
Management for Dengue Hemorrhagic Fever
in Pregnancy: A Case Report
Rajuddin
1
, Lutfi Nogroho
2
1
Division of Reproductive Endocrinology & infertility, Department Obstetric & Gynecology, university of Syiah Kuala,
Banda Aceh ,Indonesia
2
Department Obstetric & Gynecology, university of Syiah Kuala, Banda Aceh ,Indonesia
Keywords: Dengue Hemorrhagic Fever, pregnancy, thrombocytopenia
Abstract:
Dengue hemorrhagic fever is a common tropical disease in Indonesia. Nowadays, the incidence
has been increasing among adults and more cases of dengue fever and dengue hemorrhagic fever
in pregnancy are being reported. We managed one case of dengue hemorrhagic fever during
pregnancy which developed during antepartum periods. We diagnosed dengue hemorrhagic fever
during pregnancy with clinical pictures of fever, hem concentration, thrombocytopenia and
serological test. This case was treated conservatively. The patient has recovery and has already
discharged. The patient came again after 3 days with chief complaint water broke history
previous C section, so we decided to perform emergency C Section. Patient and the baby were in
good condition before discharged. Where dengue is endemic, dengue infection should be highly
suspected in cases of febrile pregnant women. A knowledge of its diagnosis and management
plays a vital role for an obstetrician, particularly regarding to the mode of delivery. Supportive
care with analgesics, bed rest, adequate fluid replacement and maintenance of electrolyte balance
forms the main stay of treatment. The management of most cases was conservative.
1 INTRODUCTION
Dengue fever has become a major health problem
especially in tropical countries. Nowadays, the
incidence has been increasing among adults and
more cases of dengue fever and dengue hemorrhagic
fever in pregnancy are being reported. Dengue
infection in pregnancy increases the risk of
haemorrhage for both the mother and the newborn.
Increased incidence of preterm births and fetal
deaths has been reported due to dengue infection in
pregnancy.(Undurraga,2015) In the literature only
about 400 cases of dengue during pregnancy have
been reported, mainly describing the maternal and
fetal outcomes.(Paixao,2016)
Diagnosis of dengue
infection affects obstetric management, particularly
the mode of delivery due to the potential risk of
haemorrhage secondary to thrombocytopenia. A
knowledge of its diagnosis and management plays a
vital role. We report a case of dengue fever in
pregnant woman 36 weeks gestational age with
history previous C section.
Dengue, a mosquitos-borne flavivirus infection,
is hyperendemic in Indonesia. Dengue hemorrhagic
fever is a leading cause of hospitalization of children
in Southeast Asia. During the past three decades in
Indonesia. A number of patients who have dengue
hemorrhagic fever has increased by several years.
Hence, one should be aware of an increase in
incidence of the infection during pregnancy. We
managed one patient who developed dengue
infection during third trimester. She was admitted to
the Zainoel Abidin general hospital Banda Aceh and
serologic test showed primary dengue infection. The
effect on pregnancy and management are discussed
here.
2 CASE REPORT
A 21-year- old, gravida 2 woman who had been a
life long citizen Banda aceh was hospitalized in at
36 weeks gestational age with previous c section 1
time. She had undergone high fever for 3 days and
epistaxis associated with malaise. She was admitted
Rajuddin, . and Nogroho, L.
Management for Dengue Hemorrhagic Fever in Pregnancy: A Case Report.
DOI: 10.5220/0008788601830187
In Proceedings of the 2nd Syiah Kuala International Conference on Medicine and Health Sciences (SKIC-MHS 2018), pages 183-187
ISBN: 978-989-758-438-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
183

9 month of pregnancy, acording to last menstrual
period correspond due to 36 weeks gestational age
(wga). Patient did ANC regularly every month at
Obgyn. She went to the Obgyn for ultrasound her
pregnancy 4 times. The last ultrasound 2 weeks ago
said that the estimation fetal weight about 2000
gram, mother and fetal was in good condition. she
complained of high fever with petechiae at both
hand and headache that began 1 days prior to
admission at the Zainoel Abidin Hospital Banda
Aceh. She complained epistaxis before she came to
the Hospital. She developed epigastric pain and
vomitting. She also has spontaneous bleeding from
her nose, headache, tenderness in both leg and
epigastric pain, defecation and mixturition within
normal limit. She didnt complaint contraction, blody
show and water broke. no have flu symptomp. no
history of fluor albus. Active fetal movement.
