
Suspension Claim Health Insurance Hospitalized Due to Incomplete
Medical Record
Agus Sarjono
1
, Endang Ruswanti
3
and Nia Puspita Haspari
4
and Kemala Rita Wahidi
2
1
Master of Management, Esa Unggul University, Jalan Arjuna Utara Number 9, Jakarta, Indonesia
2
Master of Hospital Administration, Esa Unggul University, Jalan Arjuna Utara Number 9, Jakarta, Indonesia
3
Faculty of Economy and Business, EsaUnggul University, Jakarta, Indonesia
4
Faculty of Law, Esa Unggul University, Jakarta, Indonesia
Keywords: Medical records, hospitalized patients, claims, procedures, drugs, identity.
Abstract: This study aims to determine the Influence of Medical RecordCompleteness (Data Identity, Improved Drug
Security and Certainty Procedure) Against Health InsuranceClaim Submission at RS. This type of research
includes an analytic survey with a causality approach. With this research,object data submission claims
patients sampled as many as 98 patients. Sources of data in the form of secondary data based on RS medical
records report of 2017 which is analyzed using Binary Logistic Regression. The results obtained that the
identity of the data significantly influences the submission of claims.Furthermore, the increase in drug
safety significantly affects claim submission,andlastly, the certainty of the procedure significantly affects
claim filing. The findings of researchers of the delay most claims are due to incomplete medical records,
especially data support, filling odontogram, identity data, doctor diagnosis and errors enter thecode.
Implications for hospital management in order to socialize standard operational procedure on completeness
of filling of the medical record to all providers of good care Doctor, nurse, midwife, nutrition,
physiotherapy, Pharmacy.
1 INTRODUCTION
National Health Insurance System (NHI) under
Law no. 40 The year 2004 is a compulsory Social
Health Insurance system in Indonesia. NHI is one of
the programs of the National Social Security System
(SJSN) through the Social Security Administering
Agency claim established on January 1, 2014, as
regulated in Law no. 24 2011. Health insurance that
is comprehensive for every Indonesian people is
realized through NHI program which is a
government program to make the people of
Indonesia can live healthy, productive, and
prosperous. Claim aims to realize the
implementation of ensuring the basic needs of
decent living for each participant or members of his
family. Implementation of the national social
security system based on the principle: 1) mutual
cooperation; 2) non-profit; 3) openness; 4) prudence;
and 5) accountability. (UU BPJS, 2011).
Hospitals as one health service facility have a
role important in achieving the goal of NHI which is
expected to provide efficient, effective, and
demanded services to provide appropriate health
information and produce accurate data in health
services, all of which can not be separated from the
important role of patient medical records. According
to the minister of health regulation, number
269/Menkes/Per/III/ 2008. Concerning Medical
Record is a file containing records and documents
about patient identity, examination, treatment, action
and other services that have been given to the
patient.
Health Insurance claims submissions for patients,
especially for new inpatients will be accepted what
if it meets the various conditions in accordance with
the claim law (2011), namely: 1) SEP (Letter of
Interest of Participants); 2) Inpatient Introduction
Letter; 3) Resume of hospitalization; 4) claim sheet;
5) evidence sheet of inpatient service; 6) receipts
and 7) other supporting results
The completeness of medical record documents
greatly affects the quality of disease statistics and
health problems, as well as in the process of
payment of health costs with INA CBGs software.
Incomplete medical records may indirectly reduce
2994
Sarjono, A., Ruswandi, E., Puspita Haspari, N. and Rita Wahidi, K.
Suspension Claim Health Insurance Hospitalized Due to Incomplete Medical Record.
DOI: 10.5220/0009948829943000
In Proceedings of the 1st International Conference on Recent Innovations (ICRI 2018), pages 2994-3000
ISBN: 978-989-758-458-9
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
the cost of claims based on INA CBGs software.
