
Prevalence of Intestinal Parasitic Infections among Aborigine
Children in Kampung Ulu Gerik, Perak
Anita Talib
1
, Adibah Hanum Sahari
2
and Nazar Mohd Zabadi B. Mohd Azahar
2
1
School of Distance Education, Biology Section, Universiti Sains
M
alaysia, Minden, Penang 11800. Malaysia
2
Department Faculty of Health Science, University Teknologi MARA (UiTM) Bertam, Penang, Malaysia
Keywords: Ethnobiology, intestinal parasitic infections, helminths, indigenous children, polyparasitism
Abstract: Intestinal parasitic infections among indigenous children have been identified as one of the
important public health problems among the disadvantaged population. The prevalence of these
infections causes significant illnesses and diseases among children. This cross-sectional study
was conducted to determine the prevalence of intestinal parasitic infections and their associated
risk factorsamong children aged 2 to 14 years in Perkampungan Orang AsliUluGerik, Perak. A
total of 75 faecal samples were obtained in this study. Results from our study showed that the
intestinal parasitic infections were prevalent among indigenous children. Infection by
Trichuristrichiura was the most common infection (65.3%), followed by Hookworm (46.7%),
Ascarislumbricoides (42.7%) and Entamoeba spp. (16.0). Only 1.3% of children had Giardia
spp. infection. More than half of the children in this study hadpolyparasitism representing 54.7%.
Social and environmental factors such as Father’s occupation (p=0.019), water sources
(p=0.039), type of toilet (p=0.026) and intake of the supplement (p=0.021) were significantly
associated with polyparasitism. Promotion of preventive measures such as deworming, increase
of awareness on healthy lifestyle and improvement in housing facilities are urgently needed to
reduce the intestinal parasitic infections in this community.
1 INTRODUCTION
Intestinal parasitic infection among indigenous
people is one of the critical public health problems
(Hartini et al., 2013). The World Health
Organization (WHO, 2015) has highlighted that 24%
of people have been infected with intestinal parasitic
infections such as protozoan infections and soil-
transmitted helminths (STH). Majority of infected
people are residing in the developing countries
(Hartini et al., 2013). Demographic changes and
rapid socio-economic development in Malaysia have
resulted in high endemic of intestinal parasitic
infection among indigenous communities especially
among children (Chin et al., 2016). In Peninsular
Malaysia, indigenous communities are minority
groups of people separated into three main tribal
groups: Semang (Negrito), Senoi and Proto-Malay
(Aboriginal Malay) consisting of 19 ethnicities
(Chin et al., 2016). They have various lifestyles,
having unique languages, knowledge systems and
invaluable knowledge of practices for the
sustainable management of natural resources
(Tarmiji et al., 2013).
The high prevalence of parasitic infection is
associated with poverty, poor environmental
conditions, lack of clean water, lack of proper faecal
disposal, growth impairment, school performance
and cognitive function of children (Norhayati et al.,
2003). Transmitting of intestinal parasites by faecal-
oral route and infection can be severe if left
untreated and if the immune system is weak
(Norhayati et al., 2003). The main presenting
symptoms for intestinal parasitic infections are
diarrhoea, fever, nausea and vomiting (Sinniah et al.,
2012). The most common STH found in Malaysia
are Ascarislumbricoides, Trichuristrichiura and
hookworm (Norhayati et al., 2003). The most
predominant intestinal protozoan infections are
giardiasis caused by Giardia duodenalis, followed
by amoebiasisand caused by Entamoebahistolytica
(Romano et al., 2011).
There are three methods of STH transmission:
direct, modified direct and through penetration of
Tallib, A., Sahari, A. and Azahar, N.
Prevalence of Intestinal Parasitic Infections among Aborigine Children in Kampung Ulu Ger ik, Perak.