On examination patient was conscious. She was
febrile 39.1 Celsius degrees. Her heart rate was
120/min, blood pressure was 110/70mmhg,
respiratory rate was 21 breaths/min. pulse rate was
120/min. Lungs were clear and no cardiac murmurs
were noted. She was started Intense fluid
resuscitation.( Normal saline) Bolus of 5-10
ml/kg/hour 1-2 hours given followed by 3-5
ml/Kg/Hour as a maintainance. Paracetamol 500 mg
and Ranitidine for epigastric pain. she was treated
with antipiretic drugs for 2 days.The fundal eight
was compatible with 36 weeks gestational age. The
fetal hearth rate was reassuring. Petechiae sized 1-2
mm in diameter were found around the arms.
Her hemoglobin was 10.3 g/dl; Hct 32%; TLC
11.000 cells/cumm; platelet count 108,000
cells/cumm; SGOT(315U/L) and SGPT (15U/L);
NS1Ag negative and IgG and IgM for dengue were
positive. Laboratory findings included the highest
level of hemoglobin concentrations 0f 10.7 g/dl,
hematocrit of 34% , and the lowest platelets of
35.000 on the fifth day. other laboratory findings
were within normal limit. She was diagnosed as
having dengue hemorrhagic fever grade II during
pregnancy and treated with intravenous fluid
replacement and close monitoring of vital sign and
laboratory every 12 hours. After 2 days admission,
the epigastric pain dissapeared and the vital signs
were within normal limits. On the sixth day, the
patient gradually recovered and the hematocrit was
32% with platelet count 45.000. on the ninth day the
platelet count 125.000 She was discharged on the
tenth day. Serologic study indicated primary Dengue
infection. At 37 weeks gestation, she came with
water broke. We decided to perform emergency C
section because history previous C section. Born a
healthy male baby weighing 2650 grams by C
section with an APGAR score at 1 min 9, and 5 min
of 10. No abnormality was detected.
3 DISCUSSION
Treatment and outcome of dengue in pregnant
women are similar to those of nonpregnant women.
Misdiagnosis or delayed diagnosis are often because
of the overlapping clinical and/or laboratory
features. The clinical and laboratory features are
similar with other disease that accompanied the
pregnancy. For examples HELLP syndrome,
pneumonia, pulmonary embolism, various obstetric
causes of pervaginal bleeding and other infectious
diseases.(Friedman,2016) Adverse pregnancy
outcome is still uncertain whether dengue is a
significant factor for adverse
Pregnancy outcomes such as preterm birth, low-
birth weight and caesarean deliveries. The risk of
vertical transmission is well established among
women with dengue during the perinatal period.
Significant impact of dengue at parturition are
severe bleeding may complicate delivery and/or
surgical procedures that performed on pregnant
patients with dengue during the critical phase, i.e.
the period coinciding with marked
thrombocytopenia with or without plasma leak.
Dengue fever does not warrant termination of
pregnancy. There is insufficient data of Probable