Based on the results of research Ulfah et al. (2011)
conducted at RSI Sultan Agung Semarang obtained
the result that the importance of medical record data
to smooth approval of Jamkesmas claims. Where Of
9 people with incomplete medical record documents
are all not approved of Jamkesmas claims, and from
the complete medical record records 52.9% are
approved by their Jamkesmas claim
Report from Karawaci Tangerang Hospital in
2016 showed that 8,793 (14.7%) of inpatients from
59,993 patients overall, from 8,793 inpatients there
were 296 (3.4%) patients with incomplete medical
record data. While in 2017 showed an increase in
hospitalized patients to 10,308 of 85,947 patients as
a whole, and from 10,308 inpatients there were 405
(3.9%) patients with incomplete medical record data.
Data at RS. Karawaci Tangerang in 2017 indicates
that the incompleteness of medical records data
mostly occurs at 1) The accuracy of patient identity
(name, medical record number, place of birth date,
sex) that is 37 patients (9%); 2) Increase of drug
safety (proper drug, correct dose, patient right,
proper document, timely and appropriate way of
giving) that is as many as 44 patients (11%); 3)
Certainty of procedure (date and time of action,
result of anamnesa, filling odontogram, diagnosis,
action management plan, physical and supporting
investigation, informed consent) that is 60 patients
(15%).
Also,a source in RS. Karawaci Tangerang 2015
shows hospitalized patients with claims of XYZ
claims 8,855 and 397 (4.4%) of pending claims, this
data increased in 2016 from 8,793 cases filed there
were 408 (4.6 %) claims in pending, as well as in
2017 increased claims in pending up to 445 (4.7%)
of the 9413 submitted cases.
The purpose of this research is to determine the
Influence of Medical Record Complete Patient
Inpatient health Insurance Against Claim
Submission. The contribution of research that is
expected as input for a hospital to improve health
service quality and as an evaluation to hospital
performance related to medical record matter.
The most important research motivation in this
study is the better completeness of RM data so that it
will increase the number of approved health
insurance claims that will ultimately affect the
smooth flow of cash flow and improvement of
health services.But, we have the limitation of this
research: Variable completeness of medical record
in this research is only limited to data identity
variables, drug security improvement and certainty;
This research only covers in Sari Asih Hospital
Karawaci Tangerang only with the number of
respondents is limited, so it is still possible to do
further development with the number of respondents
and research variables more.
2 RESEARCH METHOD
This type of research includes an analytic survey that
examines the existing thing without intentional
treatment to generate or cause a symptom or
condition (Notoatmodjo, 2010). The type of research
is causality. This research is done by the cross-
sectional approach, that is data collection of the
dependent variable and independent variable which is
done at the same time (Notoadmodjo, 2010). The
technique used in this study to determine the sample
size of the population is a systematic random
sampling technique (a simple random sample). Data
analysis used binary logistic regression analysis. The
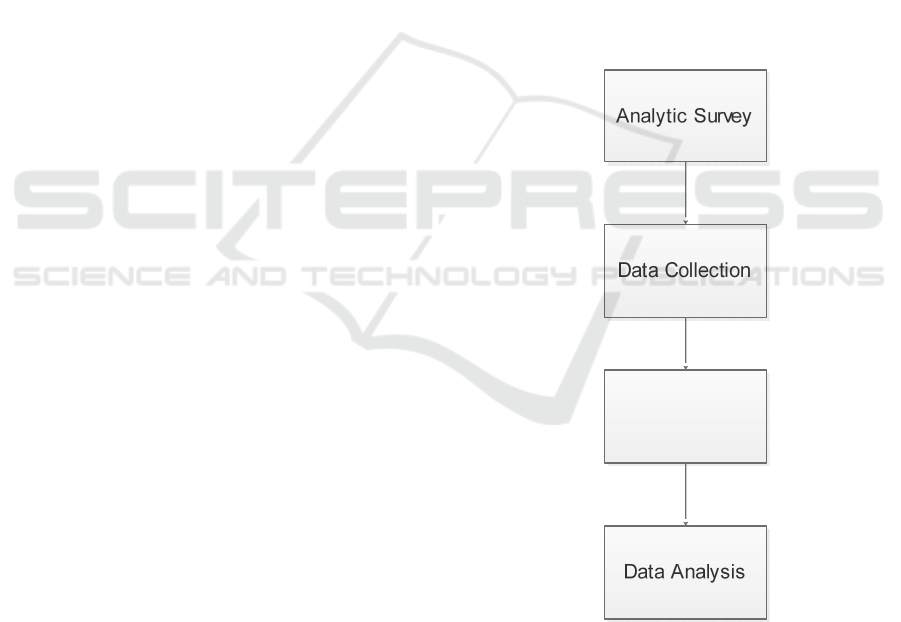
flowchart of the research method showed in Figure 1.
