
Association between Blood Absolute Eosinophil Count with the
Degree of Controlled Asthma
Desi Maghfirah
1
, T. Mamfaluti
2
, Islamuddin
3
1
Department of internal medicine, Faculty of medicine, University of Syiah Kuala, dr. Zainoel Abidin General Hospital,
Daud bereuh St, Banda aceh, Indonesia
2
Division of Alergy Immunology, dr. Zainoel Abidin General Hospital, Daud bereuh St, Banda aceh, Indonesia
3
Division of Pulmonology, dr. Zainoel Abidin General Hospital, Daud bereuh St, Banda aceh, Indonesia
Keyword: Absolute eosinophil count, ACT, PEFR
Abstract: Controlled asthma is the goal of asthma management. Blood eosinophils are known to be an indirect
marker of airway inflammation, it reflects asthmatic activity, but association with asthma control not clearly
understood. This study aims to investigate the association between blood absolute eosinophil count with the
degree of controlled asthma. An analysis observasional cross sectional study in 49 subject obtained through
out a consecutive sampling. The subject was examined physically, fill in ACT queistionnaire, and followed
PEFR test and blood test. The result were analysed using one way annova and unpaired T test. The 49
subjects were divided into three group based on ACT, 17 patients with uncontrolled, 16 not well controlled,
16 controlled and into two group based on PEFR, 38 with uncontrolled and 11 controlled. Mean differences
absolute eosinophil count between groups based on ACT is controlled vs not well controlled 212,6 (14,2-
411,1: p 0,003), controlled vs uncontrolled 373,9 (178,5-569,4: p <0,001), not well controlled vs
uncontrolled 161,3 (34,2-356,8: p 0,104). Mean differences absolute eosinophil count between groups based
on PEFR is controlled vs uncontrolled 419,8 (289,9-548,4: p <0,001). There were significant differences in
blood absolute eosinophil count between asthma control groups, better asthma control result in lower blood
absolute eosinophil count.
1 INTRODUCTION
Asthma is chronic inflammation disease that impact
social life, controlled asthma is the goal of asthma
management. The World Health Organization
(WHO) estimates 100-150 million people is
suffering from asthma, even this number is expected
to continue to grow up to 180,000 people every year.
Asthma prevalence increased by 50% every decade.
If not prevented and handled properly, then it is
expected that there will be a higher increase in
prevalence and disrupt the process of child growth
and quality of life of patients.
Blood eosinophils are known to be an indirect
marker of airway inflammation in asthma. It has
been suggested that blood eosinophil count reflects
asthmatic activity, but association with asthma
control not clearly understood. This study aims to
investigate the association between absolute
eosinophil count with the degree of controlled
asthma in asthma patient.
2 METHOD
We hypothesized there is a correlation between
blood absolute eosinophils count and the degree of
asthma control, the better the control of asthma, the
lower the number of blood absolute eosinophils.
An analysis observasional cross sectional study
in 49 subject obtained through out a consecutive
sampling since agustus -september 2015 in dr.
Zainoel Abidin Hospital Banda Aceh. Inclusion
criteria are age above 18 years, have been diagnosed
with asthma and willing to follow the research.
Parasitic infestation and acute pulmonary infection
were excluded. Patients who have been diagnosed
with outpatient asthma must perfomed stool
examination and chest radiographs. The subject was
examined physically, fill in ACT queistionnaire, and
followed PEFR test and blood test. If the subject has
value ACT ≤ 19 then is called uncontrolled asthma,
a value of 20-24 partially controlled asthma , the
value of 25 is totally controlled asthma.
Maghfirah, D., Mamfaluti, T. and Islamuddin, .
Association between Blood Absolute Eosinophil Count with the Degree of Controlled Asthma.
DOI: 10.5220/0008790000170022
In Proceedings of the 2nd Syiah Kuala International Conference on Medicine and Health Sciences (SKIC-MHS 2018), pages 17-22
ISBN: 978-989-758-438-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
17
Researchers explain how to use the HS755
peak flow meter and the patient is shown a video
recording how to use it and ensure that the patient
understands how to use the device. The patient
stands upright, inspire and place the mouth in the
mouthpiece tightly, the patient expires by blowing
strong and fast. The researcher assesses the number
in the indicator's place to stop, the examination is
repeated up to 3 times and the highest value is
recorded. The PEFR value of the patient is compared
with the predicted PEFR value. PEFR value <80%
prediction shows uncontrolled asthma.