embryo developmental disorder to mothers who had
Dengue infection in first trimester.(Ribeiro,2015)
If delivery is inevitable, bleeding should be
anticipated and closely monitored. Blood and blood
products should be cross-matched and saved in
preparation for delivery. Trauma or injury should be
kept to the minimum if possible. It is essential to
check for complete removal of the placenta after
delivery. Transfusion of platelet concentrates should
be initiated during or at delivery but not too far
ahead of delivery, as the platelet count is sustained
by platelet transfusion for only a few hours during
the critical phase. Fresh whole blood/fresh packed
red cells transfusion should be administered as soon
as possible if significant bleeding occurs. If blood
loss can be quantified, it should be replaced
immediately. Do not wait for blood loss to exceed
500 ml before replacement, as in postpartum
haemorrhage. Do not wait for the haematocrit to
decrease to low levels. Oxytocin infusion should be
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
184
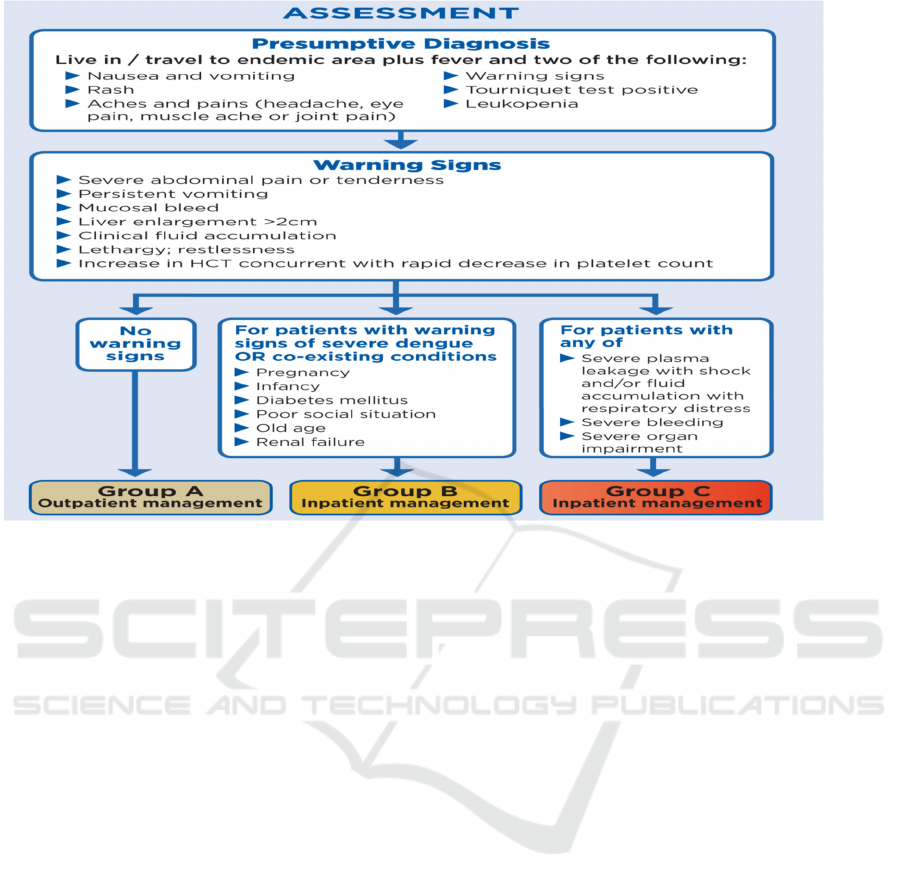
Figure 1: Dengue case management modified from WHO guideline for Dengue Hemorrhagic fever
given for uterine contraction after delivery to
prevent postpartum haemorrhage. Misoprostol may
be given for post partum hemorrhage
Prophylaxis/treatment. Intramuscular injections are
to be avoided.(Chitra,2015)
2.3 Management of dengue hemorrhagic
fever in pregnancy
All pregnant patients with suspected DHF are
advised for close monitoring.
DF without warning signs: (Group
A).(Friedman,2016)
Monitor:
• 4 hourly Temperature charting , pulse,
Blood Pressure and Pulse pressure.
• Ensure urine output at least 4-6 hours.
• ( minimum 100 cc every 4 hours)
• Capillary refill Time
• Intake Out put record.
• Labs : Daily Complete Blood Count ,
other investigations if necessary.
Treatment:
•
Paracetamol 500-650 every 6 hours.
Warn the patient that fever may not
settle with this dose but NOT to exceed 4
grams paracetamol in 24 hours. Nor to take
other NSAID like ibuprofen and diclofenac
Sodium.
• Oral Intake encouraged such as Oral
rehydration solution, coconut water, Kanji,
juice all are encouraged apart from routine
food. Aim of at least 2.5 litres. If
Nausea/Vomitting of pregnancy restrict
oral intake give IV fluid (NS) 100 cc/ hour.
(Friedman,2016)
Doctor on duty should be notified if : less
Urine output, vomiting, lethargy, narrowing of
pulse pressure, delayed capillary refill.>2
seconds Warning symptoms and signs for
capillary leak are to be looked for vigilantly
specially so when fever starts subsiding. As
warning signs hallmarks capillary leak and she
can progress to severe Dengue .These are
patients for IV fluid therapy.(Chitra,2015)
• Abdominal pain and tenderness
• Persistent vomiting
• Lethargy, restlessness
• Liver enlargement >2 cm , Capillary refill
getting delayed. UOP less
• Mucosal Bleed : epistaxis, gum bleed
petechiae.
