of respondents.
Income
Status Treatment
P OR 95% Cl
Case Control
n % n %
Low 13 100 29 93.5
1,000 20.40 0,000 High 0 0 2 6.5
Total 13 100 33 100
ICOSOP 3 2019 - International Conference on Social Political Development (ICOSOP) 3
216
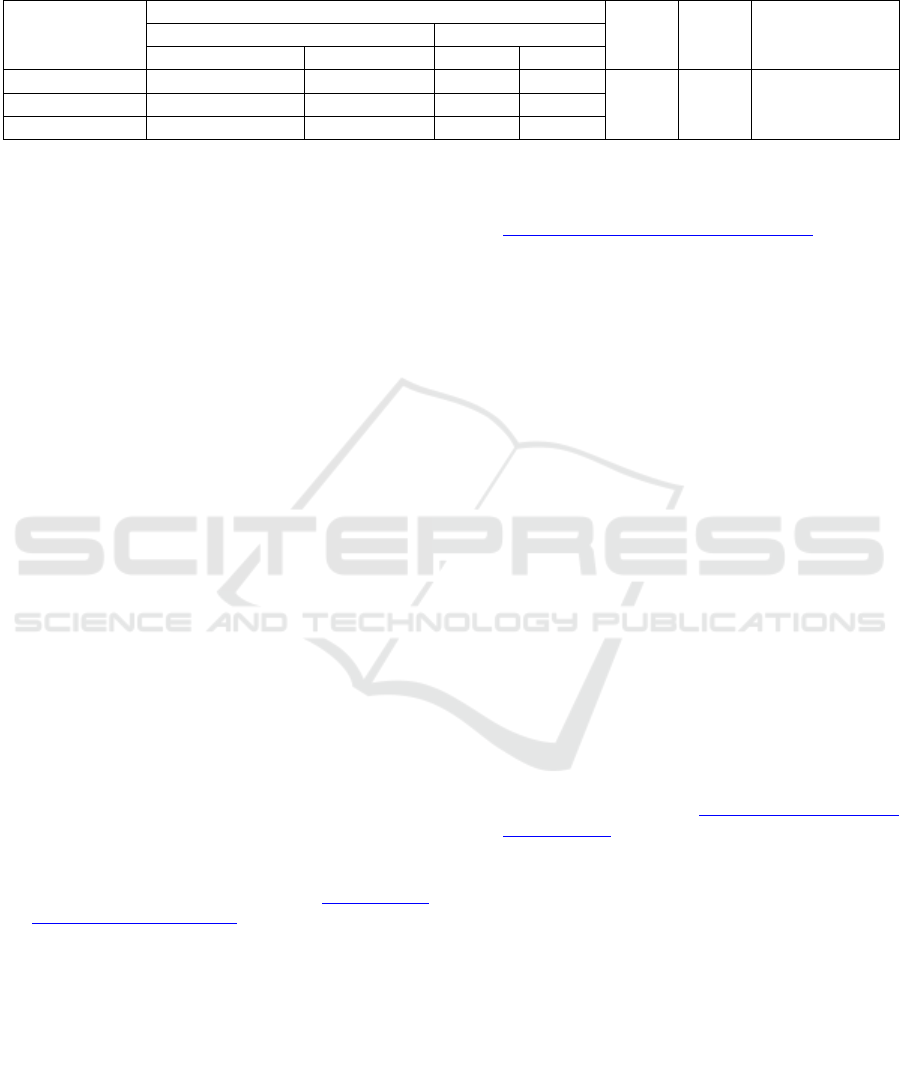
Table 7: Effect of attitude to the status of respondents.
Attitude Status Treatment
P OR 95%Cl Case Control
N % n %
Not Good 5 77.1 4 44.4
0.98 0.237 0.051 to 1.098
Good 8 22.9 27 55.6
Total 13 100 31 100
4 CONCLUSION
No influence of sociodemographic (age, sex,
education, occupation, income), knowledge and
attitude with TB RO Treatment Status.