Informed consent was requested in writing from
research subjects who were willing to participate in
the study after getting an explanation of the purpose
and objectives of this study.
The feasibility of research ethics was obtained
from the Faculty Ethics Feasibility Committee
Medicine Syiah Kuala University.
The analysis of the relationship of blood absolute
eosinophil count with the degree of asthma control
using ACT was done using one way anova, analysis
of the relationship of blood absolute eosinophil
count with the degree of asthma control using PEFR
was done using unpaired T test.
3. RESULT
In this study the proportion of asthma patients
aged at most 18-45 years (91.8%), female is 57.1%,
most of the subjects the study got the first attack of
asthma at the age of 0-11 years (55.1%), most
patients did not smoke (83.7%), with a history of
tendency most atopy (38.8%), with the most history
of drug use (49%) SABA (table 1).
Table 1: Baseline Characteristic
Characteristic n (%)
Age
- 18-45 years old
- ≥ 46 years old
Sex
- Man
- Women
First attack
- 0-11 years old
- 12-65 years old
Smoking
- Yes
- No
Atopy
- Rhinitis
- Dermatitis
- Mixed
- None
Dru
g
s
45 (91,8)
4(8,2)
21 (42,9)
28 (57,1)
27 (55,1)
22 (44,9)
8 (16,3)
41(83,7)
19 (38,8)
3 (6,1)
18 (36,7)
9 (18,4)
- SABA
- LABACS
- Metylxanthine
- SABA+ LABACS
- None
24 (49)
15 (30,6)
1 (2)
1 (2)
8 (16,3)
Characteristics of research samples when
grouped by degree asthma control using ACT, it was
found that the distribution of characteristics the
sample is the same in three asthma degree groups,
while if grouped based on the PEFR value, it was
found that in the uncontrolled asthma group it was
found older, had longer asthma, with an age of
attack first, younger, but this difference was not
statistically significant
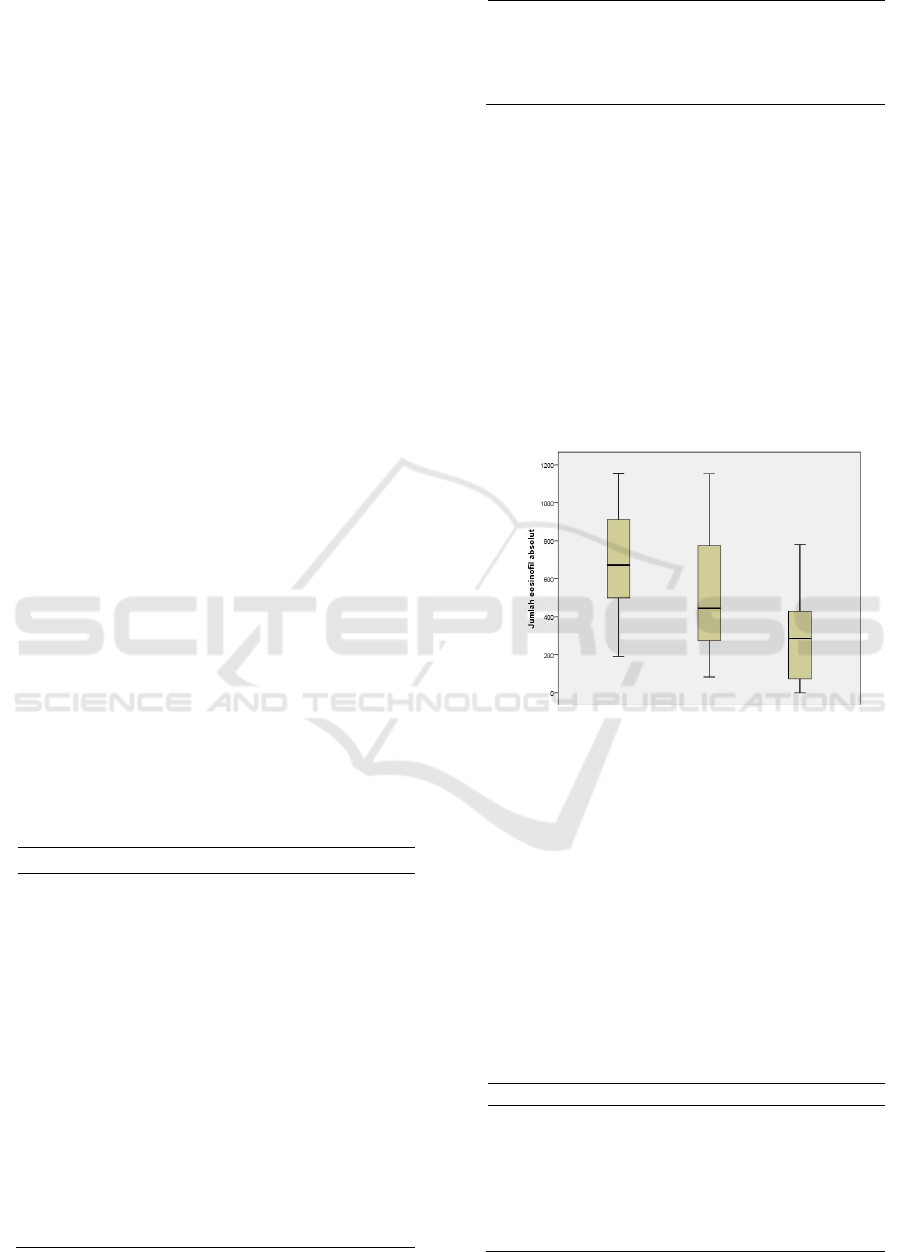
Absolute eosinophil counts in the lower total
controlled asthma group compared to the partially
controlled asthma group and uncontrolled asthma
(figure 1).
Figure 1: The Absolute eosinophil count of asthmatics
grouped by asthma control degree using ACT
One way annova test to see the correlation
between absolute eosinophil count and degree of
asthma control based on ACT found that there were
significant differences in mean eosinophil counts at