DOI: 10.5220/0008882400970102
In Proceedings of the 7th International Conference on Multidisciplinary Research (ICMR 2018) - , pages 97-102
ISBN: 978-989-758-437-4
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
97

the skin (Sina et al., 2012). Intestinal parasitic
infections are still prevalent among indigenous
children, ranging from 66.2% to 79.8% (Rahmah et
al.,1997; Yusof and Abd. Ghani 2011; Leroy and
Chua, 2016). In 2003, the World Health
Organization (WHO) revealed that soil-transmitted
helminthiasis had an adverse effect on growth and
development of children aged 2-14 years old. Thus,
the parasitic diseases will continue to threaten the
people’s health especially among communities from
rural areas if no appropriate actions are taken to
diminish the transmission of the parasites (Hartini et
al.,2013). Since the 1930s, numbers of research have
been conducted on intestinal parasitic infection
mainly soil transmitted helminths as they are
believed to be one of the tremendous medical
importance among children living in remote areas.
Intestinal parasitic infections are significantly
associated with environmental and personal hygiene
practices (Lim et al., 2009). This study highlights the
prevalence and risk factors for intestinal parasitic
infection among aborigine children in Malaysia.
Such information is important for the respective
parties to implement strategies or intervention to
reduce the risk of getting intestinal parasitic
infection among children.
2 MATERIAL AND METHODS
2.1 Study Site
The present study was conducted within the area of
HuluGerik, an area located in the north-eastern state
of Perak; on the east side of the state, a boundary
with the state of Kelantan, while in the north west,
with PengkalanHulu. In the south of this area is the
district of Lenggong. Bordering with Thailand on
the northeast, this area is also one of the gateways
between Malaysia and Thailand. The south-western
part of the area is Larut, Matang and Selama.
Participants from this study were children aged 2 to
14 years old residing in Perkampungan Orang Asli,
UluGerik. Data collection was started on December
2017 and ended in March 2018.
2.2 Sampling Techniques
A clean, wide-mouth screw-cap container pre-
labeled with the individual’s name and code for the
collection of faecal sample, 10% formalin, 15ml
Falcon tube, applicator wood stick, distilled water,
centrifuge, ethyl acetate, iodine 0.05 MOL/1(0.1N),
transfer pipette 3ml, microscopic slide frosted end,
microscopes coverslips and light microscope.
Stool specimens were collected from children
aged 2 to 14 years old. For children aged under 4
years, the stool collection was done by assistance
from their parents or guardians. The samples were
collected on the following day. The fresh stool
samples were added immediately with 10% formalin
and placed into the ice box before transported back
to the Parasitology laboratory, Faculty of Health
Sciences, UniversitiTeknologi MARA (UiTM)
Bertam, Penang on the same day of collection. Each
stool sample was fixed with 10% formalin and
stored at 4°C to 10°C until further analysis.
2.3 Formalin-ethyl ether Sedimentation
Techniques for Detection of
Intestinal Parasites
Stool sample fixed with 10% formalin was mixed
well using wood applicator stick. Approximately
5ml of each formalinized specimen was strained
through one layer of wet gauze into a 15ml Falcon
tube. Distilled water was added to a volume of 10ml.
The suspension was mixed well and centrifuged at
1500 rpm for 2 minutes. Then, the supernatant was
decanted using Pasteur pipette and distilled water
was added again to a volume of 10ml. By using a
micropipette, 3ml of ethyl acetate was added to each
tube. The tube was screwed with cap and shake
vigorously for 30 seconds. Then the mixture was
centrifuged with a table model centrifuge at 1500
rpm for 2 minutes. After centrifugation, it became
four layers: ether, debris, formalin and faeces. The
supernatant was discarded. The pellet was suspended
in residual water and homogenized with gentle
stirring. Slide for observation was labelled with
respondent’s identification code. A small drop of
pellet and iodine was placed on the slide for
examination.
