
Mental Health Literacy in South East Asia in a Cultural Context: A
Systematic Review
Fairuziana
1
, Marty Mawarpury
2
, Andriyani E. Lay
3
, Yeni Fitriani
4
, Yanti Fitria
5
,
1
Faculty of Psychology, Universitas Indonesia, Depok, Indonesia
2
Faculty of Medicine, Pyschology Department, Universitas Syiah Kuala, Banda Aceh, Indonesia
3
Faculty of Training and Education, Universitas Nusa Cendana, Kupang, Indonesia
4
Faculty of Psychology, UniversitasGadjahMada, Yogyakarta, Indonesia
5
Psychiatry Medical Unit, Ulin General Hospital, Banjarmasin, Indonesia
yeni.fitriani@mail.ugm.ac.id,yan.fitri.kj@gmail.com
Keywords: Mental Health Literacy, Cultural Context, South East Asia
Abstract: Mental health literacy and positive community attitude toward mental illness significantly
predicted the simultaneous formal help seeking to professional treatment. The diverse setting of
Southeast Asia population mental health literacy with consideration to cultural circumstances are
still understudied. This includes the population’s traditional knowledge, belief, and local
treatments of mental disorders symptoms. This study aims to systematically review available
literature to learn the variety of mental health literacy studies and analyse whether the studies
consider cultural circumstances such as local knowledge and informal help seeking. Studies that
were conducted in South East Asian countries population were systematically reviewed
according to relevant keywords in English and Bahasa Indonesia from selected major electronic
sources. The selected studies focus on the general public, health care workers, and mental health
professionals knowledge; (ii) written in English; Indonesia; (iii) study located the countries of
Southeast Asia; and (iv) focusing on mental health literacy, attitudes, and beliefs about mental
illness and mental, knowledge on mental health, and other related terms. The study result in a
systematic review of 46 articles, which were published between the past 40 years in the period of
1978- 2018. The articles are presented under the themes of 1. ) Mental health literacy among lay
people and healthcare professionals 2.) Attitudes and beliefs toward mental illness and 3.) Help-
seeking approach to mental illness. The findings discovered that while common understanding of
mental disorder is expected to identify the mental health literacy, embedding cultural context
would accommodate the understanding of lay people.
1 INTRODUCTION
The issue of mental health has become a major
concern in both the developed and developing
countries (Ganasen, et al, 2008). According to Steel
et al (2014), the global prevalence of common
mental disorders in 26 high income countries and 37
low and middle income countries indicated that on
average one in five adults experienced a common
mental disorder within the past 12 months. The term
“common” refers to the high prevalent of the
disorder in the community. WHO (2017)
categorizes common mental disorder in two main
categories: depressive disorders and anxiety
disorders.
The prevalence of mental disorder is widely
measured using CIDI (Composite International
Diagnostic Instrument). However, the global
prevalence worldwide shows a wide variety across
regions. One of the factor that affect the reports on
mental health assessment is the ability to recognize
the illness. Steel et al (2009) discovered in Vietnam
that using the international diagnostic accompanied
with a culturally derived diagnostic measure would
improve the overall prevalence compare to using the
CIDI alone.
516
Fairuziana, ., Mawarpury, M., Lay, A., Fitriani, Y. and Fitria, Y.
Mental Health Literacy in South East Asia in a Cultural Context: A Systematic Review.
DOI: 10.5220/0008591505160524
In Proceedings of the 3rd International Conference on Psychology in Health, Educational, Social, and Organizational Settings (ICP-HESOS 2018) - Improving Mental Health and Harmony in
Global Community, pages 516-524
ISBN: 978-989-758-435-0
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

The expression or idiom to indicate and report
mental disorder across countries may vary and have
influence of cultural factors (Steel, et.al, 2009). For
instance, countries in North East and South East
Asia shows a lower rate of common mental disorder
compared to other region (Steel et al 2009; Steel et
al 2015). It is argued that cultural setting might over
or underestimate the prevalence of mental disorder
(Steel et al, 2014). While symptom of mental
disorder is universal, lay people would have
different ways of expressing the understanding for
the condition. For example, in Sri Lanka, the
vocabulary of “depression” is not common in the
Sinhala ethnic group but are more being used by the
Sri Lankan who respond in English (Amarasuriya,
et.al, 2015). The ability to recognize the problem as
an illness then further relates to the help seeking
behaviour. In addition, the lack of mental health
professionals in the community would then endorse
informal help seeking such as parents and friends.
