
Retinal Vasculitis in Patients with Positive TB Testing in Aceh
(Indonesia): A Case Series
Lia Meuthia Zaini
1,2
1
Department of Opthalmology, Faculty of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia
2
Department of Opthalmology, Dr.Zainoel Abidin Hospital, Banda Aceh, Indonesia
Keywords: Retinal Vasculitis, Vitreous hemorrhage, Eales disease
Abstract: Retinal vasculitis is a group of diseases characterized by inflammation of the retinal blood vessels. Although
many retinal vasculitis are unknown, many systemic diseases are associated with this diseases such as
tuberculosis (TB), Lyme disease, syphilis, toxoplasmosis, or viral infection. Retinal vasculitis can also be
part of posterior uveitis. One of the most frequent cause of retinal vasculitis is TB, which often referred to as
Eales disease. This disease is very rare in developed countries and more often found in countries with poor
economic levels. In Aceh (Indonesia), the disease is quite common, but it has never been reported. Several
theories have been proposed to explain the etiology of this diseases. Hypersensitivity to tuberculo-protein is
the most common theory reported about the possible etiology of Eales disease. It is based on the positive
results of Mantoux reactions in Eales patients. However, Mantoux examination can be positive in 67-90% of
healthy adults in India (and possibly other developing countries including Indonesia). The author report 3
cases of Eales diseases with recurrent vitreous hemorrhage as the first manifestation, in patients with
positive TB testing in Aceh. We also provide a brief review of the literature.
1 INTRODUCTION
Retinal vasculitis is a group of diseases
characterized by inflammation of the retinal blood
vessels. Although many retinal vasculitis are
unknown (idiopathic), many systemic diseases are
associated with this diseases such as tuberculosis
(TB), Lyme disease, syphilis, toxoplasmosis, or viral
infection. In addition, retinal vasculitis can also be
part of posterior uveitis. One of the most frequent
cause of retinal vasculitis is TB, and Eales disease is
a vasculitic disease of the retina that is often
associated with TB.
2 CASE 1
A 40-year-old male presented to our outpatient
department with blurred vision of the left eye for 1
week. He had a history of hypertension. There were
no history of trauma, other systemic diseases, or
long-term drug use. Visual acuity was normal on
right eye and 5 CF on left eye. Ocular examination
revealed normal anterior segment of both eyes with
vitreous bleeding on the left eye.
We suggested the patient to have laboratory
testing and chest x-ray with no initial treatment. The
patient came a week later with a strong positive
result of Mantoux test (induration of more than 15
mm). We thought about Eales disease, and provided
oral steroid therapy as well as photocoagulation
lasers. One week later, vitreous bleeding began to
subside. We continued steroid treatment, and ask the
patient to come within 1 month.
One month later, bleeding has reduced. Visual
acuity of the both eyes were 6/6. Slit lamp bio
microscopic examination with super field lens
showed minimal hemorrhage and vasculitis on the
peripheral retina.
Six months later, the patient came again,
complaining of floaters on both eyes. Ocular
examination revealed minute vitreous bleeding in
the right eye. Minimal retinal hemorrhage and
vasculitis were found on the peripheral retina.
178
Zaini, L.
Retinal Vasculitis in Patients with Positive TB Testing in Aceh (Indonesia): A Case Series.