ICMR 2018 - International Conference on Multidisciplinary Research
98
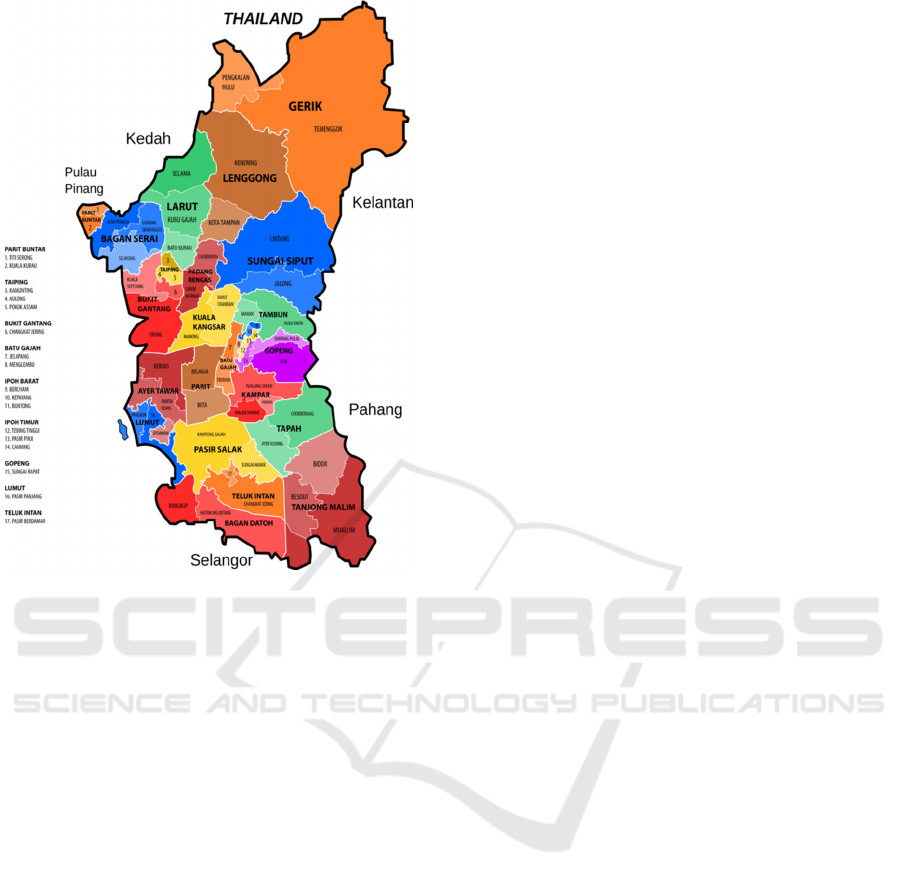
Figure 1 : The map of Perak showing the location of Gerik
(Pejabat Tanah dan Daerah Hulu Perak).
3 RESULTS AND DISCUSSIONS
In this cross-sectional study there were 75 children
aged 2-14 years old participated. The mean age of
children was 6.4±3.4 years. Almost half of the
children were aged 4 to 8 years (45.3%) and
majority was female representing 54.7%. A third of
children (35.7%) in this study wear shoes when they
were outside house. Almost all (96.0%) of children
in this study received complete vaccination from the
nearest government health clinics. Parental
information among children was assessed in this
study. A majority of the fathers work as rubber
tapper (54.7%) and 41.3% of them did not have any
formal education. Meanwhile, most of the mothers
were housewives (65.4%) and 53.3% of them did
not have any formal education. The mean age of
father was 40.6±9.4 years while 34.2±8.9 years for
mothers. With regards to monthly household
income, the mean was reported as RM309.3±121.0.
In reference to the family size of participants, the
mean total of kids in a family was 3.19±1.6 kids.
Meanwhile, more than half of the respondents
(53.3%) did not receive any financial assistance to
support their daily life. With regards to their housing
facilities, 45.3% of the respondents used treated
water sources, 58.7% have television and 48% had
radio. About two-thirds of the respondents (69.3%)
did not have toilet facilities in their home while 68%
of the respondents did not have proper defecation
place status. Only 40% of the respondents had pet at
their home. Nearly half of the respondents (46.7%)
took supplement as their additional food. All
respondents received antihelminthic agents and did
not have any systematic garbage disposal (Table 1).