least in two asthma control degree groups, the better
the degree of asthma control, the lower the absolute
number of eosinophils (table.2 )
Table. 2 Mean Differences Absolute Eosinophil Count
Between Groups Based on ACT
N Means ± SD
p
Controlled
Asthma
16 305 ± 236,3 <
0,002
Partially
controlled
Asthma
16
518 ± 322
Uncontrolled
Asthma
17 679,3 ± 271,8
Absolute eo
sinophil count
Uncontroll
Partially
Controlled
Degree of asthma control (ACT)
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
18
There were significant differences in blood
absolute eosinophil count in the total controlled and
partially controlled asthma group, in the total and
uncontrolled controlled group, but the mean absolute
eosinophil count in the controlled group did not have
a significant difference compared to the uncontrolled
asthma group (table 3).
Table 3: One way Annova after post hoc LSD test Mean Differences Absolute Eosinophil Count Between Groups Based
on ACT
Mean
Differences
CI 95 % p
Minimu
m
Maximu
m
Controlled Asthma vs Partially controlled Asthma 212,6 14,2 411,1 0,003
Controlled Asthma vs Uncontrolled Asthma 373,9 178,5 569,4 < 0,001
Partially controlled Asthma vs Uncontrolled Asthma 161,3 34,2 356,8 0,104
Table 4: Association Between Absolute Eosinophil Count With The Degree Of Controlled Asthma based on PEFR
N Means ± SD Mean Differences ( CI 95 % )
P
Uncontrolled
Asthma
38 598,6 ± 285,9 419,8 (289,9-548,4) < 0,001
Controlled Asthma 11 179,4 ±144,2
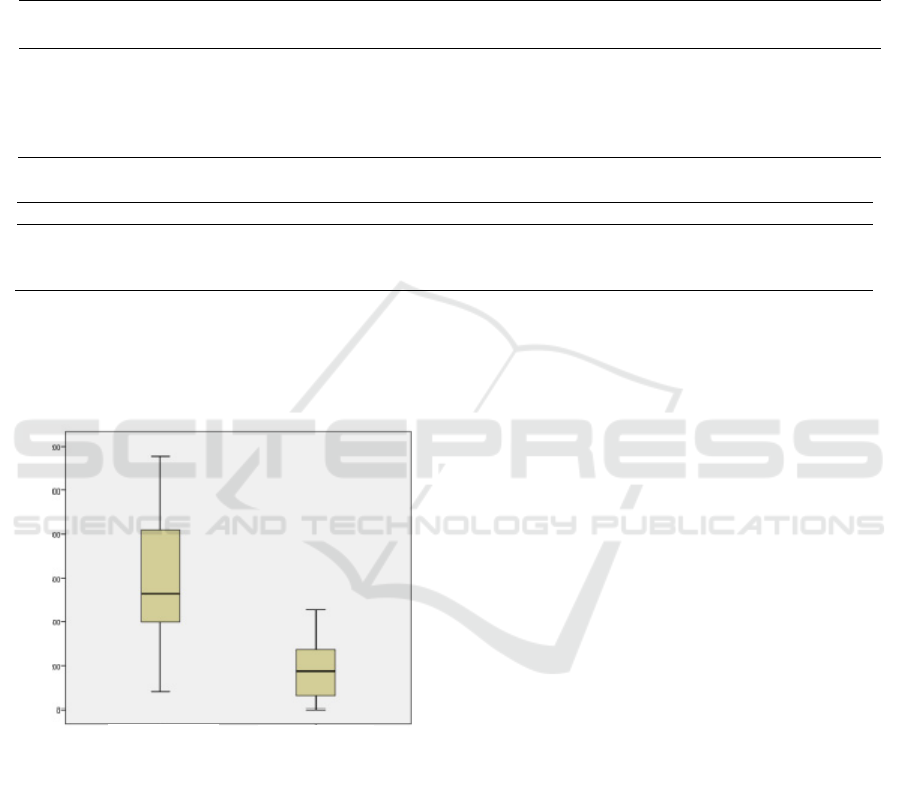
The blood absolute eosinophils count in the
controlled asthma group was lower compared to
the uncontrolled asthma group assessed according to
PEFR (figure 2).
Figure 2: The Absolute eosinophil count of asthmatics
grouped by asthma control degree using PEFR
In the unpaired T test to see the relationship
between blood absolute eosinophil count and asthma
control level based on PEFR, it was found that there
was a significant difference in the mean blood
absolute eosinophil count between controlled and
uncontrolled asthma groups, where the mean
absolute eosinophil count in the uncontrolled asthma
group was significantly lower than controlled
asthma group (table 4).
4. DISCUSSION
Thymus involution begins immediately after birth,
thymus involution causes the thymus volume to