The ASEAN (Association of South East Asia
Nation) which include 10 countries in South East
Asia, apart from East Timor have generated a task
force on mental health and launched a brief report
regarding the mental health system in the region.
The background of the ASEAN establishment is
based on some similarities such as geographical
position which lies between two continents and two
oceans, shate the Melayu Austronesia culture, have
the colonialized experience in the past, and have
similar interests in economic, social culture,
security, and politic.
The ASEAN Mental Health Report in 2016
reported that mental health was a challenging issue
in the developing countries. For example there are
two countries which did not have national
information and data about prevalence and mental
illness cases. One country did not have any clinical
psychologist. In addition, limited financial has effect
on health facilities, service and human resources
such as psychiatry and nurse. There were other
similarity in the 10 countries that give effect on the
people’s help-seeking behaviour such as lack of
knowledge, misunderstanding about mental health,
and cultural factor like possession, back magic, and
religion. Emotional factors like fear, shame, and
ignorance were the major barriers to seek help.
Stigma and discrimination are big challenges for
people with mental illness.
In average, less than half of the countries in
South East Asia have a mental health law, including
new laws in many countries that requires an
implementation plan. Some countries never have a
national epidemiology survey on mental health.
These problems are apart from the challenge to
provide a well ratio of human resource and service
in the community towards the need in the
population. A policy brief reported by the ASEAN
Task Force on Mental Health (2013) proposed four
solutions to address mental health issues in 10
countries of ASEAN. One of the strategies
addressed the promotion of depression awareness
and combat stigma using public education
campaigns, which include mental health literacy.
Mental health literacy was introduced by
Anthony Jorm (1997), which is defined as
“Knowledge and beliefs about mental disorders
which aid their recognition, management or
prevention. Mental health literacy includes the
ability to recognize specific disorders; knowing how
to seek mental health information; knowledge of risk
factors and causes, of self-treatments, and of
professional help available; and attitudes that
promote recognition and appropriate help-seeking”.
Jorm’s mental health literacy studies have been
implemented in many parts of the world, in both
western and non-western countries. The knowledge
and belief regarding mental illness is positively
associated to the treatment and help seeking,
whether to professionals, semi-formal or informal
service (Novianty, 2016). The use of English as a
spoken language greatly influence mental health
literacy. Many non-western countries learn that
mental disorder is associated to black spirit and
supernatural which need the help of traditional
healers (Ganasen et al, 2008).
In addition, the lack of research in the field of
mental health is also a challenge for the government
to obtain accurate information and design programs
that fit the needs of mental health (ASEAN, 2016).
The importance of the research role for the
development of mental health programs is also put
forward by Kermode et al (2009). Furnham and
Hamid (2014) argue that the majority of mental
health research pioneered by Jorm et al, conducted
in Western countries that can be reached by
telephone survey. Meanwhile, mental health literacy
in non-western countries is less well known.
The results of research on mental health literacy
conducted in various countries such as Africa
(Aggarwal, et al, 2016 & Atilola, 2016), America
(Altweck, et al., 2016), Canada (Gagnon, Gelinas, &
Friesen, 2015) recommends the importance of
considering cultural factors in mental health literacy
and its relation to help seeking behavior (Kelly &
Wright, 2007). Even Koutoufa & Furnham (2014)
suggests further research on the motivations
underlying one's beliefs and should also examine the
Mental Health Literacy in South East Asia in a Cultural Context: A Systematic Review
517
potential cause-and-effect relationship between
social and psychological conditions and mental
health literacy.
In an ethnographic approach, culture has a role
to determine how society determine the continuum
of normal to abnormal conditions, contribute to
certain cause of mental disorders, provide perception
of health workers in assessing, diagnosing, labelling
disorders and explaining mental illness in their
patients, and influences the way people perceive the
mental illness label that has been given by society
(Burnard, Naiyapatana & Lloyd, 2006). In the
current study, we look at research findings about the
relationship between culture and mental health
literacy in South East Asian countries as well as its
relationship to the behaviour of seeking help.
The current research aims to systematically
review previous research in South East Asia
regarding mental health literacy with two objectives
1.) Learning the variety of mental health literacy
studies 2.)Analysing whether the study considers
cultural circumstances such as local knowledge and
informal help seeking as mental health literacy.
Similarities and differences across literatures will
also be compared to find a pattern in understanding
mental health literacy in the context of South East
Asia region.