There were five intestinal parasites identified in
this study: Trichuristrichiura, Ascarislumbricoides,
Hookworm, Giardia spp. and Entamoeba spp. In
total, 65.3% of children were infected by
Trichuristrichiura, followed by Hookworm (46.7%),
Ascarislumbricoides (42.7%) and Entamoeba spp.
(16.0%). Only one child was infected by Giardia
spp. and, 12.0% of children did not have any
intestinal parasitic infection. Intestinal parasitic
infection by Trichuristrichiurawas the highest
among male and female children representing 64.7%
and 65.9% respectively. In total, there were 33.3%
of children withmonoparasitism, 30.7% two
parasites, 18.7% three parasites and 5.3% four
parasites. The prevalence of children with
polyparasitism (having at least two types of
infection) in this study was 54.7%. The prevalence
of intestinal parasitic infection by gender in this
study was presented in Table 2. Our results showed
that Trichuristrichiura was the highest intestinal
parasitic infection among children. Similar to studies
done by previous researchers in other sub-ethnic
groups (Chin et al, 2016; Delaimy et al., 2014; Nasr
et al., 2013; Ngui et al., 2015; Lee et al., 2014;
Anuar et al., 2014; Sinniah et al., 2012). Delaimy et
al., (2014) found that almost all children were
positive for Trichuristrichiura infection (95.6%).
One of the factors for the high prevalence of
Trichuristrichiura infection might be due to
occurrence of super infection. This occured when
the children harboring the parasite was re-infected
with similar parasite especially due to ineffective
treatment against this infection (Ng et al., 2014). Our
results also showed that Hookworm was the second
highest intestinal parasitic infection. This finding is
contradictory with studies done by other researchers
(Chin et al., 2016; Nasr et al., 2013; Ngui et al.,
2015; Anuar et al., 2014) whereby the infection by
Ascarislumbricoides is the second most common
intestinal parasitic infection among indigenous
population followed by Hookworm infection. This
might be due to the fact that the current study was
conducted among Temiar sub-ethnic group
meanwhile the previous studies were conducted
Prevalence of Intestinal Parasitic Infections among Aborigine Children in Kampung Ulu Gerik, Perak
99
among Temuan and MahMeri sub-ethnic groups.
Since the prevalence of infection by
Trichuristrichiura, Hookworm and
Ascarislumbricoideswere high, this study
hypothesized that the soil contamination with these
parasites was higher in this indigenous community.
In addition, most of the children in this study did not
wear shoes (64.3%) and 68% of them did not have
proper defecation place status. This will increase the
rate of intestinal parasitic transmission in the
community. However, this hypothesis should be
further confirmed with soil analysis. The finding of
the present study showed that most of the children
had polyparasitism (54.7%). Only a third of the
children had monoparasitism. The prevalence of
polyparasitism in this study was lower compared to
that reported by Delaimy et al., 2014 (71.4%). In
another study a much higher prevalence of
polyparasitism was found among respondents in
western Cote d’Ivoire (Raso et al., 2014). However,
the prevalence of polyparasitism in the current study
was slightly higher compared to a study conducted
by Chin et al., 2016. They found that the prevalence
of polyparasitism among Temuan and Mah-Meri
was 41.5% and 32.5% respectively. Current findings
indicate that the environment among indigenous
population is heavily contaminated with the
parasites. It is important findings because children
with polyparasitism may suffer from multiple
morbidity due to each species infection (Booth et al.,
1998).
