
Economic Burden for Productive Age Malaria Patient:
Case Study in Mandailing Natal Regency
Destanul Aulia
1
, Intan Permata Sari
1
and Sri Fajar Ayu
2
1
Departement of Administration and Health Policy, Faculty of Public Health, University of Sumatera Utara, Jl. Universitas
No. 21 Kampus USU, Medan 20155, Indonesia
2
Departement of Agribusiness , Faculty of Agriculture, University of Sumatera Utara, Jl. A. Sofian No. 3 Kampus USU ,
Medan 20155, Indonesia
Keywords: Economic burden, malaria, inpatien, productive age, non productives age.
Abstract: Mandailing Natal is one of the endemic areas of malaria in Sumatera Utara Province. Besides having a high
transmission risk, malaria disease also impacts on patient's economy, both in productive and non-productive
age. This was a survey study for malaria inpatients from July to December 2017, using quantitative methods
calculated based on direct and indirect costs during treatment, then comparing the economics of productive
and unproductive age inpatient. Direct costs include inpatient fees, specialist doctor's visit, doctor's and
room services, personal hygiene officer, laboratory, medicine, and administration. Indirect costs include
transport, extra meals of patient and patient roommate, productivity loss of patient and patient roommate.
The purpose of this study was to compare the economic burden in productive and unproductive age patients
during treatment. The results showed that the total economic loss of productive age patients was
Rp1,907,116 and the total economic loss of unproductive age patients was Rp1,845,499. Total losses in
malaria patients of productive and non-productive age are almost the same, with a difference Rp61,667
more in productive age. The high malaria sufferer becomes a high economic burden for the patient, because
the productive age patient will lose productive time to work, and non productive age patient will be an
additional burden for the family. Mandailing Natal Government needs to develop a comprehensive strategy
and policy for the development and improvement of environmental sanitation and community behaviour,
because Mandailing Natal Regency is a malaria endemic area with high transmission risk affecting family
health and economy.
1 INTRODUCTION
Health development in Indonesia is currently faced
with triple burden disease and a condition with the
infectious diseases is still a public health problem.
Non-communicable diseases isincreasing, by the
emergence of new diseases. One type of infectious
infection disease that is of particular concern is
malaria. Malaria is one of the major public health
challenges in Indonesia, especially for rural
communities. According to (Ministry of Health,
Republic of Indonesia, 2018)malaria is an infectious
disease caused by parasites (protozoa) of the
plasmodium genus, which can be transmitted
through anopheles mosquito bites. Accorded to
Sorontou (Sorontou, 2013), malaria actually can be
prevented by individuals and communities by
treating susceptible persons and residents in endemic
areas, providing prophylactic treatment to
individuals entering malaria endemic areas,
eradicating the nest and anopheles mosquitoes using
suitable insecticides, using bed nets when sleep or
using repellent that is applied to the skin if it is
outside the house at night.
Besides disturbing health, malaria can also cause
economic burden. This can happen because a family
prioritized malaria treatment. Malaria patients in
Mandailing Natal District are dominated by
productive age with a 58% percentage compared
with unproductive age; this will be an economic
burden for society because patients and families of
productive age will lose time to work during malaria
treatment. While unproductive age patients will be
extra burden for the family.
The impact of economic losses caused by
malaria is very influential on the economy of society
138
Aulia, D., Sari, I. and Ayu, S.
Economic Burden for Productive Age Malaria Patient: Case Study in Mandailing Natal Regency.
DOI: 10.5220/0008883201380142
In Proceedings of the 7th International Conference on Multidisciplinary Research (ICMR 2018) - , pages 138-142
ISBN: 978-989-758-437-4
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
and government then it is important to conduct cost
analysis against malaria disease. Cost analysis of
malaria is a method to calculate the amount of
casualty (cost, cost) in monetary unit (rupiah), direct
cost or indirect cost, to reach the objective (Ministry
of Health RI, 2013).
According to WHO (WHO,2017), the cost of
care for malaria patients has increased by 4% from
232 million US dollars in 2015 to 241 million US
dollars by 2016. About 400 million US dollars each
year is needed to finance as a whole the prevention
and treatment of malaria in Indonesia, and 100
million US dollars to support health systems and
operations (UNICEF, 2009).