DOI: 10.5220/0008788501780182
In Proceedings of the 2nd Syiah Kuala International Conference on Medicine and Health Sciences (SKIC-MHS 2018), pages 178-182
ISBN: 978-989-758-438-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
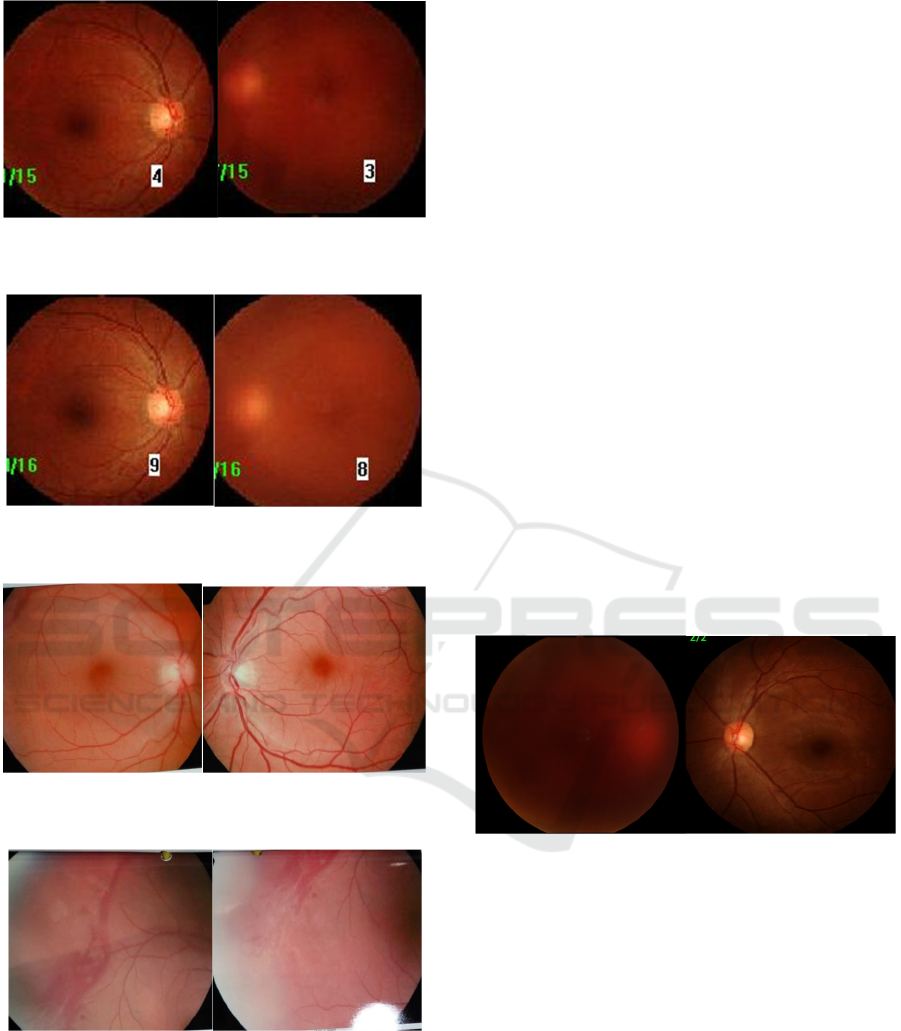
Figure 1. Vitreous hemorrhage of the left eye; right eye
was within normal limit
Figure 2. Vitreous hemorrhage of the left eye begins to
subside
Figure 3. Minimal vitreous bleeding of the right eye six
months later, the left eye was clear
Figure 4. Retinal hemorrhage and vasculitis in far
periphery of the retina detected after vitreous hemorrhage
resolved
We again prescribed oral steroid therapy and
planned PCR test. One week after that vision
improve with minimal vitreous hemorrhage. We
referred the patient to Jakarta for diagnosis
confirmation and PCR test. The patient returned 3
weeks later with 6/6 visual acuity on both eyes.
Vitreous was clear with retinal hemorrhage. PCR
results for TB was negative and OCT examination
revealed normal foveal contour of the both eyes. We
suggested bimonthly examination to the patient.
Two months later the patient came with vitreous
hemorrhage on the left eye. We decided to observe
him for 1 one month before prescribing anti-
tuberculosis drug. The condition improved on the
following 6 months with minimal complaint for
floaters.
3 CASE 2
A 19-year-old male patient came with complaint of
recurrent blurred vision of the right eye about 1
month earlier. No history of trauma and other
systemic disease. The patient noted that condition
always improved without medications.
Ophthalmological examination revealed visual
acuity of hand motion on the right eye and 6/6 on the
left eye. Anterior segment of both eyes was within
normal limits. We found severe vitreous hemorrhage
of the right eye. Ultrasound examination showed no
retinal detachment.