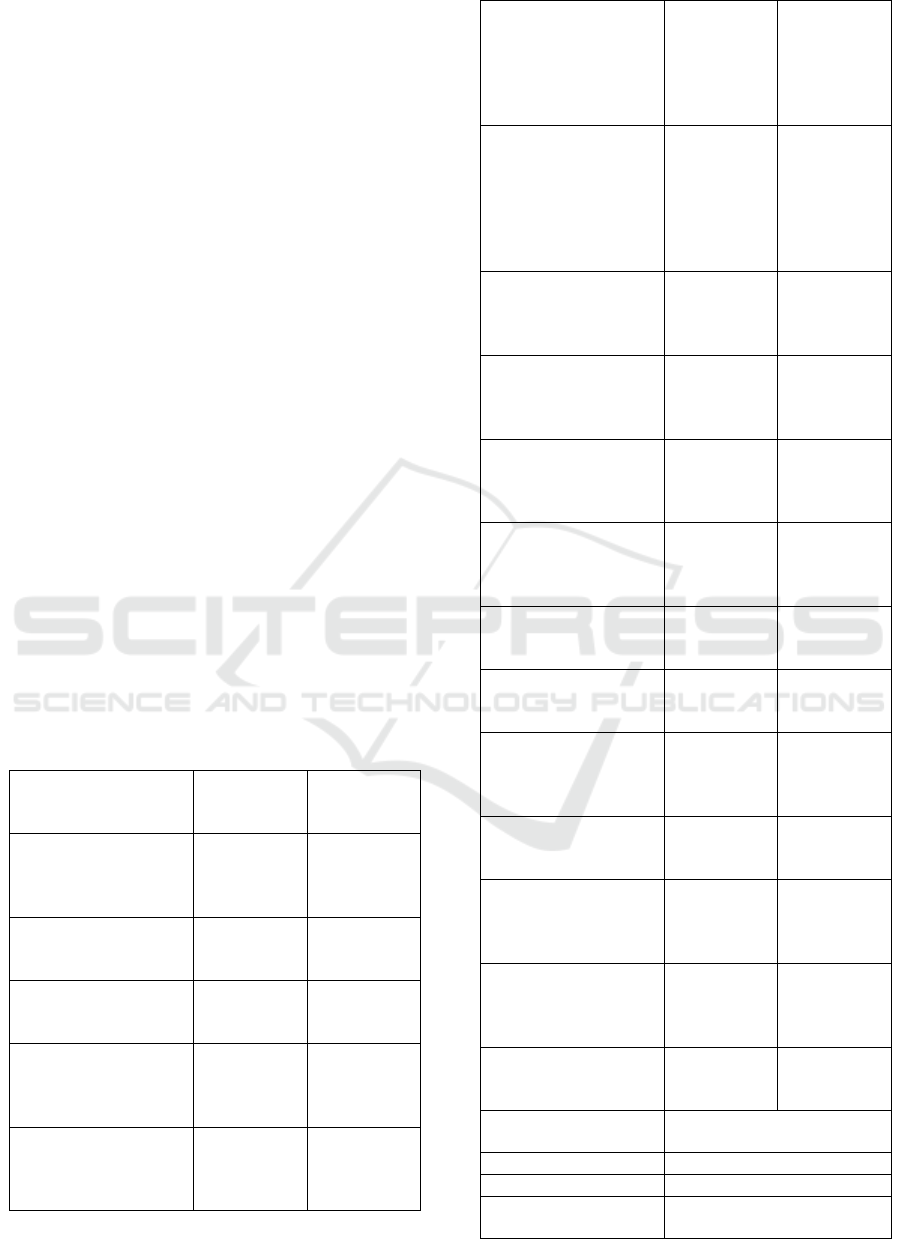
Table 1: Socio-demographiccharacteristics of respondents.