• Rise in HCT (20% of baseline)
• DHF with Warning sign (Group
B).(Friedman 2016)
Management for Dengue Hemorrhagic Fever in Pregnancy: A Case Report
185
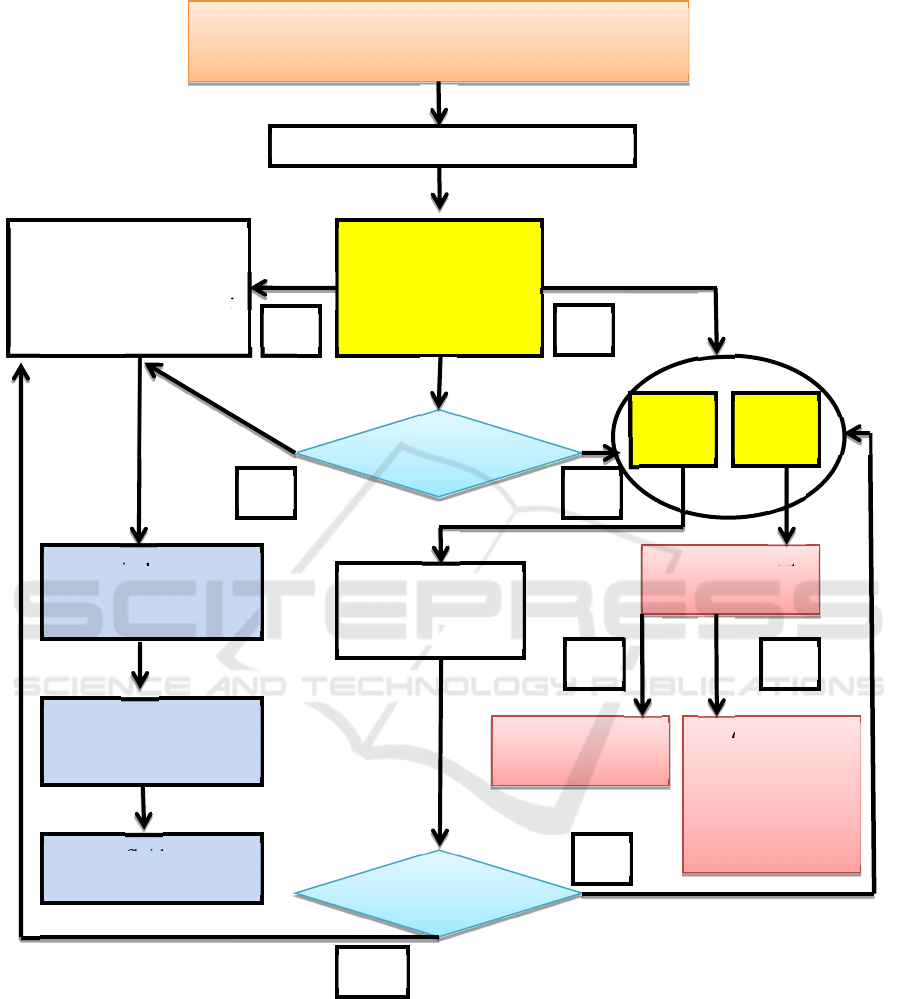
Figure 2: Treatment Algorithm for Dengue Hemorrhagic Fever in pregnancy modified from WHO Guideline
Check vitals sign every hours. Catheterize to
know precise urine output hourly ( Aim
0.5ml/kg/hour). Intense fluid resuscitation.( Normal
saline) Bolus of 5-10 ml/kg/hour 1- 2 hours given
followed by 3-5ml/Kg/Hour as a maintenance. This
is monitored by urine output and Pulse pressure.
Avoid induction of labour/ planned surgery in this
phase.(Ribeiro,2015)
DHF with shock on admission (Group C), these
patients need institutional management in ICCU
setup. Timely fluid management with appearance of
any warning symptom practically prevents further
Compensated shock
(Systolic pressure maintaned, Narrow pulse pressure)
N
ormal saline 5-10 ml/k
g
/hr for 1
Improvement in
vitals pulse volume
capillary refill temp
0f extrimities
Reduce sline gradually
5-7ml/kg/hr for 1-2 hr
3-5ml/kg/hr for 2-4 hr
2-3 ml/kg/hr for 2-4 hr
yes
No
2nd bolus of normal
saline10-20 ml/kg/hr
Improvement
HCT
High
Severe overt
bleed
Colloid 10-20
ml/kg/hr evaluate
to consider blood
transfusion if no
clinical
improvement
Urgent blood
transfusion
HCT
Low
yes No
No
Improvement
As clinical movement
is noted, reduced fluids
accordingly
Further boluses may be
needed for next 24-48
hours
Stop IV fluids at 48
hours
yes
yes
No
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
186

complication before transferring this
patient.(Chitra,2015)
• Draw blood for CBC, to know HCT.