decrease significantly after 45 years old and turn
into fat tissue, it finished approaching 60 years old.
As a result of this involution there is a decrease in
naiv T cells gradually and more memory T cells,
decreased activity T helper cell. The aging process
can also reduce the proliferative response, decreased
levels of CD8 + T cells, and changes in Th1 to Th2.
Changes to this immune system closely resembles
the effects of aging, so asthma progression in older
age it stands out and is heavier. In this study the
proportion of patients at 18-45 years (91.8%), and
those aged ≥ 46 (8.2%), it because asthma symptoms
at the age of ≥46 years heavier and the possibility of
the patient going to the emergency room,
temporarily the study was conducted in polyclinics.
Francisco et al's in 2010 was found that
proportion female asthma patients are > 65% with
aged 15-34 years. Research by Agarwal in 2006
concluded that women, old age, low socio-economic
status, history Atopy tendency, history of parents
with asthma, and smokers are risk factors for the
occurrence of asthma. Puberty is associated with
increased incidence of asthma in women while after
menopause the incidence of asthma is reduced, this
proves that the influence of endogenous hormones
and exogenous roles in asthma. In this study the
Absolute eosinophil count
Controlled
Uncontrolle
d
Degree of asthma control (PEFR)
Association between Blood Absolute Eosinophil Count with the Degree of Controlled Asthma
19

proportion of female is 57.1% and most patients do not smoking (83.7%).
Most patients get the first attack before 6 years
old. Boys get more asthma than girls, however at 11
years the prevalence is the same, while after 16
years of age, women (6.2%) were more likely to
suffer from asthma than boys (4.3%). The main risk
factors for asthma in children are, genetic
predisposition, history families with asthma or
allergies, history of parents with atopic disease,
respiratory infections, bacterial colonization, allergic
sensitization and exposure to cigarette race. Asthma
with adult onset varies from 12-65 years, compared
with the onset of children, adult onset still needs
investigation prevalence and risk factors In this
study most patients experienced the first asthma
attack before 12 years of age (55.1%).
