
Successful Methotrexate Therapy in Management Caesarean Scar, an
Ectopic Pregnancy: A Case Report
Putri Irmayani
1
,
Cut Meurah Yeni
2
1
Department Of Obstetrics & Gynecology, Dr.Zainoel Abidin, Hospital Banda Aceh, Indonesia
2
Feto Maternal Division, Department Of Obstetrics & Gynecology Syiah Kuala University – Dr.Zainoel Abidin Hospital
Banda Aceh, Indonesia
Keywords: Caesarean Scar, Pregnancy, Methotrexate, Management.
Abstract : An ectopic pregnancy developing in a Caesarean scar pregnancy (CSP) is a very rare case. We describe the
case of a-31 years old-women G4P2A1 6-7 weeks gestational age (wga), previous c-section 2 times, inter
delivery time (IDT) 2 years. She came with chief complaint amenorrrhoea for five weeks and was found to
have a positive urine pregnancy test. Transvaginal ultrasonography showed uterus was within normal limit
and there was a single intrauterine gestational sac positioned in the region lower segment caesarean section.
a local injection of NaCl 0,3 % into the amniotic sac under ultrasound guidance resulted embryonic demise.
Following the local injection, one doses of methotrexate were given intramuscular methotrexate 50 mg/m
2
.
The early diagnosis of caesarean scar ectopic pregnancy via transvaginal ultrasound is fundamental for a
successful conservative treatment.
1 INTRODUCTION
An ectopic pregnancy developing in a Caesarean
scar pregnancy (CSP) is a very rare case (Sapana et
al, 2014). Caesarean scar ectopic pregnancy occurs
where in the conceptus is implanted into the site of
previous caesarean section (Cunningham et al,
2014). Incidence of caesarean section is increasing
worldwide, therefore more cases are diagnosed and
reported (Srinivas et al, 2014). This type of ectopic
pregnancy carries with it a high risk of maternal
morbidity related to uterine rupture, miscarriage
with hemorrhage, placenta praevia with or without
accrete, and hysterectomy. Early diagnosis can offer
preservation woman’s fertility. Treatment options
CSP are medical management to surgical techniques,
which is medical use local/systemic methotrexate
(MTX) (Ross, 2016).
2 CASE REPORT
A-31 years old-women G4P2A1 6-7 weeks
gestational age (wga), previous c-section 2 times,
inter delivery time (IDT) 2 years. She came with
chief complaint amenorrrhoea for five weeks and
was found to have a positive urine pregnancy test.
Her first pregnancy was a spontaneous complete
abortion of four months pregnancy. Her second
pregnancy was an uneventful emergency caesarean
section pregnancy at 9 months due to severe
headache. She underwent elective caesarean section
in her third pregnancy due to previous c-section 1
time (IDT 16 months).
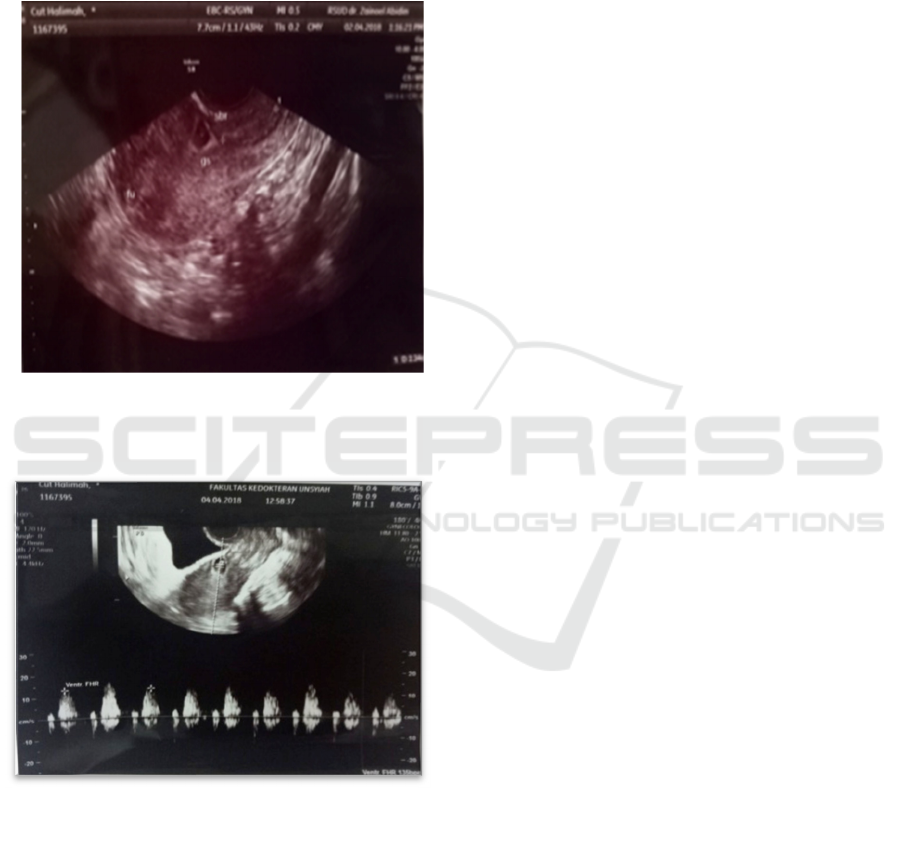
Transvaginal ultrasonography showed uterus was
within normal limit and there was a single
intrauterine gestational sac positioned in the region