Figure 1: Research Method
3 OPERATIONAL DEFINITION
OF VARIABLES
The variable in this research is the dependent
variable (Y) is the claim filing claim approval for the
Determine the
Simple Size
Suspension Claim Health Insurance Hospitalized Due to Incomplete Medical Record
2995

guarantee of the health care needs of members
health insurance itself. With the instrument in the
form of a questionnaire consisting of 9 indicators
with a nominal scale. While the independent
variable (X) is the completeness of the medical
record is a file containing records and documents
about identity, examination, treatment, action, and
other services that have been given to the patient. In
this study consisting of patient identity accuracy,
improvement of drug safety, the certainty of the
procedure. With a questionnaire instrument
consisting of 17 indicators with a nominal scale.
4 RESEARCH RESULT
The results of the research are shown in the
frequency distribution of patient medical record
completeness as follows:
Based on the above can be seen that the medical
record completeness variable consists of 3
Dimensions. The first is the data identity dimension
consisting of 4 indicators, the second dimension is
the improvement of drug safety consisting of 6
indicators, the third dimension is the certainty of a
procedure consisting of 7 indicators.
From the table, it can be seen that on the identity
data of 98 respondents there are 95 documents
complete medical records with 97% percentage
whereas incomplete medical record document there
3 with 3% percentage, i.e.2 files no place, birth date
and 1 file no gender.
Furthermore, for the improvement of drug safety
that there are 92 complete medical records document
with percentage 94% while incomplete medical
record document there 6 with the percentage of 6%,
that is, each of 2 files is not exactly patient, 2 files
have no proper document, and 2 files are not on
time.
Lastly, for the improvement of drug safety, there
are 86 medical record documents complete with
88% percentage whereas incomplete medical records
document there are 12 with 12% percentage that is 1
file there are no diagnosis and 11 files there is no
odontogram file
.
Submission of Claim Health Insurance
approved 43% and not approved 57%. The
above table states that there are 56
unacceptable claims with 57%, whereas
approved
Claims are 42% with 43% Cross-tabulation of
the completeness of
medical record documents against claims
submission.
Based on the above table it is clear that RM
document is incomplete and not approved as much
as 16, RM document is incomplete and approved 0,
while RM complete document not approved 40 and
complete RM document approved 42.
4.1 Hypothesis Testing
Based on the above table the results of testing
individually or partially based on the above table
apart note that the value of wald on each variable of
19,470 (identity data), 14.303 (Improved Security of
drugs) and 23,000 (Certainty Procedure) and all sig
0.000 <0.05 (5 %), it can be concluded that the
accepted hypothesis is the data identity variable,
drug security, the certainty of the procedure partially
significant effect on the approval of the claim.
