
Hypertension and Type 2 Diabetic Mellitus in the Middle-ages
Persons
Ade Heryana
1
, Intam Silviana Mustikawati
1
, Prima Darma Bekti
2
and Iin Desmiany Duri
3
1
Faculty of Health Sciences,Esa Unggul University
2
Public Health Department, Respati Indonesia University
3
Faculty of Public Health, Diponegoro University
Keywords: Type-2 Diabetic Mellitus, Risk Factors, Hypertension, Chronic Disease, Middle-ages
Abstract: Type-2 Diabetic Mellitus (NIDDM) is a chronic disease that glucose blood level elevated significantly
without dependency to insulin level. Diabetes gave medical and non-medical impacts for patients if
adequacy prevention was not arranged. Sedentary lifestyle made a significant positive trend to the
prevalence of diabetes. This study is a quantitative analytic investigated association between type-2 DM
with age and hypertension. Total of 680 health records from primary health service involved with
systematic random sampling. This study provided significance association between age and type-2 DM (OR
= 5.859), hypertension and type-2 diabetes (OR = 4.173) and age and hypertension (OR = 3.081).
Conclusion: people above or at 45 years old should be aware of the risk of hypertension that a gateway to
type-2 diabetes. They should routinely control blood pressure and modify healthy lifestyle to prevent
hypertension and type-2 diabetic mellitus.
1 INTRODUCTION
Diabetes Mellitus (DM or diabetes) is a group of
disease primarily characterized by chronic
hyperglycemia due to a lack of sufficient insulin
action (American Diabetes Association, 2014;
Nowotny et al., 2015; Areosa et al., 2017). One type
of DM is type 2 Diabetes or Noninsulin-Dependent
Diabetes (NIDM) is called adult-onset diabetes,
although there is tend to suffer among overweight
children (Sone, 2018).
The condition of diabetes will cause chronic
complications in various organs of the body if there
is no adequate treatment. The chronic compilations
are 1) stroke, in the cerebral blood vessels; 2)
blindness, in the blood vessels of the eye; 3)
coronary heart disease, in the heart blood vessels; 4)
chronic kidney disease, in the kidney blood vessels;
and 5) wounds difficult to heal, in the leg veins
(Waspadji, 2011; Huang et al., 2014; Sjöström et al.,
2014; Mostafa et al., 2018). This complication
definitely will reduce employee work productivity
for the productive age group.
There is an elevated level of prevalence of
diabetes in 2013 (diagnosed by doctors or
symptoms) compared to 2007 in the age group ≥ 15
years. In 2007 the prevalence of diabetes was 1.1%
while in 2013 it was 2.1% throughout Indonesia.
Prevalence of diabetes in Indonesia diagnosed by
doctors was 1.5% in 2013(Balitbangkes Kemenkes
RI, 2013). Diabetes Care Report projected the
prevalence of diabetes in Indonesia in 2030 is about
21.3 million peoples (Puskom Publik Kemenkes RI,
2009).
Hypertension or high blood pressure is a
condition where a person's blood pressure against
the arterial wall is consistently high, when the heart
contracted (systolic) greater than 140 mmHg and
when the heart weakened (diastolic) greater than or
equal to 90 mmHg (Boslaugh, 2008).This is a
chronic condition that could lead to heart disease,
stroke, and other diseases that can result in
premature death (Kung and Xu, 2015). Most of the
disease burden caused by high blood pressure is
borne by low-income and middle-income countries,
by people in middle age, and by people with
prehypertension. Prevention and treatment strategies
restricted to individuals with hypertension will miss
a much blood-pressure-related disease (Lawes et al.,
2008). RISKESDAS 2013 reported that the
prevalence of hypertension is 26.5% among peoples
≥ 18 years old. It is declined compared to the
Heryana, A., Silviana Mustikawati, I., Darma Bekti, P. and Desmiany Duri, I.
Hypertension and Type 2 Diabetic Mellitus in the Middle-ages Persons.