ACKNOWLEDGMENT
Thank you to the TALENTA Research Institute,
University of North Sumatra for providing research
funding, with contract number: 4167 / UN5.1.R /
PPM / 2019 April 1, 2019.
REFERENCES
Anderson, L.F., Watson J.P., Tamne S., Cohen T., Mitnick
T., Drobniewski F., Abubakar, I., 2013. Treatment
outcome of multi-drug resistant tuberculosis in the
United Kingdom: Retrospective prospective cohort
study from 2004 to 2007. European Surveillance,
18(40), 1-10.
Burhan, 2010. Tuberculosis Multi Drug Resistance (TB
Resistan Obat), Majalah Kedokteran Indonesia,
60(12), 535-536.
Desissa, F., Workineh T., Beyene, 2018. Risk factors for
the occurrence of multidrug-resistant tuberculosis
among patients undergoing multidrug-resistant
tuberculosis treatment in East Shoa, Ethiopia.BMC
Public Health, 18(422). Retrieved from https://doi.org/
10.1186/s12889-018-5371-3
Dinas Kesehatan Provinsi Sumatera Utara, 2018.
Kebijakan Program Pengendalian TBC Provinsi
Sumatera Utara. Medan.
Kemenkes RI, 2011. Rencana aksi nasional public private
mix pengendalian tuberkulosis Indonesia: 2011-2014.
Direktorat Jenderal Pengendalian Penyakit dan
Penyehatan Lingkungan. Jakarta.
Kuchukhidze, G, Kumar A.M.V., de Colombani P.,
Khogali M., Nanava, Blumberg H.M., 2014. Sort it
supplement: TB in eastern Europe, 2012-2014: Risk
factors associated with loss to follow-up among
multidrug-resistant tuberculosis patients in Gorgia,
Public Health Action, 4(2): 541-546. Retrieved from
https://dx.doi.org/10.5588%2Fpha.14.0048
Mientarini., E.I., Sudarmanto., Y., Hasan, M., 2018.
Hubungan pengetahuan dan sikap terhadap kepatuhan
minum obat pasien tuberkulosis paru fase lanjutan di
Kecamatan Umbulsari Jember. IKESMA, 14(1).
Retrieved from http://garuda.ristekdikti.go.id/
documents/detail/981090
Notoatmojo, S., 2010. Promosi kesehatan dan ilmu
perilaku, Rineka Cipta. Jakarta.
Rusman, B., 2019. Faktor yang mempengaruhi penderita
TB paru terhadap kepatuhan minum obat anti
tuberkulosis di puskesmas jatisawit Indramayu, Afiasi:
Jurnal Kesehatan Masyarakat, 4(1). Retrieved from
DOI: 10.31943/afiasi.v4i1.10
Utami, N., Tunru, I., Yusnita, 2018. Hubungan tingkat
pengetahuan terhadap keberhasilan pengobatan
tuberkulosis di puskesmas Kecamatan Johar Baru
Jakarta Pusat tahun 2016. Jurnal Kedokteran dan
Kesehatan, 2(12). Retrieved from DOI:
10.33533/jpm.v12i2.262
Wulandari, D.H., 2015. Analisis faktor-faktor yang
berhubungan dengan kepatuhan pasien tuberkulosis
paru tahap lanjutan untuk minum obat di rs rumah
sehat terpadu tahun 2015. Jurnal Administrasi Rumah
Sakit, 2(1).
Yusi, N., Widagdo, L., Cahyo, K., 2018. Analisis
hubungan dukungan psikososial dengan perilaku
keberhasilan pengobatan tb di Kota Semarang, JKM,
6(5). Retrieved from http://ejournal3.undip.ac.id/
index.php/j km
Determinants of TB-RO Affecting Confirmation Have Not Started the Treatment
217