One third to half of cases of asthma are caused
by atopy. Atopy can be proven by skin puncture
examination or examination IgE. In this study no
skin pricking tests were carried out IgE examination
so that the tendency of atopy is assessed based on
history history of complaints of patients associated
with atopy. In this research proportion of history of
atopy tendencies of 81% with most complaints of
rhinitis 38.8%, followed by rhinitis accompanied by
dermatitis by 36.7%, and 18.4% patients have never
had atopic complaints. Charpin et al and Wieringa et
al said that a history of atopy was associated with
asthma.
The absolute eosinophils counts increases in
circulation and is associated with asthma severity.
Research conducted by Yousry et al in 2012
Lonnkvist et al in 2001 showed that the absolute
eosinophils counts significantly higher in the asthma
group than in the group of people healthy (p
<0.001). A typical picture of asthma is an increase in
eosinophils peripheral blood. Peripheral blood
eosinophils correlate with the severity of symptoms,
levels limited air flow, and airway hypereactivity.
Suspected that blood eosinophils is an indirect
marker for airway inflammation in asthma. In this
study blood absolute eosinophil counts in the total
controlled group asthma lower than in the partially
controlled asthma group and are not controlled.
The results of this study are in accordance with
previous studies. Sele et al in 2001 found the
absolute eosinophils counts in uncontrolled asthma
hingher than patients with asthma controlled. Yousri
et al in 2012 was found that the absolute eosinophils
counts was significantly higher in patients asthma
with severe attacks compared with mild attack
patients. There is a relationship between the severity
of the asthma attack and the high number peripheral
absolute eosinophils. Fujitaka et all got that the
absolute eosinophils counts is significantly higher in
patients severe asthma compared to mild asthma.
Anna et al stated that asthma patients with high
absolute eosinophil counts have more treatment
background, more frequent exacerbations and worse
asthma control than patients with low blood absolute
eosinophils. Trung et al got the results showed that
patients who had high levels of blood absolute
eosinophils experience more asthma attacks often
compared to patients with absolute blood eosinophil
counts low. In this study it was found that there were
significant mean differences the blood absolute
eosinophils in the group of asthma was totally
controlled and controlled in part, in a total and
uncontrolled controlled group, but the average the
absolute eosinophils counts in a part of the
controlled group does not have significant difference
compared to uncontrolled asthma group.
There is a difference in the blood absolute
eosinophils between controlled and uncontrolled
asthma groups assessed using PEFR, where the
mean absolute eosinophil count in the asthma group
was not controlled more significantly lower than the
controlled asthma group. This discovery showed
that changes in blood eosinophils showed activity
diseases and the number of absolute eosinophils play
an important role in determine the degree of asthma
control.
5. CONCLUSION
There are significant differences in the number of
blood absolute eosinophils counts in asthma totally
controlled group and partially controlled, and
between total controlled and uncontrolled groups
assessed using ACT, the better the degree of asthma
control, the absolute number of eosinophils Getting
lower. There are differences in the number of
absolute eosinophils that are meaningful between a
group of controlled and uncontrolled asthma
assessed using PEFR, where the absolute number of
eosinophils in the asthma group is more controlled
significantly lower than uncontrolled asthma groups.
Increased numbers of absolute blood eosinophils are
associated with asthma not controlled.
REFERENCES
Ardinata D. Eosinofil dan patogenesa asma. Allergy Asthma
Clin Immunol.
2008;2(4):84-90.
Ballweg T, Bufford J, Busse W, Fliegel J, Jackson D, Kim M et
all. Diagnosis
and Management of Asthma -
Adult/Pediatric - Clinical Practice Guideline.
USA. 2013.
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
20

Barnes PJ. Pathophysiology of asthma. Eur Respir Mon, 2003, 23,
84-113.
Bernstein JA. Asthma in handbook of allergic disorders.
Philadelphia: Lipincott Williams & Wilkins. USA.
2003.73-102.
Bradding P. Asthma: eosinophil disease, mast cell disease, or
both? Allergy
Asthma Clin Immunol. 2008; 4(2): 84-90.
Busse W, Lemanske FR. Asthma, N Engl J Med, 344, 2001: 350-
62.
