
Invasive Amoebiasis in a Child:
A Case Report in Aceh Provincial Referral Hospital
Reno Keumalazia Kamarlis
1,2
1
Department of Anatomical Pathology, Universitas Syiah Kuala Banda Aceh, Indonesia
2
Department of Anatomical Pathology, Zainoel Abidin Hospital, Banda Aceh, Indonesia
Keywords: Amoebiasis, Enterocolitis, Histopathology
Abstract: Amoebiasis is throught to occur intraveller, immigrant from endemic areas and among men who have sex
with men. Amoebiasis, caused by parasite Entamoeba histolytica, has a worlwide distribution, with an
estimated 50 million people being infected. We present case of amoebic anal in a boy, 4 years-old with
diagnosed Enterocolitis until a punch biopsy disclosed a diagnosis Ameboetic. According to microscopic
result, the findings were typical characteristic of amoebiasis. This technique can detect the presence of dots
in the mucosa that contain many trophozoites and perform biopsy specimens for histopathological
examination to establish a definitive diagnosis.
1 INTRODUCTION
Amoebiasis is a common infectious disease in the
human digestive tract caused by a parasite infection,
Entamoeba histolytica. These parasites are generally
apathogenic microorganisms that live in the large
intestine of humans and some animals, but in certain
numbers can become pathogens by forming colonies
in the intestinal wall and penetrating the intestinal
wall causing ulceration.
Amoebiasis has a worldwide distribution with an
estimated 50 million people being infected. With
40.000-100.000 deaths reported annually, it is the
second leading cause of death from parasitic
diseases worldwide. High-risk areas include South
Asia, Southeast Asia, the Middle East, and South
America. According to (Shahrul Anuar et al., 2012),
amoebiasis prevalence in ethnic group in Malaysia,
as a developing country, is 18.6%. North Eastern
states of India has amoebiasis prevalence of 23.2%
(Nath et al., 2015). Indonesia as a fellow developing
country has a high incidence of amoebiasis, which is
10-18% (Andayasari, Lelly, 2011). The death rate
due to infectious diseases caused by amoebiasis was
ranked second after malaria. Diarrhea prevalence is
13% higher in rural areas compared to urban areas
(Balitbang Kesehatan Kemenkes RI, 2007).
In this report, the reviewed case is a 4-year-old
child diagnosed with enterocolitis, yet due to further
examination, it was found that the cause was
amoebiasis, infection of Entamoeba histolytica.
2 CASE REPORT
A boy, 4 years old, with fever, right upper quadrant
pain and has been diagnosed with enterocolitis. He
got medical treatment but the clinical manifestation
not better and he referred to pediatric surgery. In
physical examination there was a fistula near anal
and biopsy taken to confirm the diagnosis.
The macroscopic result, a gray white soft tissue
fragmented volume ± 0,5 cc, was received. Formalin
fixed paraffin embedded and Hematoxylin and Eosin
stained.
According to microscopic result, amoeba burrow
in lamina propria and cause tissue necrosis with
inflammation with scattered neutrophils. Ulceration
and the trophozoites of E. histolytica are resemble
macrophages sections revealed areas underlying
granulation tissue and focal collections of
histiocytes. Other findings were the subepithelium
clustered of spherical organisms showing a single
nucleus with prominent karyosome and cytoplasm
containing ingested red blood cells.
Kamarlis, R.
Invasive Amoebiasis in a Child: A Case Report in Aceh Provincial Referral Hospital.