• Also for group cross match, SGOT,SGPT,
Electrolytes, sugar etc.
• Fluids Bolus given as (NS) 10cc /kg over
15 minutes before transfer
• And second bolus as 10ml/kg for next 1
hour during transfer
.
• Hand over all reports , fluid bolus
details for reference for further
treatment.
Prophylactic platelet transfusion is NOT
recommended unless delivery is inevitable ( in
coming 6 hours) platelet count > 50000/CC, and
75000/cc for operative delivery. Clinically stable
Dengue with Low or very Low platelet count in
critical/recovery phase didn’t need platelet
transfusion. Platelet transfusion may be given in
presence of Overt bleeding with Low platelet counts.
Platelet transfusion was generally avoided unless
there was significant bleeding or platelet counts less
than 20.000.(Schexneider,2015)
Operative delivery for obstetric indications only.
Avoid Planned induction and surgery. The presence
of wounds or trauma during the critical phase of
dengue with marked thrombocytopenia, and plasma
leak creates a substantial risk of severe
haemorrhage. Delivery should take place in a
hospital where blood/blood components and a team
of skilled obstetricians and a neonatologist are
available.(Kariyawasam,2016)
4 CONCLUSIONS
Dengue fever in pregnancy most often is treated
conservatively. Platelet count may fall rapidly but no
active intervention required unless patient is in
labour or has bleeding disorder. Dengue infection in
pregnancy may have resulted in maternal morbidity
and mortality. Gestational age of occurrence of
dengue fever seems to have a role early or late in
pregnancy had a poor prognosis. Treatment for
dengue infection in pregnancy is supportive and
need attention to fluid balance, maintaining
normothermia, platelet count and monitoring for
shock and consideration of delivery management.
Severe thrombocytopenia requiring initial
resuscitation with blood and blood products prior to
and during delivery. Platelet transfusion may be
given in presence of Overt bleeding with Low
platelet counts. Platelet transfusion was generally
avoided unless there was significant bleeding or
platelet counts less than 20.000. A thorough
investigation should be conducted so as to confirm
the infection and prevent further maternal and fetal
complications.
REFERENCES
Guzman, G., J. Gubler, A. Izquierdo, E. Martinez, and S.
B. Halstead., 2016. Dengue infection. Nature Reviews
Disease Primers., 2: 55-60
Guzman,G.J., E. Harris.,2015. Dengue. The Lancet. 385
(96): 453–465.
Unduraga, E. A., M. Betancourt-Cravioto, J. Ramos-
Castañeda et al., 2015. Economic and Disease Burden
of Dengue in Mexico. PLOS Neglected Tropical
Diseases. 9 (3): 347-354.
WHO., 2014 Dengue Haemorrhagic Fever: Diagnosis,
Treatment, Prevention and Control. World Health
Organization, Geneva, Switzerland.
Paixao, E. S., G. Teixeira, M. D. C. N. Costa, and L. C.
Rodrigues.,2016. Dengue during pregnancy and
adverse fetal outcomes: A systematic review and meta-
analysis. The Lancet Infectious Diseases. 16(7): 857–
865.
Friedman, E. E., F. Dallah, E. W. Harville et al. 2016.
Symptomatic dengue infection during pregnancy and
infant outcomes: a retrospective cohort study. PLOS
Neglected Tropical Diseases. 8(10); 58-64
Ribeiro, C. F., V. G. Lopes, P. Brasil et al., 2015. Dengue
during pregnancy: association with low birth weight
and prematurity. 58(6): 64-72
Chitra, T. V., Chitra and S. Panicker.,2015. Maternal and
fetal outcome of dengue fever in pregnancy. Journal of
Vector Borne Diseases. 48(4): 210–213.
Schexneider, K. I., E. A. Reedy., 2015. Thrombocytopenia
in dengue fever. Current Hematology Reports. (2):
145–148
Kariyawasam, S., H. Senanayake.,2016. Dengue infections
during pregnancy: case series from a tertiary care
hospital in India. The Journal of Infection in
Developing Countries. 4( 11): 767–775.
.
Management for Dengue Hemorrhagic Fever in Pregnancy: A Case Report
187