Figure 5. Dense vitreous hemorrhage in the right eye
We performed radiological and laboratory tests
available at our hospital, provided anti thrombolytic,
and advised him to rest in semi-fowler position. One
week later the patient came with normal laboratory
results and chest x-rays, except for positive Mantoux
test with induration of more than 15 mm. Vitreous
bleeding remains the same, there was no significant
increase in vision. We diagnosed the patient with
Eales' disease and prescribed prednisone 1 mg / BW
with 10 mg tapering off weekly. After 1 month
observation, there was no improvement. The patient
was referred to undergo vitrectomy surgery. He
returned two months later with clear vitreous,
attached retina with giant vessels, minimal retinal
hemorrhage, and laser scars on peripheral retina.
Retinal Vasculitis in Patients with Positive TB Testing in Aceh (Indonesia): A Case Series
179
The patient returned two years later with the
same complaint but on the left eye. Visual acuity
was hand movement with dense vitreous
hemorrhage found on the left eye. We proposed
diagnostic workup that he eventually refused
because he preferred to consult overseas.
4 CASE 3
A 38-year-old man presented with 1 week of blurred
vision of the left eye. Initially he saw black spots.
He reported no pain, redness, and lacrimation. There
is no history of trauma and other systemic diseases.
The patient had a history of gradually blurred vision
and metamorphopsia of his other eye about one year
earlier. He was diagnosed with Branch Retinal Vein
Occlusion (BRVO) of the right eye and received
intravitreal anti-Vascular Endothelial Growth Factor
(VEGF) injection twice. He did not undergo any
laboratory test at that time. As the complaint
improves, the patient never regains control to the
ophthalmologist until symptoms appear in the left
eye.
Visual acuity at the time of examination was 6/6
on the right eye and 6/20 on the left eye. Anterior
segments were within normal limits. There were
minimal vitreous hemorrhages, retinal hemorrhage
in the supero-temporal quadrant accompanied by
cotton wool spots.
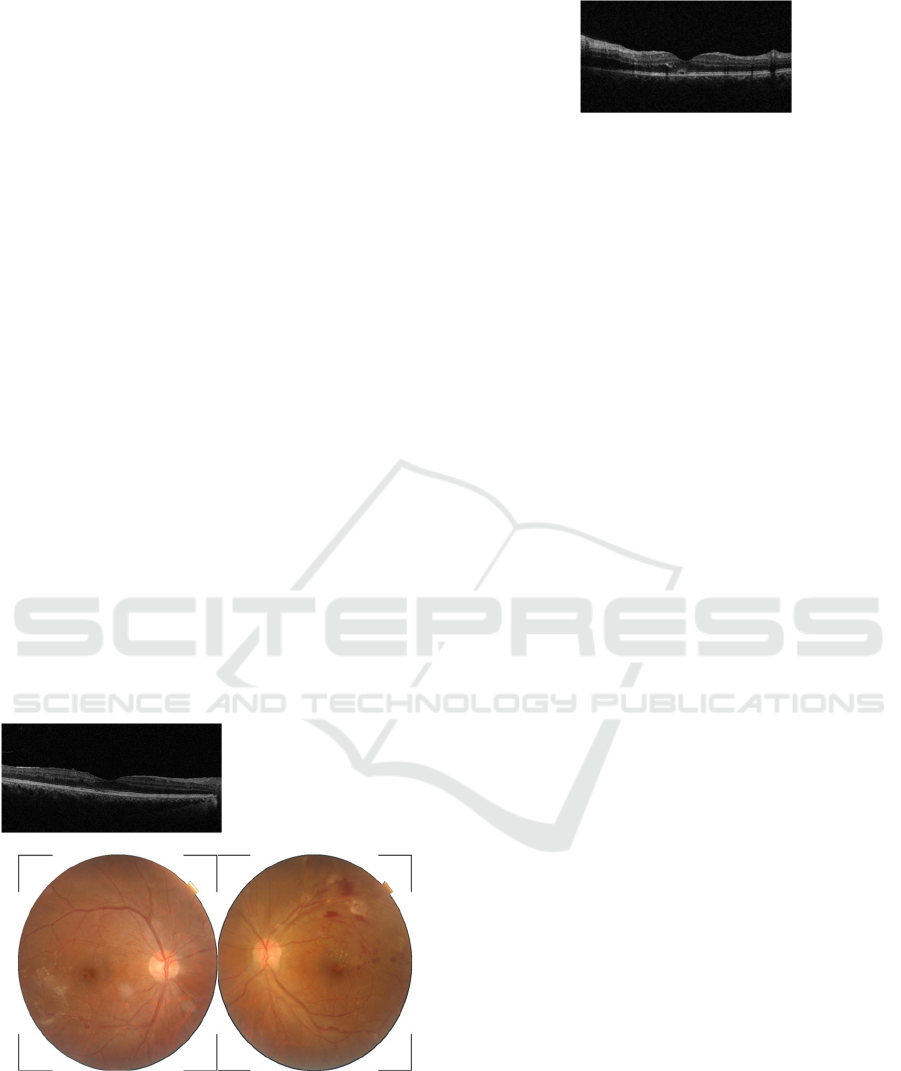
Figure 6. Retinal hemorrhage, sheating, and cotton wool
spot in the supero-temporal left eye
OCT examination showed normal foveal contour of
the right eye, and minimal sub retinal fluid and
exudate on the left eye.