DOI: 10.5220/0009951430013007
In Proceedings of the 1st International Conference on Recent Innovations (ICRI 2018), pages 3001-3007
ISBN: 978-989-758-458-9
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
3001

prevalence in 2007,i.e. 31.7% (Balitbangkes
Kemenkes RI, 2013).
Arterial hypertension reported came upon a two-
third person with type 2 diabetes. Hypertension
increases the incidence of both micros- and
macrovascular complications. A person with
hypertension and type 2 diabetes leads to four-
foldincreased risk for cardiovascular disease (CVD)
compare to type 2 diabetes with normal tension
(Pavlou et al., 2018). The inaccuracy of salt and
water storage and the elevated of pressure from the
body in the peripheral blood circulation caused of
blood pressure closely related to insulin resistance as
the originator of the incidence of diabetes (Fatimah,
2015).
Hypertension strongly associated with the risk of
developing type 2 diabetes mellitus, as well as a
significant predictor of the incidence of
nephropathy, retinopathy, and cardiovascular disease
that accompanies DM. A study conducted in Osaka
(Osaka Health Survey), the relative risk of the
development of type 2 diabetes mellitus was 1.76 in
hypertensive men compared to 1.39 in normal
tension men. The incidence of hypertension is
increased in patients with 1.5 to 3 times diabetes
compared to normal patients. A study shows 40% of
people with diabetes experienced hypertension at 45
years old, and more than 60% at the 60 years old
(Cordario, 2005).
Diabetes risk factors due to hypertension in the
18 and above years old population reached 25.8%
(Ministry of Health, 2014). In general, the
proportion of people with diabetes who suffer from
hypertension is almost the same (Soewondo and
Pramono, 2011). The association of diabetes and
hypertension study in Indonesia showed that A
significant relationship between blood pressure and
the incidence of diabetes with odd ratio 6.85 times
compared to people with normal blood pressure
(Trisnawati and Setyorogo, 2013). There was a
significant relationship between hypertension and
the incidence of diabetes, with the risk of diabetes in
the group who had a higher history of hypertension
than the group with the normal tension of 3.41 times.
Hypertension and diabetes are interconnected risk
factors (Nainggolan et al., 2013).
The term “age” according to WHO is the amount
of time a person has gone through to date by
calculating the day/date of birth as zero. Humans
generally experienced a faster physiological decline
at 40 years old, and diabetes is more common at
above 40 years old (Yuliasih and Wirawanni, 2009).
In (Cho et al., 2018) state the prevalence of diabetes
8% (peaked) in the low-income countries among the
55-64 age group.
Some study in Indonesia showed the relationship
between age and diabetes. Indonesian mostly
suffered diabetes at the 38-47 years old with a
proportion of 25.3%. The risk of DM increases
gradually according to the development of age
(Soewondo and Pramono, 2011), the older had
tendency to suffer from diabetes and the group of
55-64 years old had a 14 times risk of diabetes
compared to the 25-34 years old group (Nainggolan
et al., 2013),84% of diabetes cases could be
prevented by taking into account age risk factors,
and the probability of diabetes occurring at below 45
years old and at 45 years is around 1 in 6 (Zahtamal
et al., 2007),diabetes risk in the <45 years old group
is 72% lower than the group ≥ 45 years old
(Trisnawati and Setyorogo 2013).
The Hypertension report by the World Health
Organization states that aging is one of the main
factors that contribute to the development of high
blood pressure and its complications (World Health
Organization, 2013).
The risk of hypertension higher with the
increasing of person’s life stages (Rahajeng and
Tuminah, 2009). Several studies in Indonesia is
proventhe association between age and
hypertension. Study at Public Health Careshowed
that there is an association between age and
hypertension with risk 13,34 times to peoples > 30
years old (Mutmainah and Heryana, 2017).Study at
rural community showed that peoples ≥ 31 years old
3,76 times likely to hypertension than others
(Yogaswara and Heryana, 2018).
2 RESEARCH METHOD
This study held in Cempaka Putih public health
service district that we called “Puskesmas Cempaka
Putih.” Type 2 diabetes is a 3
rd
rank disease at
Puskesmas Cempaka Putih with the incidence
increased from 2014 to 2015. In 2014 the cases of
type 2 DM patients reached 2,022 while in 2015
increased to 2,446. Thus according to the whole
population in 2012, the prevalence of type 2 DM in
2015 is about 2.67%.