Socio-
demographic
characteristics
Frequency
(n)
Percentage
(%)
Age groups (n=75)
- Less than 4 years
- 4-8 years
- 9-12 years
20
34
21
26.7
45.3
28.0
Sex (n=75)
- Female
- Male
41
34
54.7
45.3
Wear shoe (n=70)
- Yes
- No
25
45
35.7
64.3
Father’s occupation
(n=75)
- Farmer/Hunter
- Rubber tapper
34
41
45.3
54.7
Mother’s occupation
(n=75)
- Rubber tapper
- Housewives
26
49
34.7
65.3
Father’s educational
level (n=75)
- No formal education
- Primary school
- Secondary school
31
29
15
41.3
38.7
20.0
Mother’s educational
level (n=75)
- No formal education
- Primary school
- Secondary school
40
29
6
53.3
38.7
8.0
Completed
vaccination (n=75)
- Yes
- No
72
3
96.0
4.0
Received financial
assistance (n=75)
- Yes
- No
35
40
46.7
53.3
Water sources (n=75)
- Treated
- Not treated
34
41
45.3
54.7
Own television
(n=75)
- Yes
- No
44
31
58.7
41.3
Own radio (n=75)
- Yes
- No
36
39
48.0
52.0
Type of toilet (n=75)
- No toilet facilities
-Proper toilet facilities
52
23
69.3
30.7
Defecation place
status =(n=75)
- Other places
- Proper toilet
51
24
68.0
32.0
Own pet (n=75)
- Yes
- No
30
45
40.0
60.0
Garbage disposal
(n=75)
- Systematic
- Not systematic
0
75
0
100
Antihelminthic drugs
(n=75)
- Yes
- No
75
0
100
0
Supplement (n=75)
- Yes
- No
35
40
46.7
53.3
Mean respondent’s
age
6.4±3.4
Mean father’s age 40.6±9.4
Mean mother’s age 34.2±8.9
Mean household
income (RM)
309.3±121.0
ICMR 2018 - International Conference on Multidisciplinary Research
100
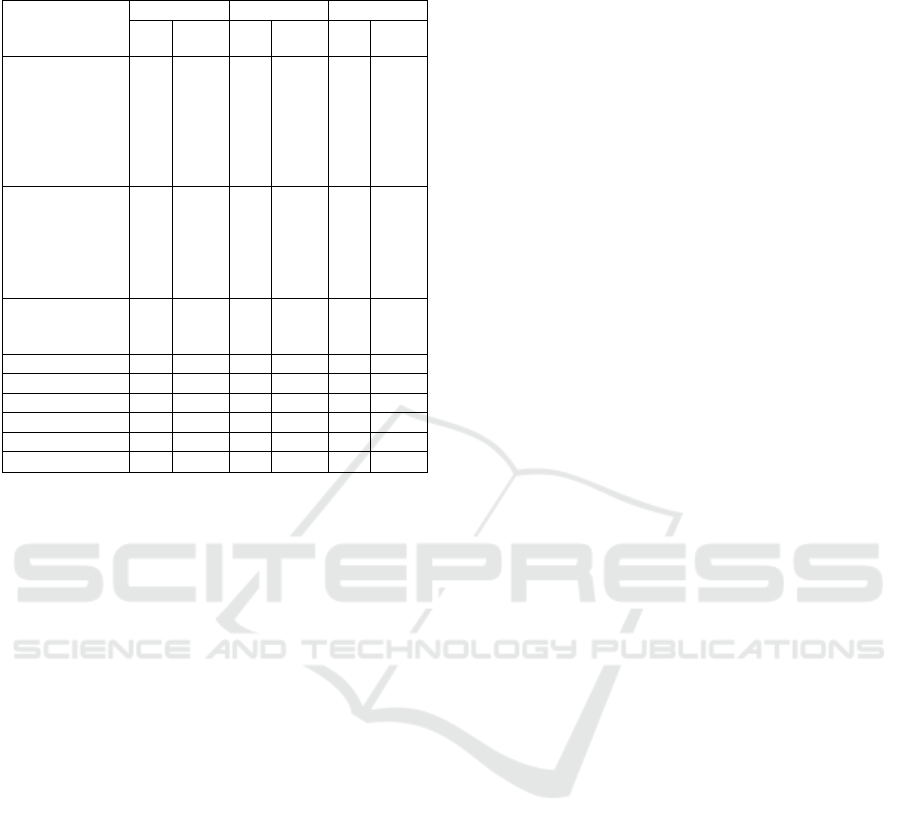
Table 2: Prevalence of intestinal parasitic infection by
gender.