2 METHOD
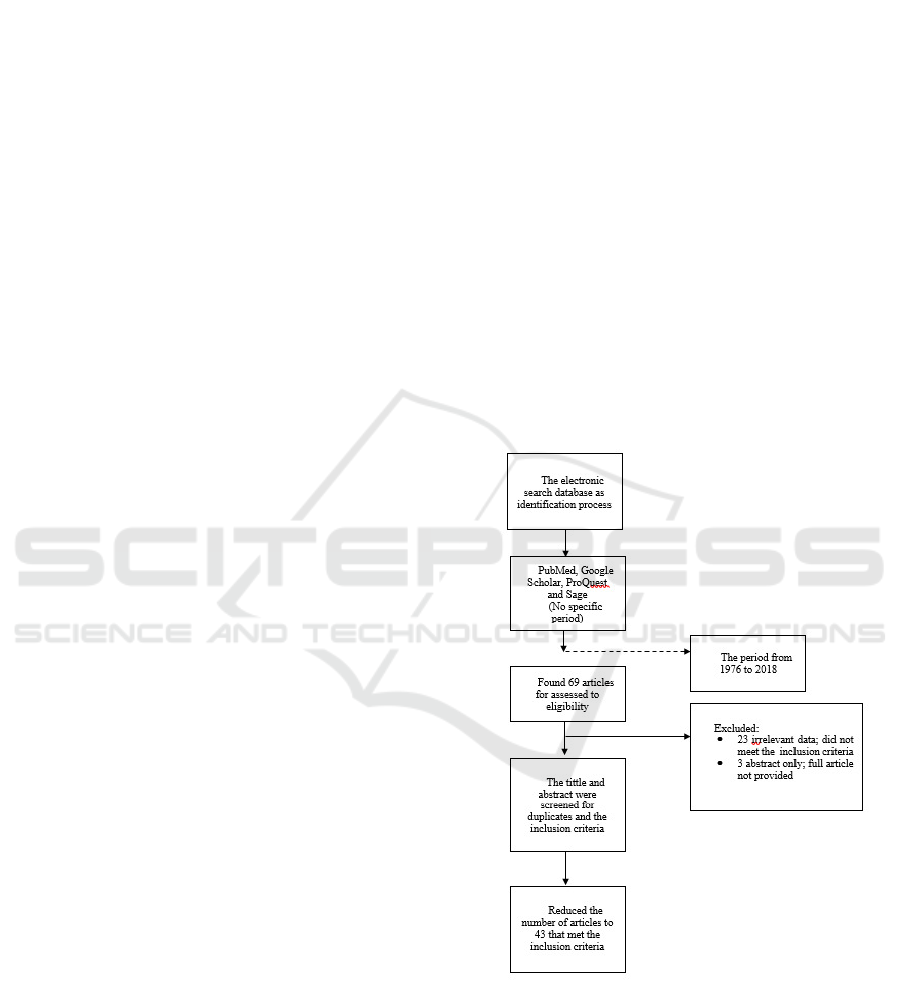
The electronic search database is performed using
PubMed, Google Scholar, ProQuest and Sage. The
literature search is not located within a certain
period to expand the possibility collecting as many
relevant articles to the key search. Articles that have
been obtained during the search process, are from
1976 to 2018. The selected terms of keyword are
used to ensure the entry of articles as much as
possible. Search is done by entering keywords
(attitude), (knowledge), (belief), (culture), (cultural
belief) AND the combination with (mental health
literacy), (mental illness), (mental disorder),
(depression), (anxiety), (schizophrenia) AND
(Southeast Asia) by title and abstract search. The
hand search of the literature was conducted as a
form of citation search study to identify relevant
studies which does not belong to a particular
database.
Based on these primary and secondary
references, the studies included in this paper meet
the following criteria: (i) studies focusing on the
general public, health care workers, and mental
health professionals; (ii) the papers are written in
English; Indonesia; (iii) the focus of this paper is the
countries of Southeast Asia; and (iv) papers focusing
on mental health literacy, attitudes, and beliefs about
mental illness or disorder, knowledge of mental
illness or disorder, relief seeking, beliefs about
seeking treatment, utilization of mental health
services, AND mental illness excluding eating
disorders, substance-related disorders, gambling-
related disorders, learning disabilities, or attention
deficit disorders.
The search criteria yielded 69 articles which
went through screening for no duplicated article by
title and abstract. In addition, article that didnot meet
the inclusion criteria were excluded. At the time of
the screening process, there are 43 articles that meet
the criteria and as many as 26 articleswere excluded,
including titles without abstract. This search method
is not precise and complete yet, as there are
possibilities of not finding articles using a different
term out of the search key both through the database
or by hand.