lower segment caesarean section. CRL diameter
0,72 mm corresponding to 6-7 wga which is, fetal
pole was present, myometrium thickness 2 mm and
there was no free fluid in the pouch of Dauglas
(Figure 1-2).
She was in stable haemodinamic with a pulse
rate of 88/min and blood pressure of 120/70 mmHg.
Abdomen was large correspond to 6-7 wga.
Laboratory tests for complete blood count, ureum
and creatinine tests were within normal limit. Serum
HCG was 6625 IU/ml. Since the patient wished to
preserve her fertility, a conservative approach was
142
Irmayani, P. and Yeni, C.
Successful Methotrexate Therapy in Management Caesarean Scar, an Ectopic Pregnancy: A Case Report.
DOI: 10.5220/0008792501420144
In Proceedings of the 2nd Syiah Kuala International Conference on Medicine and Health Sciences (SKIC-MHS 2018), pages 142-144
ISBN: 978-989-758-438-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
implemented. Because of fetal cardiac activity was
still present, a local injection of NaCl 0,3 % into the
amniotic sac under ultrasound guidance resulted
embryonic demise. Following the local injection,
one doses of methotrexate were given intramuscular
methotrexate 50 mg/m
2
. Serial serum HCG values
were performed at weekly interval.
3 DISCUSSIONS
Ectopic pregnancy in a Caesarean scar was first
reported in 1978 by Larson and Solomon (Persadie
et al, 2005). The incidence of CSP has been
estimated to range from 1/1800–1/2216 and it
constitutes 6.1% of all ectopic pregnancies in
women with history of caesarean deliveries. The
pathophysiology is the invasion of the blastocyst in
the myometrium through minimal communication
between the previous cesarean scar and the
endometrial cavity (Vora and Bansal, 2017).
Risk factors include number of two or more
previous cesarean sections, previous dilatation and
curettage, other uterine surgery such as hysterotomy,
hysteroscopy and myomectomy, abnormal
placentation, previous manual removal of placenta,
short time interval between the cesarean delivery
and the current pregnancy and retroversion of the
uterus which may lead to greater cesarean scar
dehiscence, increasing the chance of implantation of
the gestational sac in this region (Persadie et al,
2005). In this patient we found that she had history
two or more previous cesarean sections.
The diagnosis of cesarean scar pregnancy was
confirmed if all of the following sonographic using
the following criteria (Vora and Bansal, 2017):
(1) The uterus was empty, with clearly demonstrated
endometrium;
(2) The cervical canal was empty, without
gestational sac or ballooning at the early
diagnosis;
(3) Presence of the gestation sac with or without a
fetal pole, with or without fetal cardiac activity
(depending on the gestation age) in the anterior
part of the isthmic portion of the uterus; and an
absence of normal myometrium between the
urinary bladder wall and the gestational sac.