Intestinal
parasitic
infection
Male Female Total
n % n % n %
Helminth
infection
- Trichuristric
hiura
- Ascarislumbr
icoides
- Hookworm
22
10
15
64.7
29.4
44.1
27
22
20
65.9
53.7
48.8
49
32
35
65.3
42.7
46.7
Protozoan
infection
- Giardia
spp.
- Entamoeba
spp.
1
4
2.9
11.8
0
8
0.0
19.5
1
12
1.3
16.0
No intestinal
parasitic
infection
4 11.8 5 12.2 9 12.0
Monoparasitism 15 44.1 10 24.4 25 33.3
Two parasites 10 29.4 13 31.7 23 30.7
Three parasites 3 8.8 11 26.8 14 18.7
Four parasites 2 5.9 2 4.9 4 5.3
Polyparasitism 15 44.1 26 63.4 41 54.7
4 CONCLUSIONS
The results of the present study show the existence
of intestinal parasitic infection among aborigine
children. The prevalence of Trichuristrichiura
infection is the highest in this study and there are
54.7% of respondents withpolyparasitism.
Significant risk factors for polyparasitismare father’s
occupation, water sources, type of toilet facilities
and intake of supplement. Findings from this study
provide information for the responsible agencies to
promote strategic plans to reduce the rate of
intestinal parasitic infection among aborigine
community. Our study highlights the possibility that
polyparasitism could be affecting the health of
young children especially in indigenous
communities, hence Malaysian government should
put on more efforts on preventive measures such as
socio-economic development programmes to
increase knowledge and awareness and to educate
the aborigine community about disease control such
as periodic chemotherapy, provision of safe water
and improvement in hygienic practices.
ACKNOWLEDGEMENTS
Acknowledgements to School of Distance
Education, USM for the support granted to this
research in collaboration with Department of Faculty
of Health Science, University Teknologi MARA
(UiTM) Bertam, Penang. Gratitude is extended to
the staff ofJabatanKemajuan Orang Asli (JAKOA) ,
and Head of Department of Faculty of Health
Science, University Teknologi MARA (UiTM)
Bertam, Penang, En. Amir Herberd B Abdullah at
Clinical Research Laboratory for their support and
assistance.And to Head of Villages atPerkampungan
Orang AsliUluGerik, Perak and their respective
committees for their assistance in data collection.
REFERENCES
Anuar, T.S., Salleh, F.M., Moktar, N., 2014. Soil-
transmitted helminth infections and associated risk
factors in three Orang Asli tribes in Peninsular
Malaysia.Sci Rep 4:4101.
Booth, M., Bundy, D.A.P., Albonico, M., Chwaya, H.M.,
Alawi, K.S., Savioli, L., 1998. Associations among
multiple geohelminth species
Chin, Y. T., Lim, Y. A. L., Chong, C. W., The, C. S. J.,
Yap, I. K. S., Lee, S.C., Tee, M. Z., Siow, V.W.Y and
Chua, K. H., 2016. Prevalence and risk factors of
intestinal parasitism among two indigenous sub-ethnic
groups in Peninsular Malaysia. Infectious Disease of
Poverty 5: 77.
Delaimy, A.K., Al-Mekhlafi, H.M., Nasr, N.A., Sady, H.,
Atroosh, W.M., Nashiry, M., et al.,
2014.Epidemiology of intestinal polyparasitism among
Orang Asli school children in rural
Malaysia.PLoSNegl Trop Dis 8:e3074.
Hartini, Y., Geishamimi, G., Mariam, A.Z., Mohamed-
Kamel, A.G, Hidayatul, F.O. and Ismarul, Y.L., 2013.
Distribution of Intestinal Parasitic Infections Amongst
Aborigine Children at Post Sungai Rual, Kelantan,
Malaysia. Tropical Biomedicine 30(4): 596-601.
Lee, S.C., Ngui, R., Tan, T.K., Muhammad Aidil, R., Lim,
Y.A.L., 2014. Neglected tropical diseases among two
indigenous subtribes in peninsular Malaysia:
highlighting differences and co-infection of
helminthiasis and sarcocystosis. PLOS One
9:e107980.