The objective of this study is to proof (1) the
association between age with type 2 DM and
hypertension; and (2) the association between age
and hypertension. From several studies we state the
model age-DM-hypertension as follow:
ICRI 2018 - International Conference Recent Innovation
3002
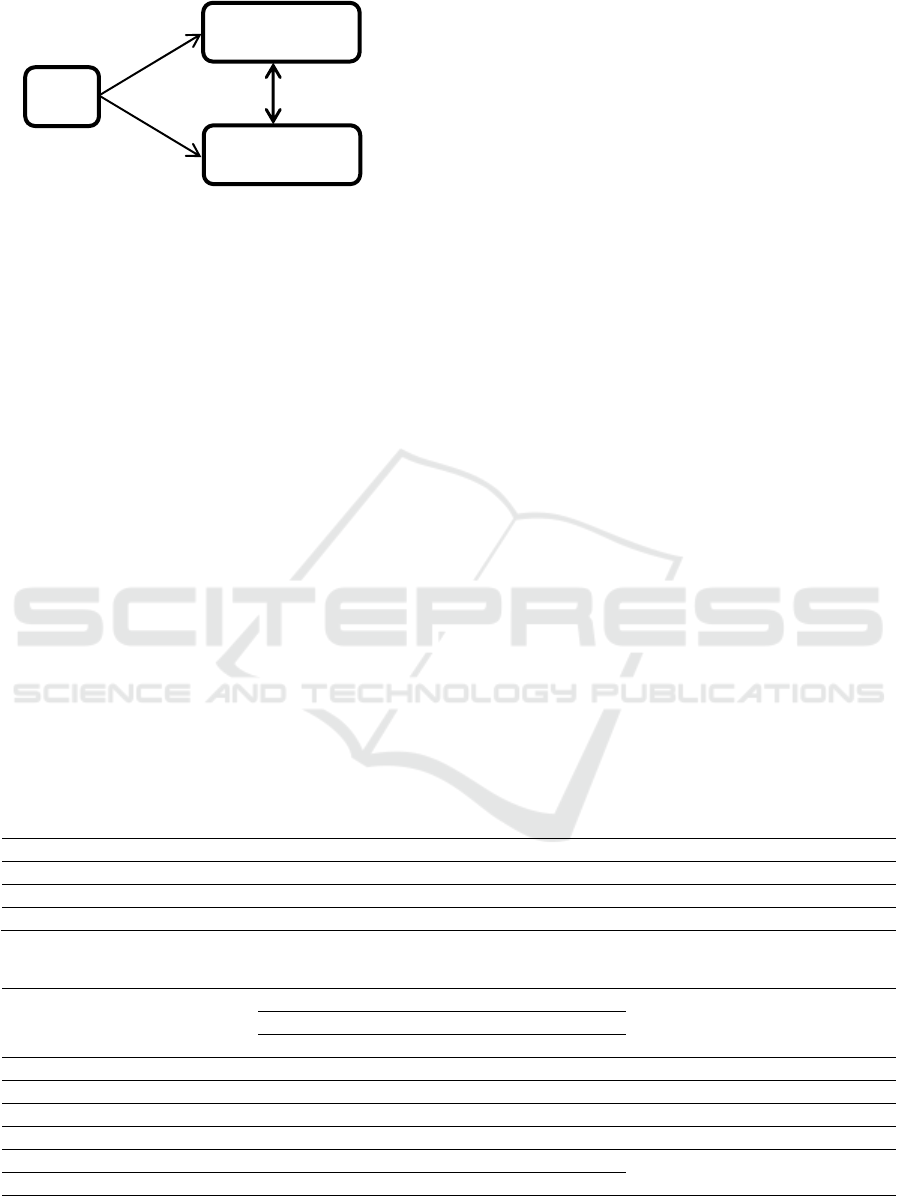
Figure 1: Age-Diabetes-Hypertension Model
We propose three hypothetical testing: positive
association between age and hypertension, positive
association between age and type-2 diabetes; and
positive association between hypertension and type-
2 diabetes (see Figure 1).We defined: (1) Type 2
diabetes is a condition of hyperglycemia in patients
that is stated with a doctor's diagnosis or ICD-X
code on a health record; (2) Hypertension is blood
pressure at the time of the study based on medical
record. Measurement classified by (1) Hypertension
if hystolic blood pressure ≥ 140 mmHg and or
systolic blood pressure ≥ 90 mmHg; and (2) Normal
tension if hystolic blood pressure <140 mmHg and
or systolic blood pressure <90 mmHg; and (3) Age
is the period of the respondent at the time of the
study which is known from the health records data.