DOI: 10.5220/0008788902010204
In Proceedings of the 2nd Syiah Kuala International Conference on Medicine and Health Sciences (SKIC-MHS 2018), pages 201-204
ISBN: 978-989-758-438-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
201
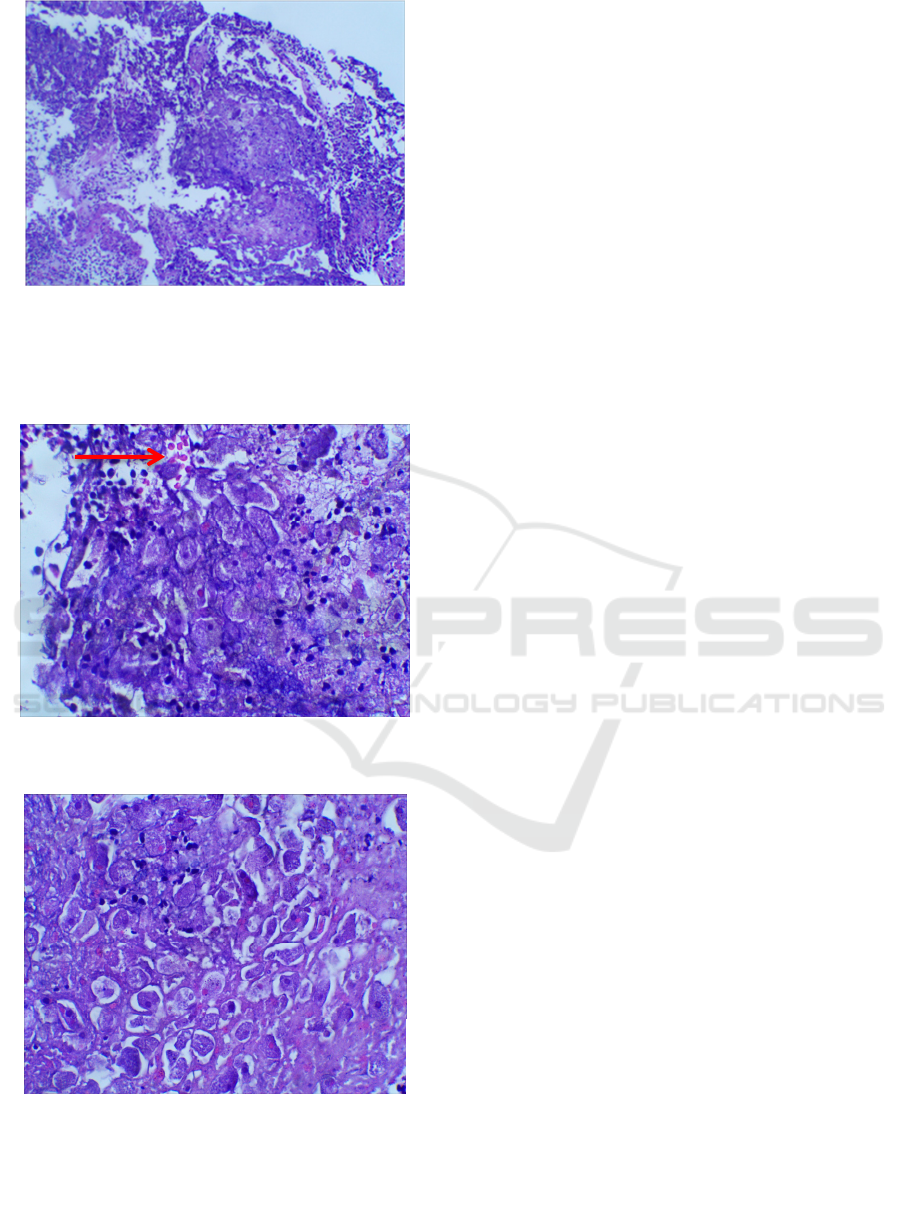
Figure 1. Tissue necrosis with inflammation with scattered
neutrophils, ulceration and the trophozoites of Entamoeba
histolytica are resemble macrophages sections revealed
areas underlying granulation tissue and focal collections of
histiocytes (100x magnification).
Figure 2. Single nucleus with prominent karyosome
containing ingested red blood cells (400x magnification).
Figure 3. Single nucleus with cytoplasm containing
ingested red blood cells (400x magnification).
3 DISCUSSION
Amoebiasis is an infection caused by protozoa
Entamoeba histolytica. Predominant spectrum of the
disease constitutes amoebic colitis and liver abscess.
This disease is strongly associated with poor
personal hygiene and environmental sanitation. The
socio-economic level of the community is one of the
factors that influence the sanitary conditions.
Research conducted by Shahrul Anuar et al. (2012)
in developing country, Malaysia, also stated that
housing conditions is a risk factor because it
indicates environmental sanitation in the area. The
risk of children infected by E. Histolytica will be
higher if the parents are carriers. This is in line with
the high prevalence of amoebiasis in children under
15 years old (Shahrul Anuar et al., 2012). E.
histolytica is second only to malaria as a protozoal
cause of death.