Figure 7. OCT examination of the right and left eye
The patient underwent laboratory tests and chest x-
ray, and all the results were negative. Mantoux test
could not be done due to technical problems in our
Hospital. We performed sub tenon injection of
triamcinolone acetonide, systemic
metylprednisolone, and laser photocoagulation on
the left eye. The condition improved but rebleeding
occurred after 1 month, so did the complaint for
black spots. Due to the recurrence, we referred the
patient to a pulmonary specialist to determine the
possibility of latent tuberculosis infection. They
performed IFN-Gamma Release Assay (IGRA)
examination, and revealed a positive result for
tuberculosis.
5 DISCUSSION
Retinal vasculitis is a group of diseases
characterized by inflammation of the retinal blood
vessels. Consensus of the Standardization of Uveitis
Working Group in November 2004 described retinal
vasculitis as an inflammation and changes in retinal
blood vessels, including perivascular sheathing,
vascular leakage , or occlusion (Mir et al., 2017; Ku
et al., 2012).
Although many retinal vasculitis are unknown
(idiopathic), many systemic diseases are associated
with this diseases such as tuberculosis, Lyme
disease, syphilis, toxoplasmosis, or viral infection
(Ku et al., 2012; Mesquida et al., 2017; Sharief et
al., 2017). Retinal vasculitis can also be associated
with other diseases like Behcet, sarcoidosis, multiple
sclerosis, collagen-vascular disease, and sympathetic
ophthalmia. In addition, retinal vasculitis can also be
part of posterior uveitis (Pelegrin et al., 2017; Do et
al., 2016).
Retinal vasculitis associated with tuberculosis is
Eales diseases. It is a primary idiopathic occlusive
vasculopathy, characterized by venous inflammation
(vasculitis), occlusion, and retinal
neovascularization that usually involves the
peripheral retina. In the early stages, Eales disease
often has no symptoms. Some patients may
experience black spots on the eyes (floaters) 75%, or
blurred vision due to vitreous bleeding (60%). Eales
disease is very rare in developed countries and more
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
180

often found in countries with poor economic levels.
India is one of the countries that quite often reported
the case. They found that 1 of 200-250 eye diseases
patients suffering from Eales. The number is also
significant in Aceh (Indonesia), but has never been
thoroughly reported (American, 2014; Das et al.,
1994; Dalvin & Smith, 2017; Patnaik, et al., 1998).
In this paper, the first and second patients come
with the main complaints of floaters, and blurred
vision caused by vitreous hemorrhage. While the
third patient came with metamorphopsia associated
with macular edema caused by Branch Retinal Vein
Occlusion (BRVO). BRVO in this case can occur
because of the inflammation (retinal phlebitis),
which is the underlying disorder of the disease. The
inflammatory cells found in the branches of central
retinal vein cause blockage of the blood vessels,
resulting in the occurrence of BRVO. Sometimes
inflammation occurs in the central retinal vein
causing the occurrence of Central Retinal Vein
Occlusion (CRVO) (Patnaik et al., 1998).