(4) Color Doppler shows high velocity with low
impedance peri-trophoblastic vascular flow
clearly surrounding the sac.
(5) In early gestations (≤8 weeks), a triangular
gestational sac that fills the niche of the scar
and at ≥8 postmenstrual weeks this shape may
become rounded or even oval
(6) A thin (1-3 mm) or absent myometrial layer
between the gestational sac and the bladder
The exact etiology of cesarean scar pregnancy is
unknown. There are several hypotheses, proposed by
different authors. There was two different type of
cesarean scar pregnancy. First type of cesarean scar
pregnancy is an implantation of conceptus on prior
cesarean scar and it grows towards the
cervicoisthmic space or the uterine cavity. Second
type of cesarean scar pregnancy is a deep
implantation into a cesarean scar defect, and it grows
towards the urinary bladder and abdominal cavity.
Transvaginal ultrasonography with color Doppler is
very useful for diagnosis of cesarean scar
pregnancies. It must be distinguished from other
Figure 2. Transvaginal ultrasonography showe
d
gestation sac in the lower uterine segment and empt
y
uterine cavity and cervical canal.
Figure 2 Transvaginal ultrasonography showed fetaL
heart rate of the fetus.
Successful Methotrexate Therapy in Management Caesarean Scar, an Ectopic Pregnancy: A Case Report
143

types of abnormally implanted pregnancies,
including cervical, cervicoisthmic, and
cervicoisthmic corporeal pregnancies, as outcome
and treatment may differ in each (Sapana et al,
2014).
CSP has showed to respond well to it (dose of 50
mg/m2), especially in those with b-hCG levels <
5000 miu/ml. Conservative medical treatment is
appropriate for a woman who is pain free and
haemodynamically stable with an unruptured CSP of
<8 weeks of gestation and a myometrial thickness <
2mm between the CSP and the bladder (Ash et al,
2007). In this case we use MTX. MTX resulted in
resolution of cesarean scar pregnancy without
surgical intervention (Jain, 2014).
Till now no well defined guidelines are available
in literature regarding management of CSP.
Ultrasound guided intra amniotic Methotrexate
injection has been proposed as a method of choice
after treatment of 12 cases in a 6 year period (Jain,
2014).
4 CONCLUSSIONS
The early diagnosis of caesarean scar ectopic
pregnancy via transvaginal ultrasound is
fundamental for a successful conservative treatment.
Owing to their rarity, there is no consensus on
treatment regimens. The options are medical,
surgical or a combination of both methods.
REFERENCES
Sapana S, Rupa V, Rebecca E, et al. Management of
Cesarean Scar Pregnancy. IOSR Journal of Dental and
Medical Sciences 2014;13(9):12–7.
Cunningham FG, Lenevo KJ, Bloom SL et al. Williams
Obstetrics. 24 th Edit. Mc Graw Hill Education; 2014.
1240-1241 p.
Srinivas M, Ragupathy K, Ndumbe F. Dilemma in The
Management of Caesarean Scar Pregnancy. Reprod
Syst Sex Disord 2014;3(1):1–2.
Ross J, Interstitial & Scar Pregnancies. King’s College
Hospital, 2016;
Persadie RJ, Fortier A, Stopps RG. Ectopic Pregnancy in a
Caesarean Scar : A Case Report. J Obstet Gynaecol
Can
2005;1102–6.
Vora PH, Bansal V. Case Report Cesarean Scar
Pregnancy : Clinicians Challenge. Int J Reprod
Contracept Obstet Gynecol. 2017;6(5):2101–3.
Ash A, Smith A, Maxwell D. Caesarean Scar Pregnancy.
BJOG 2007;114:253–263.
Jain D. Caesarean Scar Pregnancy Managed by Scar
Resection – A Case Report and Algorithm for
Management. JSM Clin Case Rep 2014: 2(1): 1018
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
144