Figure 1. Flow diagram of systematic review procedure.
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
518

3 RESULT
This systematic review included 43 articles, which
are published between the past 40 years of 1978-
2018. The studies were conducted amonglay people
and health care professionals in South East Asia.
The present work review category is similar to
Tonsing’s (2017) study which was conducted among
Singaporean population.In that study, a narrative
review approach was conducted to asses 20 articles
under the theme of mental health literacy across the
lay people and health professional participants.
In the present work, most reviewed articles
usevignette study for the data collection and
aresummarized in Appendix B. The 43 articles are
presented under the following subheadings:
1. 23 articles under mental health literacy among
lay people and healthcare professionals
2. 25 articles under attitudes and beliefs toward
mental illness
3. 13 articles under help-seeking approach to
mental illness treatment
Each article is not exclusively under one
heading. Some articles fall under two or three
themes
3.1 Mental Health Literacy among Lay
People and Healthcare
Professionals
This topic is discussed in more than half of the
articles reviewed. The results in Southeast Asian
countries have similar results. From an ethnic point
of view, the rate of Mental Health Literacy (MHL)
differs in comparing the level of MHL in an ethnic
group. For example,the Chineseethnic in the
countryside has lower MHL than ethnic Malaysians.
While in other places mentioned ethnic China-
Singapore has a better MHL than Malaysian and
Indian ethnic.
Factors affecting the MHLto be better in the
community are based on the residential locations
where urban communities have better MHL, higher
education, income and based on religion. MHL
related knowledge is obtained formally and
informally. In terms of time, research from year to
year still shows similarities related to causes and
symptoms of mental disorders. Mental disorders are
still associated with supernatural beliefs and
traditional beliefs.
Many consider mental disorders due to external
factors such as family, occupation, unmarried or
karmic. The symptoms mentioned related to mental
disorders such as lack of hope, physical complaints,
lack of courage, poor mind, defeat, communication
difficulties and abnormal social behaviour, some are
harmful and not.
In terms of individual or groups knowledge,
psychiatrists have the ability to recognize mental
disorders better than others. Traditional healers can
help in recognizing symptoms but are not significant
in their role to reduce or heal symptoms. In terms of
diagnosis, dementia, alcohol abuse and OCD are
better recognized. Depression is better known than
schizophrenia. New schizophrenia is recognized
after years without treatment.
3.2 Attitudes and Beliefs toward
Mental Illness
Some SEA countries have different attitudes toward
mental disorders. For example, urban Chinese
society shows a higher level of knowledge for
depression than rural China. Meanwhile, the urban
and rural Indian urban have a relatively similar
attitude about depression. In another study, the
Chinese Tiansghoa community has a better level of
literacy on depression, followed by Malaysians and
Indians. This fact is associated with education and
income levels. Older age, male gender, lower
education and socioeconomic status are associated
with more negative attitudes toward people with
mental disorders.
The response rate for psychiatrists is higher than
that of the primary healthcare practitioner. The
majority of primary health practitioners and
psychiatrists consider that patients will be
discriminated against, especially schizophrenia and
mania rather than depression. For example, major
health practitioners in Singapore have more negative
views than Singapore psychiatrists about the results
of professional interventions for the three major
psychiatric disorders. These findings have
implications for education and training for primary
health practitioners as well as for the care of
psychiatric patients in primary health environments.
Mental health contributes less to the behavior of
help seeking. Community attitudes toward mental
illness contributes more significantly to the behavior
of seeking help. Compared with the general
population, mental health professionals have a more
positive attitude toward mental illness. Compared to
nurses, doctors showed a significantly more positive
attitude to 'social restrictions' and 'prejudice and
misunderstanding'. Having a close family or friend
diagnosed with a mental illness is negatively related
to 'social distance' among professionals.
Mental Health Literacy in South East Asia in a Cultural Context: A Systematic Review
519

Stigma against people with mental disorders is
higher in older individuals, men, lower education
and lower incomes. Stigma is lower in individuals
who have experience or have relatives who are
affected by mental disorders. Severe psychotic
disorders (more psychotic) have more stigma in
society.
MHL does not contribute much to the behavior
of seeking medication, while the attitude toward the
illness is the most decisive attempt to seek treatment.
However, the higher the MHL increases the effort to
seek professional treatment.