4.2 Discussion
4.2.1 Medical Record Compliance
Based on this research, data from 98 medical
record document samples are 82 complete medical
records document with the percentage of 83,6%,
while a document of incomplete medical record is
16 with percentage 16,4%. Medical records
according to the Indonesian Minister of Health
Regulation 269 / MENKES / PER / III / 2008 are
files containing records and documents on identities,
checks, medications, actions and other services that
have been provided to patients. Completeness of
medical record is very important because a complete
medical resume in addition to maintaining the
quality of medical records is also used for the
administration of insurance claims (Anggraini,
2013) .The results of this study in line with research
conducted by Ulfahet al. (2011) obtained data from
94 samples 85 complete medical record document
with the percentage of 90%, while incomplete
medical records document there are 9 with the
percentage of 10%.
According to the researchers, the following
matters are factors for the incompleteness of the
medical record document in this study, because the
patient did not fill in the data on the date of birth and
sex because the patient forgot to fill in the
consultation form. Also seen from the form filling
data supporting results that have been prepared but
not yet complete for example the diagnosis of
febristhypoid must be equipped with blood test
results, Tuberculosis equipped with sputum
examination and thorax photo.
ICRI 2018 - International Conference Recent Innovation
2996

4.2.2 Claim Submission
Based on research at Karawaci Hospital of
Tangerang, the researcher obtained the result of the
claim which has been approved by independent
verifier of 98 samples. There are 56 unacceptable
claims with 57% percentage, while the approved
claim is 42% with 43% percentage. Submission of
Claim Approval is the activity of the verification
process by the independent verifier to the
correctness of administration of responsibility of
service which has been executed by Hospital.
Complete claim requirements then the verification
process may be approved, the claim requirements
are incomplete then the verification process is not
approved and returned to the medical and financial
records to complete its administration based on the
results of its verification.
This research is in line with those done by Ulfah
et al. (2011), which are 9 people with incomplete
medical record documents, all of which are not
approved by Jamkesmas claim, and from the
complete medical record document, 52,9% are
approved by Jamkesmas claim.
According to the researchers can be seen that the
percentage of the approved 57% larger than the
approved is 42%, this is according to researchers
occur due to several factors. Of 56 unapproved
verifiers with 57% percentage, influenced by RM
incomplete document factor (no gender identity,
TTL, patient exact, proper document, odontogram
and diagnostic) and no physician's signature,
incompleteness as much as 16 data or 28.6%, then
because of diagnostic investigation result (thorac
examination and ct scan, blood test, urine
examination, therapy or medicine) data with
percentage 62.5% and because of coding rules there
are 5 data with percentage 8.9%. Based on the
number of factors affecting the unapproved claim,
the biggest factor affecting the claim is not approved
due to the incomplete investigation result
4.2.3 Influence Data Identity with
Submission of Health Assurance
Wald test results obtained wald value of 19.470
and p-value significance variable data identity of
0.000 <0.05 then reject H0. It can be concluded that
there is a significant influence on the data identity of
JS claim submission with the value of effect
coefficient which can be seen based on value (B) of
1.310.
The identity of medical record data is the
backbone of effectiveness and efficiency of medical
record system (WHO, 2002). The results of this
study are in line with research conducted by Ulfahet
al. (2011) where as many as 9% of unapproved
BPJS claims are affected by the incompleteness of
the RM document including the medical resume
containing the identity of the health insurance
patient data.
According to the researcher, the identity of the
data is the recording of all information about the
evidence of a person/Individual to establish and
equalize the information with a person. The
completeness of the document identity data greatly
affects the quality of RM data which will be
included in a medical resume which is the
requirement of health insurance claim submission
According to search results, there was no data of
2% sex and 2% on the place of birth date on the
medical record because the patient did not fill out
the data on the consultation form and the TPP officer
did not ask.