Leroy, A.L., Chua, T. H., 2016. Worm infection among
children in Malaysia.Borneo journal of medical
sciences. 10(1) :59-74
Lim, Y.A.L, Romano, N., Colin, N., Chow, S.C. and
Smith, H.V., 2009. Intestinal parasitic infections
amongst Orang Asli (indigenous) in Malaysia: Has
socioeconomic development alleviated the problem?
Tropical Biomedicine 26(2): 110-122.
Prevalence of Intestinal Parasitic Infections among Aborigine Children in Kampung Ulu Gerik, Perak
101

Nasr, N.A., Al-Mekhlafi, H.M., Ahmed, A., Roslan, M.A.,
Bulgiba, A., 2013.Towards an effective control
programme of soil-transmitted helminth infections
among Orang Asli in rural Malaysia. Part 1:
prevalence and associated key factors. Parasit Vectors
6:27.
Ng, J.V., Belizario,J.r. V.Y, Claveria, F.G., 2014.
Determination of soil-transmitted helminth infection
and its association with hemoglobin levels among
Aeta schoolchildren of Katutubo Village in Planas,
Porac, Pampanga. Phil SciLett. 7: 73–80.
Ngui, R., Aziz, S., Chua, K.H., Aidil, R.M., Lee, S.C.,
Tan, T.K., et al., 2015. Patterns and risk factors
Norhayati, M., Fatmah, M.S., Yusof, S. and Edariah, A.B.,
2003. Intestinal parasitic infection in man: A Review.
Medical Journal of Malaysia 58: 296-305
Pejabat Tanah dan Daerah Hulu Perak.Geografi Daerah.
http://pdtgerik.perak.gov.my/profil/informasi-
daerah/geografi-daerah. Access on 30 September 2017
Rahmah, N., Ariff, R.H., Abdullah, B., Shariman, M.S.,
Nazli, M.Z. and Rizal, M.Z., 1997. Parasitic infections
among aborigine children at Post Brooke, Kelantan,
Malaysia.Medical Journal of Malaysia 52: 412-414.
Raso, G., Luginbu¨hl, A., Adjoua, C.A., Tian-Bi, N.T.,
Silue´, K.D., et al., 2004.Multiple parasite infections
and their relationship to self-reported morbidity in a
community of rural Coˆte d’Ivoire.Int J Epidemiol 33:
1092–1102.
Romano, N., Saidon, I., Chow, S.C., Rohela, M. and
Yvonne, A.L.L., 2011.Prevalence and Risk Factors of
Intestinal Parasitism in Rural and Remote West
Malaysia.PLoS Neglected Tropical Diseases 5(3):
e974.
Sina, H., Akre, M.A., Alia, T. and Neil, A., 2012.Soil-
transmitted helminths.Global Health Education
Consortium.
Sinniah, B., Sabaridah, I., Soe, M.M., Sabitha, P., Awang,
I.P.R., Ong, G.P. and Hassan, A.K.R., 2012.
Determining the prevalence of Intestinal Parasites in
Three Orang Asli (Aborigines) communities in Perak,
Malaysia.Tropical Biomedicine 29(2): 200-206.
Tarmiji, M., Fujimaki, M., Norhasimah, I., 2013. Orang
Asli in Peninsular Malaysia: Population, Spatial
Distribution and Socio-Economic
Condition.www.ritsumei.ac.jp/acd/re/k-
rsc/hss/book/pdf/vol06_07.pdf. Access on 11
November 2017.
World Health Organization : Soil-transmitted helminth
infections. Fact sheet no. 366 updated May 2015.
http://www.who.int/mediacentre/factsheets/fs366/en/
Accessed 09 February 2018.
Yusof, H. and Abd.Ghani, M.K., 2011. Intestinal parasitic
infections among Orang Asli children at PosLenjang,
Pahang.First Regional Health Sciences and Nursing
Conference 2011.
ICMR 2018 - International Conference on Multidisciplinary Research
102