The measurement classified into (1) Risk, if age ≥
45 years old; and (2) Not at risk, if the age is <45
years old.
Case-Control design held for the association
between type-2 diabetes and age/hypertension, and
Cross-sectional design for the association between
age and hypertension. Cases group was people with
diabetes mellitus ≥ 15 years old during 2016-2017
who were obtained from the healthrecord, while
Control group was patients ≥ 15 years old who
visitedgeneral medical service thatwere not type 2
diabetes diagnosed by a medical doctor. The
population were all of the patients visited general
medical service in 1 year period,it isabout 2.540
peoples in 2016. Total of 680 sample size counted
with Hypothesis Test for the Odds Ratio methods,
obtained 340Case and 340 Control group.Systematic
randomsampling was carried out to this study.
Inclusion criteria are above 15 years old, no barrier
in communication, and willing to be a respondent.
Exclusion if pregnant women and in illness
condition.
3 RESULTS
Table 1 showed that the mean of systolic blood
pressure is 120.4 mmHg (CI 95% : 119.1 – 121.6
mmHg), with a range from 80 to 200 mmHg.
Diastolic blood pressure’s mean is 78.7 mmHg (CI
95% = 78.1 – 79.4 mmHg), with range from 30 to
110 mmHg. The range of age from 16-74 years with
the mean 45.5 (CI 95% = 44.7 – 46.3 years).
Table 2 showed that 313 participants (55.6%)
diabetesin hypertension condition, and 90
participants (76.9%) non type-2 diabetes in normal
tension, there is a significant association with risk
4.173 times likely suffering type-2 DM for
hypertension participants.
Table 1: Age and Blood pressure Profiles (N=680)
No Characteristics Mean CI95% SD SE Min Max
1 Systolic blood pressure 120.4 119.1 – 121.6 16.9 0.647 80 200
2 Diastolic blood pressure 78.7 78.1 – 79.4 9.0 0.346 30 110
3 Age 45.5 44.7 – 46.3 10.8 0.413 16 74
Table 2: Association between Type-2 DM with Hypertension and Age (N=680)
No Independent variables
Type-2 Diabetic Mellitus
p-value Odds Ratio (CI 95%) Case (+) Control (-) Total
Freq. % Freq. % Freq. %
1 Blood pressure
Hypertension 313 55.6 250 44.4 563 100.0 0.000 4.173 (2.589 – 6.880)
Normal tension 27 23.1 90 76.9 117 100.0
2 Age
≥ 45 years old 199 75.1 66 24.9 265 100.0
0.000 5.859 (4.096 – 8.406)
< 45 years old 141 34.0 274 66.0 415 100.0
Age
Hypertension
Type 2 DM
Hypertension and Type 2 Diabetic Mellitus in the Middle-ages Persons
3003
Table 3: Association between Age with Hypertension (N=680)
No Age
Blood Pressure
p-value Odds Ratio (CI 95%)
Hypertension Normal Total
Freq. % Freq. % Freq. %
1 ≥ 45 years old 94 22.7 321 77.3 415 100.0 0.000 3.081 (1.868 – 5.245)
2 < 45 years old 23 8.7 241 91.3 265 100.0
Table 2 also showed that 199 participants
(75.1%) with type-2 DM were above and at 45 years
old. Otherwise, 241 participants (91.3%) non type-2
DM were below 45 years old. Thisresults proof that
age and type-2 DM had a significant association,
with risk 5.859 times likely suffering type-2 DM for
participants above and at 45 years old compared to
below 45 years old.