Whereas according to WHO (2002) the identity
of patient data must be written clearly and truthfully
because the truth of patient identity makes it easier
for hospital staff to:
To find out information about patients
whenever they come to health services
To connect the arrival of the previous patient
or the presence of outpatients and inpatients to
enter the targeted health service by using the
medical record number
To find the correct medical record if more
than one patient has the same name
Given the importance of the patient's data
identity in the RM, it is expected that the health
worker should be more proactive in assisting the
completeness of the patient's medical records file by
asking carefully and carefully about the patient's
identity and should ensure that the questions asked
are clear and understandable by the patient. Also,
there is cooperation between each section to
complete the filing of patient medical record files.
4.2.4 Effect of Improving Drug Security
with Submission of claims
Wald test results obtained wald value of 14.303
and indigo p-value significance of drug safety
improvement variables of 0.000 '<0.05 then rejected
H0 which proves that there is a significant effect of
increasing the safety of drugs against claims BPJS
with the value of the coefficient of influence can be
seen by value ( B) of 0.648.
Suspension Claim Health Insurance Hospitalized Due to Incomplete Medical Record
2997

Increased drug safety means to know precisely
the drug, proper dose, patient right, proper
document, a timely and appropriate way of
administration (WHO, 2002).According to
Permenkes no 28 of 2014 states that any reports of
drug services reported in BPJS claims should
contain data on drug use against individuals is claim
participants.
The results of this study are in line with previous
research conducted by Feriawati P and Kusunat AP
(2015) on factors of delay in claiming claim in
Bhayangkara Hospital Semarang, found documents
that are not equipped or about 5.7% of the total
samples included are incompleteness medical
resume data.
According to the research results of researchers
on incomplete RS documents (2%), right patient
(2%) and timely (2%) this happens because there are
still health workers who are not disciplined in
identifying patients with identification bracelet so
they can not be inputted in RM data. Also, because
of time limitations in the collection of RM
documents
According to the researcher, drug safety
improvement becomes part of file verification in
claim filing that is in the verification stage of
hospital service included in a medical resume. If the
hospital can meet the completeness of documents,
the faster the process of disbursement of claims.
4.2.5 The Influence of Certain Procedures
with Submission of Claims
Wald test results obtained wald value of 23,000
and value of p-value significance of the certainty of
the procedure of 0.000 '<0.05 then reject H0 which
proves that there is a significant influence the
certainty of the procedure against the approval of
claims with the value of coefficient of influence can
be seen based on value (B) of 0.893.
The certainty of the procedure is the certainty of
action seen from the date and time of action, the
results of the history, the filling of the odontogram,
the diagnosis, the plan of action management, the
investigation and the physical, informed consent
(WHO, 2002).
This result is in line with previous researchers
conducted by Ulfahet al. (2011) where as many as
9% of unapproved claim claims are affected by the
incompleteness of RM documents including most of
which are medical resumes containing diagnoses and
investigation results.
The researcher found that odontogram filling was
incomplete 11%. This is because the dentist feels
like overwhelmed because he has so many patients
can not make or prepare medical record records
odontogram in practice. While 1% (1 medical
record) there is no doctor diagnosis of the matter
because the doctor did not write the diagnosis or the
doctor's writing is unreadable.
The medical recorder will return to the polyclinic
through a nurse. However, if this is still allowed (the
doctor still does not write the diagnosis), then the
medical recorder will take back the medical record
and not coding the diagnosis. Medical record
officers rarely reprimand doctors for being reluctant
and have no binding rules such as Standard
Operation Procedure (SOP).
According to the researcher, the certainty of the
procedure becomes the condition of the
completeness of the medical record contents which
in the medical record should contain sufficient
information about the patient, giving the reason in
applying the diagnosis and equipment and recording
the entire examination result. Services obtained by
the patient during treatment or medical treatment.
The certainty of procedure becomes one of these
sections of medical record files that have
administrative value in claims due to their contents
concerning actions based on authority and
responsibility as medical and paramedical personnel
in achieving health service goals. Therefore the
more complete the document,the faster the
submission of claims BPJS.