Etiopathogenesis of Eales disease remains
controversial. Wardsworth described Eales disease
as a primary vasculitis with an unknown etiology in
young adults. Retinal vasculitis and peripheral
retinal revascularization associated with various
systemic and ocular diseases may resemble Eales
disease in the inflammatory and proliferative
phases.
12
Our three patients have no symptoms of
tuberculosis infection seen from chest x-ray
examination. However, Mantoux tests were strongly
positive (induration more than 15 mm) in the first
and second patients. This test is one of the major
tuberculin skin tests used around the world and
widely used in patients with Eales disease. Mantoux-
positive rate has been reported in 42-98% of Eales
disease. However, Mantoux examination can be
positive in 67-90% of healthy adults in India (and
possibly other developing countries including
Indonesia). Therefore, the role of this examination in
Eales disease still a questioned, in addition this
disease has also been reported in patients with
Mantoux negative (Patnaik et al., 1998; Biswas &
Verma, 2007; Biswas et al., 2002; Talat et al., 2014;
Murugeswari et al., 2014). In our first and second
cases, the Mantoux examination results were
strongly positive with induration of more than 15
mm. The third patient underwent IGRA due to
technical problem in performing Mantoux test in our
hospital and all hospitals in Aceh at the time. This
examination is considered to have better specificity
than tuberculin skin test (Banaei et al., 2016; Katyal
et al., 2018). So far, we have not found a literature
report about IGRA on Eales disease. In our case this
test helped us establish the diagnosis. Utilization of
IGRA is therefore an interesting idea.
The three major signs of Eales disease are
inflammation characterized by periphlebitis or
vasculitis in the periphery retina, ischemia caused by
blood vessel blockage, and retinal
neovascularization (in optic disc or retina) which
responsible for recurrent vitreous haemorrhage (Das
et al., 2010; Gadkari, 2007). In the first patient we
found vitreous bleeding and signs of inflammation in
the peripheral retina. Although bleeding and
inflammation are not severe, an excellent response
to corticosteroids coupled with strong positive
Mantoux results helped us to guide the diagnosis. In
the second patient, the retina couldn’t be evaluated
more detail due to dense vitreous hemorrhage. It is
unfortunate that so difficult for us to follow up the
course of the disease because the patient has
undergone vitrectomy abroad, and not so good
record system in our hospital at that time. The
diagnosis of Eales became doubtful because there
was no confirmation of the inflammatory process in
the peripheral retina, until the patient came again
about 1 year later and there was a severe vitreous
bleeding occurred in the other eye. Male with
productive age, recurrent vitreous hemorrhage, and
strong positive results of Mantoux test guide us to
make the most possible diagnosis of the patient. The
third patient presented with symptoms characteristic
with inflammation of the peripheral retina,
accompanied by complications of BRVO in both
eyes that do not occur simultaneously. Positive lab
testing is only IGRA tests and a slight increase in
total cholesterol and LDL, as well as decreased
HDL. The literature suggests that young adult males
with BRVO or CRVO who do not have hypertension
and diabetes, and who have no signs of
arteriosclerosis, and indicate the presence of
phlebitis can be diagnosed as Eales. Response to oral
corticosteroids helps us to confirm the diagnosis.
With all the limited facilities, we have, the first
and third patients can still be well managed. The
disease records describe that the retina and vision is
still stable with corticosteroid and laser therapy in
the first patient, as well as corticosteroids and
intravitreal anti-VEGF injection in the third patient.
The second patient had to undergo overseas
vitrectomy surgery due to severe vitreous
hemorrhage. The absence of vitrectomy machine in
our province at that time made it difficult for us to
manage it here. We recognize that the financial
problems facing our country, especially in the
province of Aceh, causes difficulties and sometimes
lead to a bit of frustration in terms of diagnosing and
Retinal Vasculitis in Patients with Positive TB Testing in Aceh (Indonesia): A Case Series
181

managing. So, it is our responsibility as an
ophthalmologist, and also local governments to
continuously strive to improve the facilities and
human resources in our province, in order to perform
good management for our patients later.
REFERENCES
American Academy of Ophthalmology staff., (2014-
2015). Other Retinal Vascular Diseases. In: American
Academy of Ophthalmology staff, ed. Retina and
Vitreous. Basic and Clinical Science Course. Sec 12.