Based on data from the Central Bureau of
Statistics (BPS) on the results of the economic
census in 2016, the economy of Mandailing Natal
Regency decreased from 6.49% in 2014 to 6.21% in
2015. In addition, 93.47% of its workforce is in the
sector informal, This condition shows the level of
wage of the working population in the informal
sector is quite low, meaning that if the population is
faced with the high risk of transmission of malaria
then it is probable that the economic burden of
suffering from the disease is very vulnerable faced
by the community.
Analysis of malaria treatment cost is considered
very necessary to be done in Mandailing Natal
District because this area becomes one of malaria
endemic areas, so the risk of transmission of malaria
disease is very large and then affect the level of
morbidity and mortality.
2 METHODS
This study was a survey of malarial inpatients from
July to December 2017, using quantitative methods
calculated based on direct cost and indirect costs
during treatment, then comparing the economic
burden on the patient's age productivity and non-
productivity. Direct costs include inpatient fees,
specialist doctor's visit, doctor's services and room
attendant, personal hygiene officer, laboratory,
medicine, and administration. Indirect costs include
transport, patient extra meals and patient care, as
well as patient and patient productivity costs of
missing patients.
The inclusion criteria for sample selection are:
(1) Patients (BPJS and general) with the primary
diagnosis of uncomplicated malaria hospitalized in
July - December 2017; (2) Patients with complete
data (age, sex, LOS, treatment class, diagnosis) and
drug (drug name) and (3) Domiciled in Mandailing
Natal District.
3 RESULT
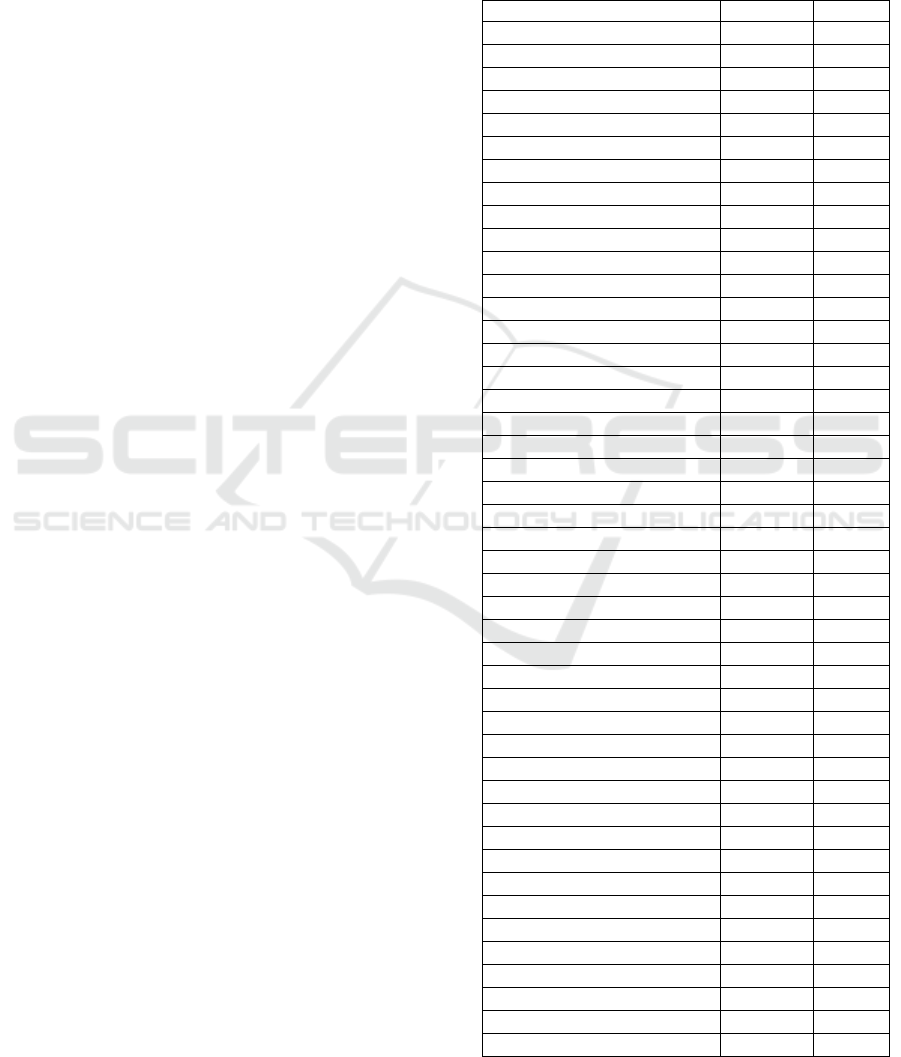
Table 1: Characteristics of respondents.