4.2.6 Medical Record Completeness
Relation (Data Identity, Improvement
of Drug Security, Certainty of
Procedure) with Claim Submission of
Claim
Medical Record Completeness Relation (Data
Identity, Improvement of Drug Security, Certainty
Procedure) together can be seen from omnibus test
obtained Sig.Model value of 0.000 <0.05 so it is
concluded that the medical record completeness
variable (X) used, together affect the claim health
insurance submission (Y).
Medical records according to the Indonesian
Minister of Health Regulation 269 / MENKES /
PER / III / 2008 are files containing records and
documents on identities, checks, medications,
actions and other services that have been provided to
patients. The completeness of the medical record is
of great importance as a complete medical resume in
addition to maintaining the quality of medical
records is also used for the administration of
insurance claims (Anggraini, 2013).
ICRI 2018 - International Conference Recent Innovation
2998

Medical records are an important part of patient
management. RM is important for doctors and
medical officers as the patient's medical
documentation correctly in addition to the
importance of medical records due to two things
namely; The first is to help patients evaluate
appropriately and plan treatment protocols. Second,
the legal system relies primarily on documentary
evidence in case of medical negligence. Therefore,
medical records must be properly written and
maintained to serve the interests of the physician as
well as his patients (Amit, Bali et al., 2011).
Referred to the completeness of medical records in
this study is the completeness of medical record
documents regardingthe accuracy of data identity,
improvement of drug safety and certainty of
procedures.
According to Ilyas (2013), the claim is a request
of one of the two parties having a bond so that his
rights are fulfilled. One of the two parties who
commit the bond will file his/her claim to the other
party in accordance with the agreement or policy
provision mutually agreed upon by both parties. In
this case, the claim is claimedhealth insurance with
one of the requirements is the completeness of the
medical record.
The results of this research are in line with
previous research conducted by Ulfah et al. (2011)
conducted at RSI Sultan Agung Semarang obtained
the result that the importance of medical record data
to the smooth submission of claims. Where Of 9
people with incomplete medical record documents
all are not approved by claims, and from complete
medical records 52.9% are approved by health
insurance claims. In his research Ulfah, et al. (2011)
stated that SOP of claim submission already exists,
but still not according to the procedure, thepatient
often does not bring requirement, delay of claim
process health insurance happened partly because of
some of the data incomplete, often inconsistent
name of the patient.
Feriawati (2015) states that an incomplete DRM
file such as the absence of a doctor's signature and
the doctor's bright name, the diagnosis has not been
filled / not yet written / the diagnostic code, the
history of the course of the disease has not been
completely filled. This will lead to a delay in the
process of submitting a claim to health insurance.
Another study by Changfu (2013) states that the
accuracy and appropriateness of medical record
document information will help the Hospital in
making claims to the insurance provider against the
cost of services that have been issued by the
Hospital. The Hospital will easily obtain fees for
compensation in accordance with the applicable
rules and agreements. This is because a complete
and accurate medical record document can meet all
legal procedures, regulations and audit requirements.
According to the researchers, the completeness
of the medical record document is one of the
supporting in improving the quality of hospital
health services. Proper and correct documentation
will affect the quality of medical records as well as
ongoing medical records and patient care.
Completeness of DRM also affects the smoothness
of the insurance claim process both government and
private insurance to know the amount of payment to
be paid, from the information contained in the
medical record. In this research, the incompleteness
of medical record documentation is because there is
no diagnosis by doctors, incomplete data such as
evidence of laboratory results etc, and errors enter
the code.
Given the importance of medical record
completeness in the effort to file XYZ claim
therefore health officers should be more accurate in
collecting files so that there is no shortage of files in
the previous section, especially data completeness
investigation so that at the time of claiming can be
faster than that remind doctors to enforce diagnosis
according to the standard of medical service
according to the specialization of the case and
complete the complete and correct resume as well as
training for medical record officer according to
coding theory that is book of ICD-10 volume 2 in
order to meet the coding performance accuracy>
84%, and medical record officers need to perform
quantitative and qualitative analysis.