In another analysis, Table 3 showed that 94
participants (22.7%) above and at 45 years old had
hypertension. Otherwise,241 participants (76.9%)
below 45 years oldhad normal tension. Thisresults
proof that age and hypertension had a significant
association, with risk 3.081 times likely suffering
hypertension for participants above and at 45 years
oldcompared to below 45 years old participants.
4 DISCUSSION
4.1 High Blood Pressure and Diabetic
Mellitus
This study provided that The mean of systolic blood
pressure is 120.4 mmHg (95 CI = 119.1 – 121.6
mmHg) and diastolic is 78.7 (78.1 – 79.4),
hypertension has a significant association with type
2 diabetes mellitus. This result linear with other
hypertension studies.
According to Joint National Committee Report,
participants in this study on average have a normal
tension both systolic and diastolic, but if we look the
maximum value, there are some participants in stage
2 hypertension. JNC VII stated that normal tension if
systolic < 120 mmHg and diastolic and< 80 mmHg
(National Institute of Health, 2004). It isimportant
for the authority of the health system to take action
in controlling blood pressure especially to peoples
above 45 and at years old.
Early detection of blood pressure is an effective
intervention and treatment to prevent hypertension
and more impact of cumulative cardiovascular risk
(Volpe et al., 2018). Furthermore this healthy action
effective in the association with diabetes risk factors.
Unfortunately, this healthy behavior is rarely seen in
our community. This condition includes the
prevention of hypertension with decreasing risk
factors and routine blood pressure control.
Blood pressure controlling in Indonesia showed
that only 18% of hypertension participants were
under control (Herwati and Sartika, 2013). Maharani
and Syafrandi (2017) reported that 60% of
hypertension persons had unhealthy behavior in
controlling blood pressure. This study proofed that
people’s awareness of the importance of routinely
blood pressure control already in low level,
especially among people with high-risk factors.
For persons who are suffering diabetes should
manage and control hypertensionshould be ˂ 130/85
mmHg (Niakan and Cushman, 2018). In (Grenier et
al., 2018) only about one-third of patients with
diabetes achieved the target blood pressure below
130/80 mmHg. Patients with blood pressure ≥
130/80 mmHg were also less likely to achieve
optimal guideline-recommended glycated
hemoglobin and low-density lipoprotein-cholesterol
targets. Improved comprehensive management of all
risk factors in patients with diabetes is warranted.
The empowerment of older health integrated unit
and chronic disease control program at public health
care in Indonesia is a useful intervention to promote
controlling blood pressure. It is the cross-section
tasks that public healthcare has to collaborate with
all stakeholders.
4.2 Association between Age and
Diabetes and Hypertension
This study provided that age has a significant
association with type 2 diabetes and hypertension.
This result linear with other studies. Middle-ages is
human life stages that decline some organ function
(Knopman et al., 2001). It isimportant for the
authority of health system to promote
healthylifestyle among ≥ 45 age group, especially
for the older group. IDF predicted by 2050 the
proportion of older people in the population will
increase from 15% to 25%. Itis led to the prevalence
of type 2 diabetes in older people,andunfortunately,
the management of diabetes for this group is not
easy(Colagiuri et al., 2014).
ICRI 2018 - International Conference Recent Innovation
3004

One of national levelhealth program that aids
action to prevent hypertension and diabetes at
middle-ages is “Prolanis”.Since 2014 Prolanis is
health programdirected by primary health care and
supervised by national health insurance to maintain
the healthy condition of NHI member that suffering
chronic disease. “Prolanis” aims to reach optimal
quality of life with effective and efficient in service
cost(BPJS Kesehatan, 2014).