Davoodi P, Mahesh PA, Holla AD, Ramachandra NB.
Association of socio-
economic status with family history
in adult patients with asthma. Indian J Med Res
2013;138:497-503.
Departemen Kesehatan RI. Pedoman Pengendalian Penyakit
Asma. Depkes RI.
Jakarta. 2009.
Fujitaka M, Kawaguchi H, Kato Y, Sakura N, Ueda K, Abe Y.
Significance of
the eosinophil cationic protein/eosinophil
count ratio in asthmatic patients: its
relationship to disease
severity. Ann. Allergy Asthma Immunol. 2001; 86: 323 -9.
Gay BG, Parker K. Understanding the Complete Blood Count
With Differential. J of Peri Anesthesia Nursing.
2003;2(18):96-117.
Ghaffari J, Khademloo M, Saffar MJ, Rafiel A, Masiha E.
Hypersensitivity to
house dust mite and cockroach is the
most common allergy in north Iran. Iran J. Immunol.
2010;7:223-34.
Gibson PG, Saltos N, Borgas T. Airway mastcells and
eosinophils correlatewith clinical severity and airway
hyperresponsiveness in corticosteroid-treated asthma. J
Allergy Clin Immunol. 2000;105:752-9.
GINA. Global strategy for asthma management and
prevention. National
nstitutes of Health. Canada. 2007.
Green RH, Brightling CE, McKenna S, Hargadon B, Parker
D, Bradding P,
Wardlaw AJ, Pavord ID. Asthma
exacerbations and sputum eosinophil counts: a
randomised controlled trial. Lancet. 2002 Nov
30;360(9347):1715-21.
Hamid Q, Tulic MK, Liu MC, Moqbel R. Inflammatory
cells inasthma:
Mechanisms and implications for therapy. J
Allergy Clin Immunol. 2003;1:5-17.
Hamri R, Xenakis JJ, Spencer LA. Eosinophils in innate
immunity: an evolving story. Cell TissueRes. 2012;343:57-
83.
Humbert M, Kay AB. Chronic inflammation in asthma. Eur
Respir Mon,
2003;23:126-37.
Jia CE, Zhang HP, Yan LV, Liang R, Jiang YQ, Powell H et al.
Asthmacontrol
test/quistionnaire for assesing asthma
control: systematic review and meta-
analysis. J Allergy Clin Immunol. 2013 Mar;131(3):695-703.
Juniper EF, Gruffydd JK, Ward S, Svensson K. Validation,
measurement
properties and interpretation of the asthma
controll questionnaire in children. Eur Respir J 2010; 36:
1410-6.
Juniper EF, Bosquet J, Abetz L, Bateman ED. Identifying well
controlled and not
well controlled asthma using the
asthma control quistionnaire. Respir Med
2006;100: 616-
21.
Juniper EF, Svensson K, Mork AC, Stahl E. Measurement
properties and
i
nterpretation of three shortened version
of the asthma control quistionnaire.
Respir Med 2005; 99:
53-8.
Kikkawa,Y,Sugiyama K, Obara K, Hirata H, Fukushima Y,
Toda M, etal.
Interferon-alpha inhibits airway
eosinophilia and hyperresponsiveness in an
animal asthma
model. AsiaPac.Allergy 2012; 2: 256-63.
Koh I, choi IS. Blood eosinophil counts for the prediction of
the severity of
exercise-induced bronchospasmin asthma. J
resp med 2002;96, 120-5.
Kumar RK, Herbert C, Yang M, Koskinen AM, McKenzie AN,
Foster PS. Role of interleukin-13 in eosinophil
accumulation and airway remodelling in a mouse
model of chronic asthma. Clin Exp Allergy 2002; 32(7):
1104-11.
Lee YS, In KH. Immunopathogenesis of Asthma. Tuberc
Respir Dis. 2006
Apr;60(4):379-90.
Liang Z, Zhao H, Y, Li R, Dong H, Liu L, etal. Moderate
accuracy of peripheral
eosinophil count for predicting
eosinophilic phenotype in steroid naive non-
atopic adult asthmatics. Intern.Med. 2012;51:717-22.
Lonnkvist K, Hellman C, Lundahl J, Hallden G, Hedlin G.
Eosinophil markers in blood, serum, and urine for
monitoring the clinical course in childhood asthma:
impact of budesonide treatment and withdrawal. J.