5 RESEARCH FINDING
The findings of research results based on
interviews and observations using various data
analysis can be expressed as follows: (1) It causes
incomplete medical records file that is: (a) The
patient did not fill out the data on the consultation
form and the TPP officer did not ask (b) Health
workers are not disciplined in identifying patients
with identification bracelet so it cannot be inputted
in medical record (c) Limitations of time in
document collection medical record: (2) The thing
that causes the claim submission is not approved (a)
Medical record documents are not complete and
there is no signature of the treating physician (b)
Completeness of investigation results such as
laboratory results, Rontgen photo and therapeutic
results, are given (c) Error enter the code
Suspension Claim Health Insurance Hospitalized Due to Incomplete Medical Record
2999

6 CONCLUSIONS
There is significant influence between the
Medical Record of Inpatient Patients of BPJS on
Claim Submission at RS. Sari Asih Karawaci
Tangerang Year 2017. This research has the
implications:
To the hospital management to conduct
socialization of SOP (Standard Operational
Procedure) complete medical record 1 X 24
hours after completion of service to all
doctors, nurses, midwives, nutrition,
physiotherapy, pharmacy and socialization
about the patient requirement of health
insurance medical records can be on time.
Attending or conducting training or seminar
seminars on the completeness of the medical
record for perfection in the service as well as
for law and claim
Creating service excellence training for all
officers at registration officer
Make the Internal Verifier Worker, who will
perform the completeness check of the
BPJSclaim submission requirements
For subsequent research, We have the
suggestions. They are:
Conducting socialization of SOP (Standard
Operating Procedure) on the filling of
Medical Record.
Revised Standard Operating Procedure claims
as a guide in carrying out routine work.
Regular evaluation of the incompleteness of
medical records file at Sari Asih Karawaci
Hospital Tangerang.
Increase the power for the hospital's Internal
Verifier, who will perform the initial
verification before submitting to health
insurance.
Conduct routine evaluation in the
implementation of health insurance services
ACKNOWLEDGEMENTS
The researchwas supported by Master of
Management, Faculty of Economy and
Business,Faculty of Law, Esa Unggul University.
REFERENCES
Amit, Bali Management of Medical Records: Facts and
Figures for Surgeons. E-journal. Milbank quarterly.
Retrieved via: https: //www.ncbi.nlm.nih .gov / pmc /
articles / PMC3238553. 2011
Anggraeni, C. A. D. Causes and Impacts of Non-
Inheritance of Medical Resume Sheet of Inpatient
Hospital at Sanjiwani Gianyar Hospital Bali. Thesis.
Vocational School of Gadjah Mada University,
Yogyakarta. 2010
Chang. Fu. The Impact of Medical Records Quality on
Claims of Significant Amounts of Medical Insurance.
E-journal Chinese Medical Record English Edition
Volume 1, 2013. Retrieved via
http://www.tandfonline.com/author/Fu%2C+Chang.
China. 2013
Notoarmodjo. Health Research Methodology. Jakarta:
Rineka Cipta. 2010
Pamungkas T. W., Marwati T., Solikhah, 2010. Analysis
of the Incomplete Filling of Medical Record File at
PKU Muhammadiyah Hospital Yogyakarta. Journal of
Kes-Mas Vol. 4, No. 1, January 2010: 1 - 75
Permenkes Number 269 / Menkes / Per / III / 2008. About
Medical Records. Jakarta: 2008
Ulfah, et al. Relation of Document Record Completion
With Approval Claim Jamkesmas By Verifikator With
INA System CBGs The Fourth Quarter 2011 In RSI
Sultan Agung Semarang. Semarang: FK Universitas
Dian Nuswantoro, 2011.
UU BPJS. Clarification Verification Technical
Directive.Jakarta: Directorate of Services, 2011
ICRI 2018 - International Conference Recent Innovation
3000