Worldwide the prevalence of amoebic infections
is estimated at 40-50 million with 40,000-110,000
deaths occurring annually. Most parts of Asia and
Africa are endemic for amoebic infection. In
developed countries infection occurs primarily
among travellers and immigrants to endemic
regions, homosexual males, immunosuppressed and
institutionalized individuals. Transmission is
predominantly by oro-faecal route (Dhingra et al.,
2007).
Some cases of Entamoeba histolytica infection is
asymptomatic, but there are also some cases that
show symptoms such as diarrhoea, dysentery,
fulminant colitis to extra intestinal amoebiasis which
can infect other organs such as liver, cardiac, lung,
cerebral, kidneys and other organs. According to
Pritt & Clark (2008), the life cycle of Entamoeba
histolytica begins with the entry of active cysts that
originate from feces into the human intestine, either
through contaminated food or drink or oral sexual
behaviour. In the large intestine, the cyst develops
and multiplies itself asexually into an active
trophozoite form and enters the mucosa of the large
intestine. Some active trophozoites are out with
feces and can survive in humid conditions for
several weeks or months. Active cysts that are
outside the human body are susceptible to
contamination with food, drinks or even other
humans so that the chain of infection continues to
repeat itself. Trophozoites that are still in the
intestinal mucosa are carried along with the blood
circulation system to the organs outside the large
intestine. This is what causes extraintestinal
amoebiasis. Extraintestinal amoebiasis often occurs
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
202

in the liver causing damage to the liver because liver
parenchymal cells are eaten by active trophozoites.
Mostly, people who infected with E. histolytica
is asymptomatic, the disease may occur within days,
months, or years after the infection, but the
condition will be worsen and can lead to colitis,
swelling and resembling a tumor in the large
intestine. Symptoms caused by E. histolytica
infection will be more progressive, begin from
abdominal pain, diarrhoea, bloody diarrhoea to
colitis. E. histolytica infection also occurs outside
the large intestine. The most common infected organ
is liver. Parasites are carried along with the
bloodstream. This causes pain in the right upper
quadrant pain and fever.
E. histolytica transmitted primarily through
ingestion of food or water contaminated with faecal
cysts. Transmission through faecal-oral can be
directly by person to person or indirectly by
consuming food or drink that contaminated by
faecal. Entamoeba histolytica can also communicate
through contamination of food or drinks through
vectors such as flies, cockroaches, and rodents.
Beside faecal-oral transmission, Entamoeba
histolytica has been recently recognised as an
emerging sexually transmissible pathogen in
homosexual (Escolà-Vergé et al., 2017). It often
found in the stool of homosexual men (Shelton).
Sexual transmission has also been reported,
particularly via contact with commercial sex
workers or in men who have sex with men (Gilroy et
al., 2018). This caused sporadic outbreaks in
countries where it is not endemic (Escolà-Vergé et
al., 2017). According to Shahrul Anuar et al., (2012)
the possibility of family members being infected by
Entamoeba histolytica is higher if the family
members themselves are the one who carried the
cyst and the transmission occurs between the family
members, because the cyst is more likely to become
infective.
Diagnosis can be done in several ways, including
faecal examination, culture, biopsy and
sigmoidoscopy, radiology and serology (Maryatun,
2008). Diagnosis with faecal examination is done to
find eggs, larvae and protozoa cysts using
concentration techniques. Culture is also one of the
techniques for diagnosing amoebiasis by making a
layer of liquid that is located on top of the basic
nutrient in a partial anaerobic state. Another
technique to diagnose amoebiasis is biopsy. This
technique can detect the presence of dots in the
mucosa that contain many trophozoites and perform
biopsy specimens for histopathological examination
to establish a definitive diagnosis. Radiology
techniques performed with the use of barium.
However, this technique cannot be used to examine
eggs and parasites. Another technique is serology,
which is primarily aimed for extraintestinal
amoebiasis diagnosis when stool examination shows
negative results.
Gross description discrete ulcers with normal
intervening mucosa may show areas of colitis or
inflammatory polyps. Histopathological examination
result of the fistulous tract and the curetted
granulation tissue shown the presence of multiple
trophozoites of E. histolytica exhibit
erythrophagocytosis in the background of mixed
inflammatory infiltrate.