Characteristic Number
F %
Aged (Years)
a. 0-5
15 23
b. 16-11
10 15
c. 12-17
6 9
d. 18-23
6 9
e. 24-29
6 9
f. 30-35
3 5
g. 36-41
6 9
h. 42-47
4 6
i. 48-53
6 9
j. 54-59
2 3
k. 60-65
2 3
l. >65
0 0
Sex
a. Male
40 61
b. Female
26 39
Job
a. Non-Job
16 24
b. IRT
1 1
c. PNS
1 1
d. Privite Worker
3 4
e. Self-enterprise
5 8
f. Farmer
3 5
g. Merchant
7 11
h. Worker
6 9
i. Students
19 29
j. Others
5 8
Income
a. <Rp. 1.000.000
5 16
b. Rp1.000.000-2.000.000
14 45
c. >Rp. 2.000.000
12 39
Inpatient Class
a. VVIP
4 6
b. VIP
3 5
c. Class I
18 27
d. Class II
14 21
e. Class III
27 41
Assurance
a. BPJS
36 55
b. Genaral
30 45
LOS
a. <3 days
33 50
b. 3-5 days
32 48
c. >5 days
1 2
Economic Burden for Productive Age Malaria Patient: Case Study in Mandailing Natal Regency
139
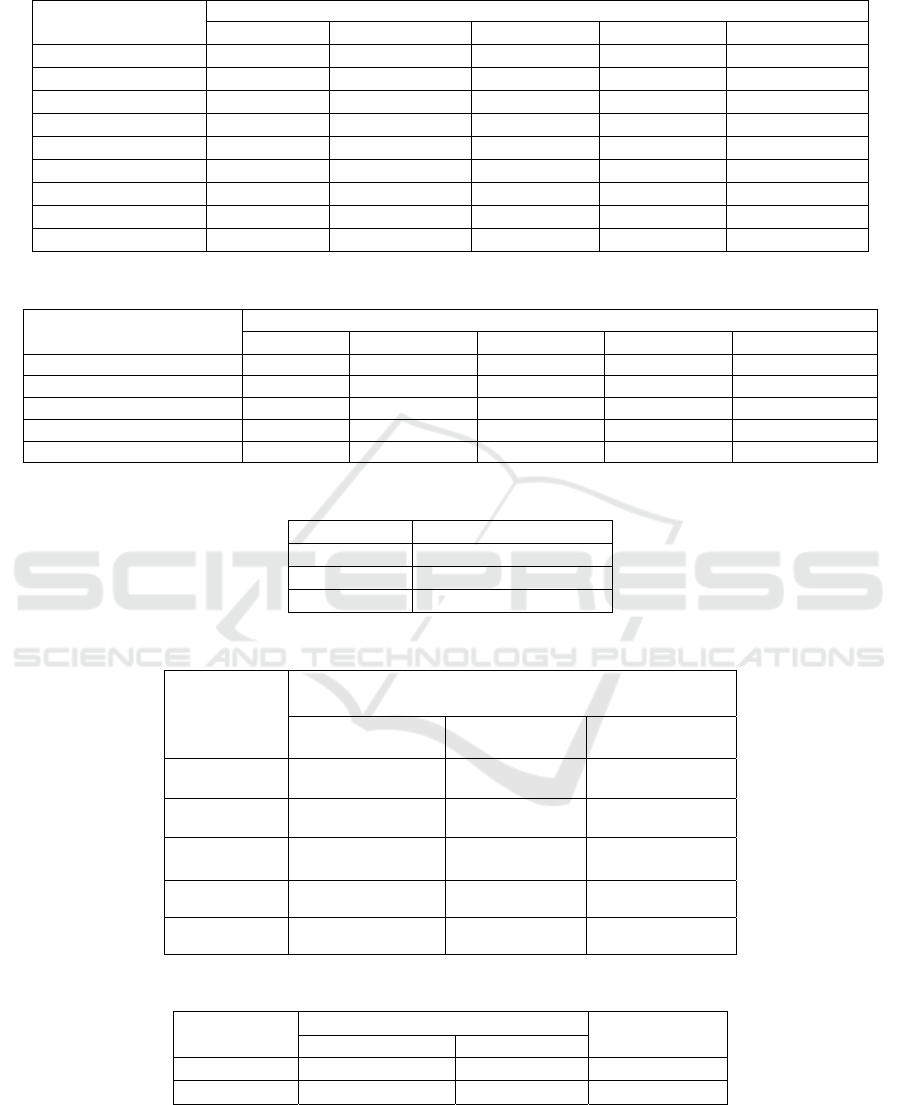
Table 2: Direct cost of general inpatien.