3.3. Help-seeking Approach to Mental
Illness Treatment
The same problem in almost all countries in SEA,
the number of mental health professionals is still
lacking. Factors that influence the search for
professional treatment are age, gender, ethnicity,
income, personal experience or the nearest person,
and stigma. Among the 13 articles discussing the
approach / behavior of help seeking on the treatment
of illness / mental disorders discovered:
a. Recognize mental disorders and labeling issues
and naming mental disorders. There are still many
lay people unable to recognize the different types of
mental disorders. A negative attitude toward mental
illness that prevents individuals from seeking
professional care, and seeking help, is a common
theme that emerges. Health professionals have
different views on the causes and treatment of
mental disorders. The findings also reveal that
seeking treatment, attitudes and beliefs about mental
illness are associated with mental health literacy. In
ordering, here are some categories of criteria used to
label baa / mental disorder / insane in an individual:
b. Seeking help: traditional healer, simultaneously or
before seeking professional help, The most common
undertaking in dealing with mental disorders is
talking to family. In terms of treatment, there are
some tendencies to believe that mental health
services are only intended for severe psychiatric
disorders such as schizophrenia. The reluctance to
seek professional help is also related to the
perception that the disturbance is not severe enough
to receive assistance. Traditional explanatory models
can provide understanding and integration of the
meaning system of interruptions but are
unsuccessful in alleviating symptoms. The strength
of social support and the trust of patients, friends,
and / or relatives in the treatment of mental illness is
strongly associated with traditional medicine.
Culture is believed to be a major deterrent to
psychiatric care in some countries.
c. Not looking for help. The reason for not seeking
professional treatment is because they do not know
of any health facilities for treatment of mental
disorders, distance to health facilities, beliefs about
other causes that can be treated in other ways, and
financial problems.
4 DISCUSSION
Numerous study of mental health suggested that
characteristic of demographic has affected on
knowledge and mental health literacy. Novianty &
Hadjam, (2017) suggest that there is a direct and
indirect connection between characteristic of
demography and community’s attitude toward
mental health problem and seeking formal help,
potential gender differences in MHL could inform
future intervention (Coles, etc., 2015). Age group
(Marcus &Westra, 2012) and group of racism
(Ypinazar, Margolis, Haswell-Elkins, & Tsey, 2007)
have unique views and needs respect to the
management of mental health problems. Regarding
to socio-economic status, SES is a factor to
recognize psychiatric disorders and treatment
options (Furnham, & Hamid, 2014). SES also has a
consistent relationship with the MHL and has an
inconsistent relationship with help seeking behavior
(Holman, 2015).In this study we also find that most
of research reported demographics factor had affect
toward mental health literacy and level of formal
help-seeking (Yeap& Low, 2009). However, these
factors play different roles on individual and
community group of mental health literacy, hence
influence formal help-seeking. Demographic
characteristic of sample in the studies were
conducted in Indonesia, Malaysia, Singapore, Laos,
Vietnam, Thailand, and Brunei Darussalam covered
various social demographic backgrounds such as
age, gender, education, religion, language, ethnicity,
socioeconomic status, mental disorder patients,
residential location, community, families, students,
religious practitioner and professionals in different
research context.
The range of age sample is the lowest 15 years
and highest 65 years old. Tze-Ping et al (2008)
indicated that a large proportion of adults with
mental disorders do not seek help. While the
younger sample which have good knowledge of
mental health were more willing to seek help (Yeap
& Low, 2009). Gender factors influence perception
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
520

and awareness of pain. In general, women tend to be
more aware of symptoms than men who tend to be
unaware of health problems and are more likely to
delay seeking help. Education level is related to
good MHL in some mental disorder. The level of
education affects access to good mental health
information and can receive relevant information
from good education.
Ethnic differences is significantly a factor
associated with MHL against some disorders such as
how mental health is described and labelled, for
example Indians can identify depression and
dementia and more Malays can recognize dementia.
Ethnicity also affects one's belief in the cause of
mental illness. Hong Kong ethnic Chinese are more
likely to believe that social factors cause mental
illness than genetic factors. The Japanese use fewer
psychiatric labels when compared to Australians
(Chong SA, et al, 2016).
According to the socioeconomic status, there are
differences in helps seeking behaviour to
professionals. The low-SES families seeks more
formal help than high-SES families. Families with
lower middle-class socioeconomic status that have
family members with mental disorders tend to refer
to professional help seekers than families with
above-average incomes that tend to cover up in
shame (Novianty & Hadjam, 2017).