Prolanistargeted for peoples who registered as
NHI members (BPJS Kesehatan, 2014). Study
conducted at one of primary health care in Indonesia
showed that the members of Prolanis largely women,
above 45 years old, had lower education,
unemployment, and had obesity condition. Most of
members are disobedient to routinely implement the
education of this program and physical activity and
had unstable glucose level in blood.The obedient to
implement Prolanis associated with stability of
glucose level in blood(Primahuda and Sujianto,
2016).It is suggested that Prolanis program should be
empower by all stakeholders in diabetes prevention
Prolanis is an appropriate way to increase health
statue for people who above or at 45 years old.
Prevalence of hypertension in elderly higher than
adult, wich is most of primary hypertension and
isolated systolic hypertension. Hypetension
management in elderly basically similar with adult, it
is included life-style modification and
pharmacotherapy intervention. Several life-style
should be improved are decreasing body weight if
obesity or overweight, restricted to alcohol, pyshical
activity, low salt intake, adequate potasiumand
magnesium intake, stop smoking, and decreasing
intake of saturated fat and cholesterol (Kuswardhani,
2006).
Some of foods and beverages should avoid to
prevent hypertension include: high level of
saturated-fat, process with natrium salt, Cans
food/drink, preserved meal, full cream milk,
margarine, mayonnaise, eggs, seasonings with high
natrium, alcohol, and alcohol contained food like
durian (Kemenkes RI, 2014).
Theaction of hypertension intervention above
should undertake with others activity to prevent
diabetes. In (Chatterjee et al., 2017) prevention of
type 2 diabetes should attempted with widespread
national prevention programmes. Prolanis is the
right intervention for controlling prevalence of
hypertension and diabetes focus on middle-aged.
5 CONCLUSIONS
This study provided significance association
between age and type-2 DM (OR = 5.859),
hypertension and type-2 DM (OR = 4.173) and age
and hypertension (OR = 3.081). People above or at
45 years old should be aware with the risk of
hypertension that a gateway to type-2 diabetes. They
should routinely control blood pressure and modify
healthy life-style to prevent hypertension and type-2
diabetic mellitus. Primary health care should
intensively arrange “Prolanis” program that
supervised by National Health Insurance.
ACKNOWLEDGEMENTS
We thanks to staff of Puskesmas Cempaka Putih that
accompanied this study and Professor Bacharudin
Lapau to supervised progress of research.
REFERENCES
Areosa, A. S., Vernooij, R. W., González-Colaço, M. H.,
and Martínez, G. (2017). Effect of the treatment of
Type 2 diabetes mellitus on the development of
cognitive impairment and dementia. Cochrane Library.
John Wiley & Sons, Ltd. Available at:
https://www.journalslibrary.nihr.ac.uk/downloads/othe
r-nihr-research/cochrane-programme-
grants/Effect%20of%20the%20treatment%20of%20T
ype%202%20diabetesmellitus%20on%20the.pdf
American Diabetes Association. (2014). Diagnosis and
Classification of Diabetes Mellitus. Diabetes Care,
37(1): S81-S90.
Balitbangkes Kemenkes RI. (2013). Riset Kesehatan
Dasar: RISKESDAS 2013. Laporan Nasional 2013.
Jakarta: Kementerian Kesehatan RI. https://doi.org/1
Desember 2013
Boslaugh, S. (2008). Hypertension. In Encyclopedia of
Epidemiology 1&2 (p. 513). SAGE Publications.
BPJS Kesehatan. (2014). Panduan praktis PROLANIS
(Program pengelolaan penyakit kronis). BPJS
Kesehatan. Jakarta: BPJS Kesehatan.
Chatterjee, S., Khunti, K., and Davies, M. J. (2017). Type
2 diabetes. The Lancet. https://doi.org/10.1016/S0140-
6736(17)30058-2
Cho, N. H., Shaw, J. E., Karuranga, S., Huang, Y., da
Rocha Fernandes, J. D., Ohlrogge, A. W., and
Malanda, B. (2018). IDF Diabetes Atlas: Global
estimates of diabetes prevalence for 2017 and
projections for 2045. Diabetes Research and Clinical
Practice, I(38): 271–281.