Direct Cost
Class (Rp)
VVIP VIP Class I Class II Class III
Drug 454675 273955 263770 5747000 1024755
dr Visiting 220000 120000 165000 190000 140000
Room worker 330000 240000 330000 510000 840000
Nurse 55000 40000 50000 95000 140000
Lab 440000 320000 400000 760000 1120000
Adm 60000 45000 60000 120000 165000
Inpatien 1815000 1120000 1200000 1140000 840000
Total 3374675 2158955 2468770 3389700 4269755
Average 843669 719652 617103 431213 388160
Table 3: Indirect cost of general inpatien.
Indirect Cost
Class (Rp)
VVIP VIP Class I Class II Class III
Transport
63000 159000 197000 305000 466000
Room-mate
538000 450000 482000 140000 762000
Loss of Productivity
1016000 1020000 624500 1273500 1340000
Total
1617000 1629000 1303500 1718500 2568000
Average
404250 543000 325875 214812 233455
Table 4: Direct costs of BPJS patients.
Class Total cost (Rp)
I 2.964.700
II 2.541.200
III 2.117.600
Table 5: Indirect cost of BPJS inpatient.
Indirect Cost
Total Cost
Class I
(n=14)
Class II
(n=6)
Kelas III
(n=16)
Transport
Rp.535.000 Rp.247.000 Rp.533.000
Room-mate
Rp.1.298.000 Rp.930.000 Rp.1.619.000
Productivity
Rp.3.994.500 Rp.2.144.000 Rp.2.428.750
Total
Rp.5.827.500 Rp.3.321.000 Rp.4.580.750
Average
Rp.416.250 Rp.553.500 Rp.286.297
Table 6: Average cost of malaria treatment.
Outcome Total
Direct cost Indirect cost
General Rp.525.650 Rp.315.067 Rp.840.717
BPJS Rp.2.517.628 Rp.381.368 Rp. 2.898.996
ICMR 2018 - International Conference on Multidisciplinary Research
140
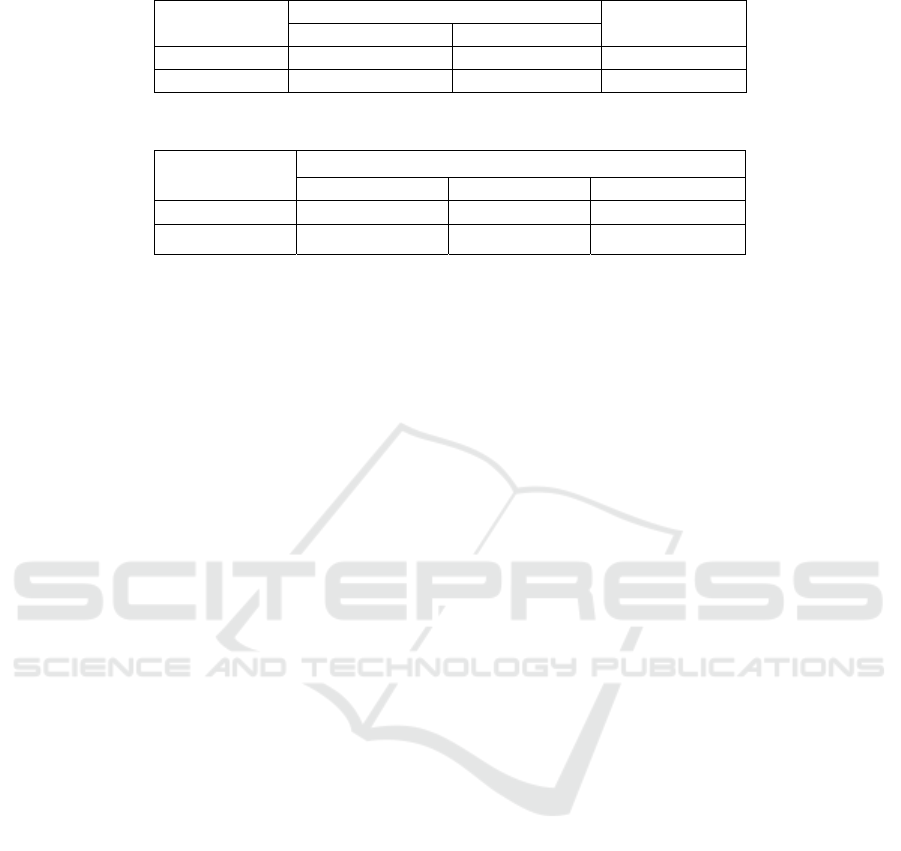
Table 7: Average malaria costs in productive aged.
Outcome Total
Direct Cost Indirect Cost
General Rp.609.037 Rp.369.038 Rp.978.076
BPJS Rp.2.416.582 Rp.407.926 Rp. 2.836.156
Table 8: Average malaria costs in non-productive aged.
Guaranted
Direct cost Indirect Cost Total
General Rp.461.883 Rp.273.794 Rp.735.677
BPJS Rp.2.608.037 Rp.347.184 Rp. 2.955.221
4 DISCUSSION
4.1 Characteristics of respondents
The results showed that in the productive age
category (15-65 years) there was a higher number
compared with the unproductive age of reaching
58%. The high number of malaria sufferers at the