Language and religion play a major role
especially in the therapeutic process. The language
differences of the therapist and the patient affect the
expression, idiom, and meaning. Religious
differences will affect the perspective and beliefs of
individuals about mental disorders. Religion is the
lifeline of the individual, which is then adopted as
the ideology and philosophy of the state
(Kumaraswamy, 2007).
According to the findings, most countries in
South East Asia were find available to provide
studies about mental health literacy, except the
Philippines and East Timor. Most studies elaborated
the mental health literacy and attitude. While fewer
studies emphasized in the help seeking behaviour, it
has been covered in the first two categories. The
categories are somewhat overlapped because each
article would usually explain two categories in one
article, for instance, mental health literacy and help
seeking or attitude and help seeking. Thus, the
category does not exclusively determine the
differences of one article to another.
Given the respondent’s participation, most of the
participants are distinctly grouped according to their
living place such as urban and rural, or education
major such as medical and non-medical, and age
group. Students’ literacy are moderate.
The studies show that the understanding of
mental illness are associated with the level of
income. Rural participants tend to have less income
and lower education attainment which consequently
gives less information about mental health. Thus,
people living in rural area associate the causation of
mental health problems to God’s destiny and
supernatural causation. However, none of the urban
or rural citizen use supernatural labels to identity the
problem.Ethnicity are related to the understanding of
mental health cases, but the predictors are still
associated to income levels and education
attainment.
Most mental health literacy vignettes requires the
participants to correctly answer the case with a
psychotic label instead of lay people’s label such as
emotional distress. On the other hand, the use of
English as the main spoken language does affect the
participant’s knowledge to recognize the mental
health cases in a medical term.
Rural participants would endorse for religious
treatment compare to the urban’s who prefer to
modify their lifestyle, visiting a psychologist, or
psychiatrist. Recognizing culture as part of the
understanding of mental health was discovered in
several studies. In Thailand, there is a mixture of
modern and traditional treatment for mental illness
which appear to be available in rural areas compare
to the capital in Bangkok. In Javanese culture, the
spiritual connection become a coping mechanism
and screening tool to identify depression disorder.
The idiom of “discouragement” is expressed a
demotivated feeling. In the Laotian society, folk
diagnosis are categorized with some social label
called “baa label”. Social explanation were also
found in Indonesia and Malaysia. It is argued that
mental health problems have similar symptoms
around the world, however the expression are
different according to the value and belief system in
the society.
Religion also holds an important role to define
mental health literacy. Lay people in countries such
as Brunei Darussalam and Malaysia believe that
mental disorder is a consequence for not obeying the
Islamic commands. Buddhist is also one of the
religion in many parts of South East Asia, which
holds value to recognize the mental health state of a
person.
Mental Health Literacy in South East Asia in a Cultural Context: A Systematic Review
521

5 CONCLUSION
The present study in South East Asia Region have
covered most of the studies available related to
mental health literacy. Lay beliefs about
schizophrenia may serve different functions for
different ethno-cultural groups, which has an
influence on help-seeking behaviour. The folk
diagnosis of mental disorders is made not based on
the strength of one criterion, but several. While a
common understanding of mental disorder is
expected to identify the mental health literacy,
adding cultural context would accommodate the
understanding of lay people. Studies in mental
health literacy should integrate anthropology and
sociology as valuable perspective to a better
understanding of the community’s literacy on mental
health.
REFERENCES
*Afifah, K.A., Asyanti, S. and Psi, S.,
2016. LiterasiKesehatan Mental pada Tenaga
Kesehatan (Doctoral dissertation, Universitas
Muhammadiyah Surakarta).
Aggarwal, S., Berk, M., Taljard, L., & Wilson, Z.
(2016).South African adolescents’ beliefs about
depression. International Journal of Social
Psychiatry, 62(2), 198-200.
Atilola, O. (2016). Mental health service utilization
in sub-Saharan Africa: is public mental health
literacy the problem? Setting the perspectives
right. Global health promotion, 23(2), 30-37.
Altweck, L., Marshall, T. C., Ferenczi, N.,
&Lefringhausen, K. (2015). Mental health
literacy: a cross-cultural approach to knowledge
and beliefs about depression, schizophrenia and
generalized anxiety disorder. Frontiers in
psychology, 6.
Amarasuriya, S.D., Jorm, A.F. and Reavley, N.J.,
2015. Depression literacy of undergraduates in a
non-western developing context: the case of Sri
Lanka. BMC research notes, 8(1), p.593.