Allergy Clin. Immunol.
2001;107: 812-7.
Molfino NA. Targeting of eosinophils in asthma. ExpertOpin.
Biol.Ther. 2012;
12:807-9.
Obase Y, Shimoda T, Mitsuta K, Matsuo N, Matsuse H, Kohno
S. Correlation
between airway hyperresponsiveness and
airway inflammation in a young adult
population:
eosinophil, ECP, and cytokine levels in induced
sputum. Ann.
Allergy Asthma Immunol. 2001;86: 304-10.
Pereira LMP, Boodoo S, Dindial KA, Hosein A, Seemungal
TAR, Bekele I.
Evaluation of asthma control using patient
based measures and peak expiratory
flow rate. West Indian Med J 2009; 58 (3): 214
Prussin C, Metcalfe DD. IgE, mast cells, basophils, and
eosinophils. J Allergy
Clin Immunol 2003;111:486 -94.
Quaedvlieg V, Sele J, Henket M, Louis R. Association between
asthma control
and bronchial hyperresponsiveness and
airways inflammation: a cross-sectional study in daily
practice. Clin Exp Allergy. 2009;39(12):1822-9.
Rahmawati I, Yunus F, Wiyono HW. Patogenesis dan
patofisiologi asma. Dalam: Cermin Dunia Kedokteran.
Jakarta. 2003;141:5-10.
Ramlie A, Soemarwoto RAS, Wiyono WH. Korelasi antara
asthma control test
dengan VEP
1
% dalam menentukan
tingkat kontrol asma. J Respir Indo. 2014;
34(2): 95-101.
Rengganis I, Diagnosis dan tatalaksana asma bronkial. Maj
Kedokt Indon. 2008;58 (11): 444-51.
Rigazio A. Raised blood eosinophil levels as an indicator of
prospective asthma
outcomes. dalam: Hoyle B, editor.
2013 Annual Meeting of the American
College of
Allergy, Asthma & Immunology. 2013 Nov 9-12. America.
2013.p53.
Saeed W, Badar A, Hussain MM, Aslam M. Eosinophils and
eosinophil products in asthma. J Ayub Med Coll
Abbottabad. 2002; 14(4): 49-55.
Spector SL, Tan RA. Is a single blood eosinofil count a
reliable marker for
eosinophilic asthma?. J.Asthma.
2012;49:807-10.
Spencer LA, Szela CT, Perez SA, Kirchhoffer CL, Neves JS,
Radke AL, etal.
Human eosinophils constitutively
express multiple Th1, Th2, and
immunoregulatory cytokines that are secreted rapidly
and differentially. J.
Leukoc. Biol. 2009;85:117-23.
Sundaru H, Sukamto. Asma bronkial. Dalam : Sudoyo AW,
Setiyohadi B. Alwi I. Simadribata M, Setiati S, editor. Buku
ajar ilmu penyakit dalam Jilid I. Edisi V.
Jakarta : Balai penerbit Fakultas Kedokteran Indonesia ;
2010. Hal 404-14.
Tran TN, Khatry DB, Ke X, Ward CK, Gossage D. High blood
eosinophil count is associated with more frequent asthma
Association between Blood Absolute Eosinophil Count with the Degree of Controlled Asthma
21

attacks in asthma patients. Ann Allergy Asthma Immunol.
2014;113(1):19-24.
Wardlaw AJ, Brightling C, Green R, Woltmann G, Pavord I.
Eosinophils in
asthma and other allergic diseases. Br Med
Bull 2000; 56:985-1003.
Wardlaw AJ. Eosinophil trafficking in asthma. Clin Med
JRCPL.2001;1:214-8.
Youroukova VF, Oddera S, Silvestri M, Spallarossa D,
Rossi GA. Blood
eosinophilia and degree of sensitization
to house-dust mites in preschool and
school children with
asthma. J. Asthma. 1998;35: 489-96.
Zohery YZA, Kenawy MA, Awad AA, Helmi N, Shafei AM,
Hamid YMA.
Levels of five biochemical parameters in
asthmatic patient’s blood as markers for
bronchial asthma induced by the house-dust mite allergy.
Egypt. Acad. J. Biolog. Sci. 2012; 4(1)
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
22