productive age will have a greater impact on the
economic losses for both the patient and the family
and the government.Based on sex, it turns out that
most respondents who suffer from malaria is male
amounted to 40 people (61%), The cause of the large
number of male respondents exposed to malaria is
associated with a higher risk of malaria in males due
to environmental risks and working time and this is
will be a problem because male with productive age
is majority worker in Mandailing Natal. The income
of respondents who are productive age is
Rp.1.000.000 - Rp.2.000.000, - per month as 14
people (45%). average income of respondent is
Rp.1.683.710, - / month, this income of respondents
who are still below of regional income of
Mandailing Natal Regency in 2017 amounting to
Rp. 2,096,250, -. This indicates that the respondent
has limitations in saving his income every month
because the money is only enough for the daily
needs, so it will become an economic burden if
malaria occurs.Under the guarantor, patients are
guaranteed by BPJS more than the general patients.
While the type of treatment class is selected.
Mostpatients are in the third class is 41%. This is
because patients who are hospitalized via BPJS are
as much as 44%, a beneficiary contribution (PBI).
While in general patients, as many as 37% of
respondents chose class I as an option to get
inpatient services due to the cost of maintenance that
is quite affordable.Based on the long days of
hospitalization (long of stay), most of the 50% of
respondents treated ranged from 1-2 days. While the
overall average is for 3 days of care.
4.2 Total economic losses in general
patients (direct cost + indirect cost)
The total cost of the respondents directly related to
the treatment (direct cost) is Rp.15.769.495, - with
an average of Rp.525.650, In addition, respondents
also incur costs associated with loss of productivity
(indirect cost) with a total of Rp.8.947.000, - and an
average of Rp.315.067, -. The total economic loss of
the patient (general) as a whole is Rp. 23,673,470, -
and on average Rp. 840.717.