Colagiuri, S., Cho, N. H., Distiller, L., Dong, B., Duning,
T., Gadsby, R., … Sinay, I. (2014). The IDF global
Hypertension and Type 2 Diabetic Mellitus in the Middle-ages Persons
3005

guideline for managing older people with type 2
diabetes. Journal of Diabetes Nursing.
https://doi.org/10.1016/j.diabres.2014.03.005
Cordario, R. A. (2005). Type-2 Diabetes, Prediabetes, and
the Metabolic Syndrome: The Primary Care Guide to
Diagnosis and Management. New Jersey: Humana
Press.
Fatimah, R. N. (2015). Diabetes Melitus Tipe 2. Majority,
4(5): 93–101. https://doi.org/10.2337/dc12-0698
Grenier, J., Goodman, S. G., Leiter, L. A., Langer, A.,
Teoh, H., Bhatt, D. L., … Yan, A. T. (2018). Blood
Pressure Management in Adults With Type 2
Diabetes: Insights From the Diabetes Mellitus Status
in Canada (DM-SCAN) Survey. Canadian Journal of
Diabetes, 42(2): 130–137.
https://doi.org/10.1016/j.jcjd.2017.01.005
Herwati, H., and Sartika, W. (2013). Terkontrolnya
Tekanan Darah Penderita Hipertensi Berdasarkan Pola
Diet Dan Kebiasaan Olahraga Di Padang Tahun 2011.
Andalas Jorunal of Public Health, 8(1): 8–14.
Huang, E. S., Laiteerapong, N., Liu, J. Y., John, P. M.,
Moffet, H. H., and Karter, A. J. (2014). Rates of
complications and mortality in older patients with
diabetes mellitus: the diabetes and aging study. JAMA
internal medicine, 174(2): 251-258.
Kemenkes RI, P. (2014). Hipertensi. Infodatin. Jakarta.
https://doi.org/10.1177/109019817400200403
Knopman, D., Boland, L. L., Mosley, T., Howard, G.,
Liao, D., Szklo, M., … Folsom, A. R. (2001).
Cardiovascular risk factors and cognitive decline in
middle-aged adults. Neurology, 1(2): 42–48.
https://doi.org/10.1212/WNL.56.1.42
Kung, H. C., and Xu, J. (2015). Hypertension-related
Mortality in the United States, 2000-2013. NCHS data
brief, (193): 1-8.
Kuswardhani, T. (2006). Penatalaksanaan Hipertensi Pada
Lanjut Usia. Jurnal Penyakit Dalam, 7(2): 135–140.
Lawes, C. M., Hoorn, S. Vander, and Rodgers, A. (2008).
Global burden of blood-pressure-related disease, 2001.
The Lancet, 371(9623): 1513–1518.
https://doi.org/10.1016/S0140-6736(08)60655-8
Maharani, R., and Syafrandi, D. P. (2017). Faktor yang
Berhubungan dengan Perilaku Pengendalian Tekanan
Darah pada Penderita Hipertensi di Puskesmas
Harapan Raya Kota Pekanbaru Tahun 2016.
Kesehatan Komunitas, 3(5): 165–171.
Mostafa, S. A., Coleman, R. L., Agbaje, O. F., Gray, A.
M., Holman, R. R., and Bethel, M. A. (2018).
Modelling incremental benefits on complications rates
when targeting lower HbA1c levels in people with
Type 2 diabetes and cardiovascular disease. Diabetic
Medicine, 35(1): 72-77.
Mutmainah, N., and Heryana, A. (2017). Faktor-faktor
Risiko yang Berhubungan dengan Kejadian Hipertensi
pada Pasien di Puskesmas Kecamatan Kembangan
Tahun 2017. Universitas Esa Unggul.
Nainggolan, O., Kristanto, A. Y., and Edison, H. (2013).
Determinan Diabetes Melitus Analisis Baseline Data
Studi Kohort Penyakit Tidak Menular Bogor 2011.
Buletin Penelitian Kesehatan, 16(3 Juli 2013): 331–
339.
National Institute of Health. (2004). The Seventh Report of
the Joint National Comittee on Prevention, Detection,
Evaluation, and Treatment of High Blood Pressure.
Niakan, A., and Cushman, W. C. (2018). Hypertension
and Diabetes. In Encyclopedia of Endocrine Disease
(pp. 1–6). Elsevier.