ASEAN. (2016). ASEAN mental health system for
ASEAN Mental Health. Jakarta: The
ASEANSecretariat.http://asean.org/storage/2017/
02/55.-December-2016-ASEAN-Mental-Health-
System.pdf. Accessed by July 11, 2018. 22:46
pm
ASEAN. (2013). ASEAN Mental Health Task
Force. Jakarta: The ASEAN Secretariat.
*Brintnell, E, S, Sommer, R, W, Kuncoro, B,
Setiawan, G, Pandu & Bailey, P 2013. ‘The
expression of depression among Javanese
patients with major depressive disorder: A
concept mapping study’, Transcultural
Psychiatry, pp. 1-20.
*Burnard, P, Naiyapatana, W & Lloyd, G 2006.
‘Views of mental illness and mental health care
in Thailand: a report of an ethnographic study’.
Journal of psychiatric and Mental Health
Nursing, vol. 13, pp. 742-749
Gagnon, M. M., Gelinas, B. L., & Friesen, L. N.
(2015). Mental Health Literacy in Emerging
Adults in a University Setting: Distinctions
Between Symptom Awareness and
Appraisal. Journal of Adolescent Research,
DOI.0743558415605383.
Ganasen, K.A., Parker, S., Hugo, C.J., Stein, D.J.,
Emsley, R.A. and Seedat, S., 2008. Mental health
literacy: focus on developing countries. African
Journal of Psychiatry, 11(1), pp.23-28.
*Chong, S, A, Verma, S, Vaingankar, J, A, Chan, Y,
H & Wong, L, Y 2007. ‘Perception of the public
towards the mentally ill in a developed Asian
country’. Social Psychiatry and Psychiatry
Epidemiology, vol. 42, pp. 734-739
*Chong, S, A, Abdin, E, Picco, L, Pang, S,
Jeyagurunathan, A, Vaingankar, J, A, Kwok, K,
W &Subramaniam, M. 2016. ‘Recognition of
mental disorders among a multiracial population
in Southeast Asia’. BMC Psychiatry, pp. 1-10.
Coles, M.E., Ravid, A., Gibb, B., George-Denn, D.,
Bronstein, L.R. and McLeod, S., 2016.
Adolescent mental health literacy: Young
people's knowledge of depression and social
anxiety disorder. Journal of Adolescent
Health, 58(1), pp.57-62.
*Coton, X, poly, S, Hoyois, P, Sophal, C & Dubois,
V 2008. ‘The healthcare-seeking behavior of
schizophrenic patients in Cambodia’.
International Journal of Social Psychiatry, vol.
54, no. 4, pp. 328-337.
*Edman, J, L & Koon, T, Y 2000. ‘Mental illness
beliefs in Malaysia: Ethnic and Intergenerational
comparisons’. International Journal of Social
Psychiatry, vol. 46, no. 2, pp. 101-109.
*Furnham, A. & Hamid, A. (2014). Mental health
literacy in non-western countries: a review of the
recent literature. Mental Health Review Journal.
Vol. 19 No. 2 2014, pp.84-98. DOI
10.1108/MHRJ-01-2013-0004
Holman, D., 2015. Exploring the relationship
between social class, mental illness stigma and
mental health literacy using British national
survey data. Health:, 19(4), pp.413-429.
Jorm, A.F., Korten, A.E., Jacomb, P.A., Christensen,
H., Rodgers, B. and Pollitt, P., 1997. "Mental
health literacy": a survey of the public's ability to
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
522

recognise mental disorders and their beliefs
about the effectiveness of treatment. Medical
Journal of Australia, 177(5), pp.182-186.
*Kadir, N, B, A &Bifulco, A 2010. ‘Malaysian
moslem mothers’ experience of depression and
service use’, Cultural Medical psychiatry, vol.
34, pp. 443-467.
Kelly, C. M., Jorm, A. F., & Wright, A. (2007).
Improving mental health literacy as a strategy to
facilitate early intervention for mental
disorders. Medical Journal of Australia, 187(7),
S26.
*Khan, T, M, Sulaiman, S, A &Hassali, M, A 2010.
‘Mental health literacy towards depression
among non-medical students at a Malaysian
university’. Mental Health in Family Medicine,
pp. 27-35.
*Khan, T, M, Sulaiman, S, A, S, Hassali, M, A,
Anwar, M, Wasif, G & Khan, A. H 2010.