4.3 Total economic losses in patients of
bpjs (direct cost + indirect cost)
The total cost incurred by BPJS in the treatment
(direct cost) of malaria patients is Rp. 30.634.600, -
with an average of Rp. 2,517,628. In addition,
patients also incur costs associated with loss of
productivity (indirect cost) with a total of Rp.
13,729,250, - and on average Rp.381.368.
4.4 Cost comparison of productive and
unproductive age
The results showed that the total economic loss of
patients of productive age is Rp1,907,116 and total
economic losses of unproductive age patients is
Rp1,845,499. Total losses in malaria patients of
productive and non-productive age are almost the
same, with a difference of Rp61,667 more in
productive age, respondents of productive age and
have worked mostly as traders and labourers. If
malaria occurs they cannot work during
hospitalization and will lose their income. The cost
of productivity loss in this study is limited only
when the patient is admitted in hospital, as well as
Economic Burden for Productive Age Malaria Patient: Case Study in Mandailing Natal Regency
141

the companion calculated based on the length of
time he accompanies the patient in the room. The
total cost of loss of productivity will surely be
greater considering that after the patient leaves
treatment room, it still takes a few more days for
rehabilitation and rest until it is fully recovered and
ready to return to work as usual.The results showed
the average income of patients of productive age lost
with the length of 3 day care is Rp.176.927, - and
companyRp. 88146, -. While the unproductive age
patient does not lose income because there is no
wok, but the patient's family recovering their
treatment fee is lost with an average of Rp.136.836.
5 CONCLUSION
1. Based on the results of the study of malaria
patients hospitalized at RSUD Panyabungan
period July - December 2017 productive age
reaches 58% and male patients 61%.
2. Based on the type of work in productive-aged
patients, most of them are traders and labourers
and most unproductive age is student.
3. Total economic loss of patients (general) as a
whole is Rp. 23.673.470, - with an average of
Rp. 840.717, -. Total economic loss of patients
(BPJS) and government is Rp. 104,363,850, -
with an average of Rp. 2.898.996.
REFERENCES
As’ad, H., Asiah, H., dan Haerani. 2012.
KerugianEkonomi(Economic Loss)Pasien Rawat
InapUsiaProduktif Pada Lima Penyakit di RSUD Mamuju.
Jurnal AKK, Vol 1 No 1. Makassar:
UniversitasHasanuddin. Dipublikasi September 2012.
Badan Pusat StatistikKabupatenMandailing Natal. 2017.
SensusEkonomi 2016
Analisis Hasil Listing
PotensiEkonomiKabupatenMandailing Natal.
MandailingNatal : BPS KabupatenMandailing Natal.
Badan Pusat StatistikKabupatenMandailing Natal. 2017.
KondisiKesehatanPendudukKabupatenMandailing
Natal. MandailingNatal : BPS KabupatenMandailing
Natal.
DinasKesehatanKabupatenMandailing Natal. 2016.
LaporanPengendalianPenyakit Malaria Tahun 2015.
MandailingNatal
:DinasKesehatanKabupatenMandailing Natal.
DinasKesehatan Sumatera Utara. 2016.
LaporanPengendalianPenyakit Malaria Tahun 2015.
Medan :DinasKesehatan Sumatera Utara.
Kemenkes RI. 2008.
PelayananKefarmasianUntukPenyakit Malaria.
Jakarta: Kementerian KesehatanRepublik Indonesia.
. 2013. PedomanPenerapan Kajian
Farmakoekonomi. Jakarta: Kementerian
KesehatanRepublik Indonesia.
. 2017. ProfilKesehatan Indonesia
Tahun 2016. Jakarta: Kementerian KesehatanRepublik
Indonesia.
Sorontou, Y., 2013 .Ilmu Malaria Klinik. Jakarta:
EGC.
UNICEF. 2009. Fakta Malaria. Jakarta: UNICEF.
WHO. 2017. World Malaria Report 2017. Geneva: World
Health Organization
Yanuar, Ferri., 2003. BiayaAkibatSakit(cost of illness)
malaria: Studikasus di RSUD SungailiatKabupaten
Bangka Tahun2003.(Tesis). Jakarta: Universitas
Indonesia.
ICMR 2018 - International Conference on Multidisciplinary Research
142