Nowotny, K., Jung, T., Höhn, A., Weber, D., and Grune,
T. (2015). Advanced glycation end products and
oxidative stress in type 2 diabetes mellitus.
Biomolecules, 5(1): 194-222.
Pavlou, D. I., Paschou, S. A., Anagnostis, P., Spartalis,
M., Spartalis, E., Vryonidou, A., … Siasos, G. (2018).
Hypertension in Patients with Type 2 Diabetes
Mellitus: Targets and Management. Maturitas, 112:
71–77.
Primahuda, A., and Sujianto, U. (2016). Hubungan Antara
Kepatuhan Mengikuti Program Pengelolaan Penyakit
Kronis (PROLANIS) BPJS Dengan Stabilitas Gula
Darah Pada Penderita Diabetes Melitus Di Puskesmas
Babat Kabupaten Lamongan. Jurnal Jurusan
Keperawatan, 1–8. Retrieved from
http://eprints.undip.ac.id/49908/
Puskom Publik Kemenkes RI. (2009). Tahun 2030
Prevalensi Diabetes Melitus Di Indonesia Mencapai
21,3 Juta Orang. Retrieved August 26, 2018, from
http://www.depkes.go.id/article/view/414/tahun-2030-
prevalensi-diabetes-melitus-di-indonesia-mencapai-
213-juta-orang.html
Rahajeng, E., and Tuminah, S. (2009). Prevalensi
Hipertensi dan Determinannya di Indonesia. Majalah
Kedokteran Indonesia, 59(12): 580–587.
Sjöström, L., Peltonen, M., Jacobson, P., Ahlin, S.,
Andersson-Assarsson, J., Anveden, Å., ... and
Näslund, I. (2014). Association of bariatric surgery
with long-term remission of type 2 diabetes and with
microvascular and macrovascular complications.
Jama, 311(22): 2297-2304.
Soewondo, P., and Pramono, L. a. (2011). Prevalence,
characteristics, and predictors of pre-diabetes in
Indonesia. Medical Journal of Indonesia, 20(4): 283–
294. https://doi.org/10.13181/mji.v20i4.465
Sone, H. (2018). Diabetes Mellitus. In Encyclopedia of
Cardiovascular Research and Medicine (pp. 9–16).
Elsevier.
Trisnawati, S. K., and Setyorogo, S. (2013). Faktor Risiko
Kejadian Diabetes Melitus Tipe II Di Puskesmas
Kecamatan Cengkareng Jakarta Barat Tahun 2012.
Jurnal Ilmiah Kesehatan, 5(1): 6–11.
Volpe, M., Gallo, G., and Tocci, G. (2018). Is Early and
Fast Blood Pressure Control Important in
Hypertension Management? International Journal of
Cardiology, 254: 328–332.
Waspadji, S. (2011). Diabetes Melitus: Penyulit Kronik
dan Pencegahannya. In S. Soegondo, P. Soewondo;, &
I. Subekti (Eds.), Penatalaksanaan Diabetes Melitus
Terpadu (FK Univers). Jakarta.
ICRI 2018 - International Conference Recent Innovation
3006

World Health Organization. (2013). A Global Brief on
Hypertension: Silent Killer, Global Public Health
Crisis. Geneva, Switzerland.
Yogaswara, Y. M., and Heryana, A. (2018). Faktor-faktor
yang Berhubungan dengan Kejadian Hipertensi di
RT11 Desa Pantai Hurip Kabupaten Bekasi 2018. Esa
Unggul.
Yuliasih, W., and Wirawanni, Y. (2009). Obesitas
Abdominal sebagai Faktor Risiko Peningkatan Kadar
Glukosa Darah. Universitas Diponegoro.
Zahtamal, Z., Chandra, F., Suyanto, S., and Restuastuti, T.
(2007). Faktor-faktor Risiko Pasien Diabetes Melitus.
Berita Kedokteran Masyarakat, 23(3): 142–147.
Hypertension and Type 2 Diabetic Mellitus in the Middle-ages Persons
3007