Necrotic material admixed with mucin,
proteinaceous exudate and blood clot lining ulcers,
significant surface epithelial changes such as
shortening and tufting adjacent to sites of ulceration.
Mild chronic inflammation extending into the deep
mucosa and mild architectural alteration were
features of amebiasis. Trophozoite forms of amoeba
were seen in the necrotic material lining sites of
ulceration or lying separately, as well as over intact
mucosa.
Necrotic material lining ulcers was less common
in inflammatory bowel disease. The chronic
inflammation crypt abscess formation and
architectural alteration were more severe (Singh et
al., 2015). Typically, the parasites are surrounded by
an artifactually clear space. They are round or ovoid,
measure 6-40 nm in diameter, and contain abundant
cytoplasm with a distinctive vacuolated appearance
and relatively small. They also perfectly round
nuclei with prominent nuclear borders and central
karyosome. Erythrocytosis by trophozoites is usually
present (Rosai, 2004). The cytoplasm is vacuolated
which leads to confusion with macrophages
(Dhingra et al., 2007). The presence of trophozoites
containing red blood cells is indicative of tissue
invasion Adequate sampling and step sections are
very important to get true diagnosis.
4 CONCLUSION
A boy, 4 years old, with fever, right upper quadrant
pain confimed as a case of amoebiasis. Diagnosis
can be done in several ways, including biopsy.
According to microscopic result, amoeba burrow in
lamina propria and cause tissue necrosis with
inflammation with scattered neutrophils. Ulceration
and the trophozoites of E. histolytica are resemble
macrophages sections revealed areas underlying
granulation tissue and focal collections of
Invasive Amoebiasis in a Child: A Case Report in Aceh Provincial Referral Hospital
203

histiocytes. Other findings were the subepithelium
clustered of spherical organisms showing a single
nucleus with prominent karyosome and cytoplasm
containing ingested red blood cells. This technique
can detect the presence of dots in the mucosa that
contain many trophozoites and perform biopsy
specimens for histopathological examination to
establish a definitive diagnosis.
ACKNOWLEDGEMENTS
Department of pathology and anatomical Zainoel
Abidin Hospital, Banda Aceh, Indonesia.
REFERENCES
Andayasari, Lelly, A., 2011. Epidemiological studies of
gastrointestinal infections caused by amoeba in
indonesia. Media Litbang Kesehatan, 21(1), pp. 1–9.
Balitbang Kesehatan Kemenkes RI, 2007. Basic health
research 2007, Laporan Nasional 2007.
Dhingra, K. et al., 2007.
Amoebic cervicitis mimicking
cervical carcinoma: a rare presentation. Iranian
Journal Of Pathology 3(1).
Escolà-Vergé, L. et al., 2017. Outbreak of intestinal
amoebiasis among men who have sex with men,
Barcelona (Spain), October 2016 and January 2017.
Eurosurveillance, 22(30), pp. 1–4.
Gilroy, N. et al., 2018. A 12-year retrospective study of
invasive amoebiasis in western sydney: evidence of
local acquisition. Tropical Medicine and Infectious
Disease, 3(3), p. 73.
Maryatun, 2008. Entamoeba histolytica : parasit causes
intestinal and liver amoebiasis. Kedokteran Syiah
Kuala, 8(1), pp. 39–46.
Nath, J. et al., 2015. Molecular epidemiology of
amoebiasis: a cross-sectional study among north east
indian p;opulation. PLoS Neglected Tropical Diseases,
9(12), pp. 1–19.
Pritt, Bobbi S. and Clark, C. G., 2008. Amebiasis. Mayo
Clinic Proceedings, 83(10), pp. 1154–1160.
Rosai, J., 2004. Rosai and ackerman's surgical pathology.
Mosby. USA, 9
th
edition.
Shahrul Anuar, T. et al., 2012. Prevalence and risk factors
associated with entamoeba
histolytica/dispar/moshkovskii infection among three
orang asli ethnic groups in malaysia. PLoS ONE,
7(10).
Singh, R. et al., 2015. The differentiation of amebic colitis
from inflammatory bowel disease on endoscopic
mucosal biopsies. Indian Journal of Pathology and
Microbiology, 58(4), pp. 427–432.
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
204