Sanfransisco: American Academy of Ophthalmology.
pp. 113-55
Banaei, N., Gaur, RL., Pai, M., (2016). Interferon Gamma
Release Assays for Latent Tuberculosis: What are the
Sources of Variability? Journal of Clinical
Microbiology. 54, 845-850.
Biswas, J., Sharma, T., Gopal, L., Madhavan, HN.,
Sulochana, KN., Ramakrishnan, S., (2002). Eales
disease—an update. Survey of ophthalmology. 47(3),
197-214.
Biswas, J., Verma, A., (2007). An Update on Eales’
Disease. Kerala Journal of Ophthalmology. 19, 300-
307
Dalvin, LA., Smith, WM., (2017). Intraocular
manifestations of mycobacterium tuberculosis: A
review of the literature. Journal of Clinical
Tuberculosis and Other Mycobacterial Diseases. 7,
13-21.
Das, T., Biswas, J., Kumar, A., Nagpal, PN.,
Namperumalsamy, P., Patnaik, B., Tewari, HK.,
(1994) Eales' disease. Indian J Ophthalmol. 43, 3-18.
Das, T., Pathengay, A., Hussain, N., Biswas, J., (2010).
Eales’ disease: diagnosis and management. Eye. 24
(3), 472.
Do, BK., Giovinazzo, J., (2016). Retinal Vasculitis. Adv
Ophthalmol Optom.1(1), 69–84.
Gadkari, S., (2007) Inflamatory vascular disease. Eales’
disease. In: Joussen, AM., Gardner, TW., Kirchhof,
B., Ryan, SJ, ed. Retina Vascular Disease. Berlin:
Springer.p.613-627
Katyal, M., Leibowitz, R., Venters, H., (2018). IGRA-
Based Screening for Latent Tuberculosis Infection in
Persons Newly Incarcerated in New York City Jails.
Journal of Correctional Health Care. 24(2),156-170.
Ku, JH., Ali, A., Suhler, EB., Choi, D., Rosenbaum, JT.,
(2012). Characteristics and visual outcome of patients
with retinal vasculitis. Arch Ophthalmol.
130(10),1261–1266.
Mesquida, M., Llorens, V., Adán, A., (2017). New
imaging techniques in retinal vasculitis. Med Clin
(Barc) 149(6), 261–6.
Mir,TA., Reddy, AK., Burkholder, BM., Walsh, J.,
Shifera, AS., Khan, IR., Thorne, JE., (2017). Clinical
Features and Incidence Rates of Ocular Complications
in Patients With Retinal Vasculitis. Am J Ophthalmol
179,171–178.
Murugeswari, P., Shukla, D., Kim, R., Namperumalsamy,
P., Stitt, AW., Muthukkaruppan, V., (2014).
Angiogenis Potential of Vitreous from Proiferative
Diabetic Retinopathy and Eales’ Disease Patients.
PloS ONE. 9(10), 1-8.
Patnaik, B., Nagpal, PN., Namperumalsamy, P., Kalsi, R.,
(1998). Eales disease: clinical features,
pathophysiology, etiopathogenesis. Ophthalmology
Clinics. 11(4), 601-617.
Pelegrin, L., Hernández-Rodríguez, J., Espinosa, G.,
Llorenç, V., Sainz-de-la-Maza, M., Fontenla, JR.,
(2017). Characterization of isolated retinal vasculitis.
Analysis of a cohort from a single center and literature
review. Autoimmun Rev. 16(3), 237–243.
Sharief, L., Lightman, SUE., Blum-hareuveni, T., Bar, A.,
Tomkins-netzer, O., (2017). Clinical Outcome of
Retinal Vasculitis and Predictors for Prognosis of
Ischemic Retinal Vasculitis. Am J Ophthalmol 177,
206–212.
Talat, L., Lightman, S., Tomkins-Netzer, O., (2014).
Ischemic Retinal Vasculitis and its Management.
Journal of Ophthalmology. 7, 1-13
SKIC-MHS 2018 - The 2nd Syiah Kuala International Conference on Medicine and Health Sciences
182