‘Community knowledge, attitutes, and beliefs
towards depression in the state of Penang,
Malaysia. Community Mental Health Journal,
vol. 46, pp. 87-92.
Koutoufa, I., &Furnham, A. (2014). Mental health
literacy and obsessive–compulsive personality
disorder. Psychiatry Research, 215(1), 223-228.
*Kua, J, H, K, Parker, G &Jorm, A, F 2000. ‘Beliefs
about outcomes for mental disorders: A
comparative study of primary health practitioners
and psychiatrists in Singapore’. Singapore
Medical Journal, vol. 41, no. 11, pp. 542-547.
*Kumaraswamy, N 2007. ‘Psychotherapy in Brunei
Darussalam’. Journal of Clinical Psychology: In
Session, vol. 63, no. 8, pp. 735-745.
*Kurihara, t, Kato, M, Reverger, R &Tirta, I, G, R,
T 2006. ‘Beliefs about causes of schizophrenia
among family members: A community-based
survey in Bali’. Psychiatric Services, vol. 57, no.
12, pp. 1795-1799.
*Lemelson, R.B., 2004. Traditional healing and its
discontents: efficacy and traditional therapies of
neuropsychiatric disorders in Bali. Medical
anthropology quarterly, 18(1), pp.48-76.
*Loo, P, W &Furnham, A 2012. ‘Public knowledge
and beliefs about depression among urban and
rural Chinese in Malaysia’. Asian Journal of
Psychiatry, vol. 5, pp. 236-245.
*Loo, P, W &Furnham, A 2013. ‘Knowledge and
beliefs about depression among urban and rural
Indian Malaysians’, Mental Health, Religion &
Culture, vol. 16, no. 10, pp. 1009-1029.
Marcus, M., Westra, H. and Mobilizing Minds
Research Group, 2012. Mental health literacy in
Canadian young adults: results of a national
survey. Canadian Journal of Community Mental
Health, 31(1), pp.1-15.
*Matthews, M 2011. ‘Assessment and comparison
of culturally based explanations for mental
disorder among Singaporean Chinese youth’.
International Journal of Social Psychiatry, vol
57, no. 1, pp. 3-17.
*Ng, T,Z, Jin, A, Z, Chua, H, C, Fones, C, S, L &
Lim, L, L 2008. ‘Health beliefs and help seeking
for depressive and anxiety disorders among
urban Singaporean Adults’. Psychiatric Services,
vol. 59, no. 12, pp. 105-108.
*Ng, T, P, Nyunt, M, S, Z, Chiam, P, C &Kua, E, H
2011. ‘Religion, health beliefs and the use of
mental health services by the elderly’. Aging &
mental Health, vol. 15, no. 2, pp. 143-149.
*Novianty, A &Hadjam, M, N, R 2016.
‘Literasikesehatan mental
dansikapkomunitassebagaiprediktorpencarianpert
olongan formal’. JurnalPsikologi, vol. 44, no. 1,
pp. 50-65.
*Novianty, A 2017. ‘Literasikesehatan mental:
pengetahuandanpersepsipublikmengenaiganggua
n mental’. Analitika, vol. 9, no. 2, pp. 68-75.
*Pang, S, Liu, J, Mahesh, M, Chua, B, Y, Shahwan,
S, Lee, S, P, Vaingankar, J, A, Abdin, E, Fung,
D, S,S, F, Chong, S, A &Subramaniam 2017.
‘Stigma among Singaporean youth: A cross-
sectional study on adolescent attitudes towards
serious mental illness and social tolerance in a
multi ethnic populatioan’. BMJ Open, pp. 1-11.
*Parker, G, Mahendran, R, Yeo, S, G, Loh, M, I
&Jorm, A, F 1999. ‘Diagnosis and treatment of
mental disorders: a survey of Singapore mental
health professionals. Social psychiatry and
Psychiatry Epidemiologi, vol. 34, pp. 555-563.
*Rachmayani, D & Kurniawati, Y., 2017.
StudiAwal: Gambaran Literasi Kesehatan Mental
Pada Remaja PenggunaTeknologi.Prosiding
Seminar Nasional Penguatan Individu di Era
Revolusi Informasi
*Razali, S, M &Najib, M, A, M 2000. ‘Help-seeking
pathways among Malay Psychiatric Patients’.
International Journal of Social Psychiatry, vol.
46, no. 4, pp, 281-289.
*Razali, S, M & Ismail, Z 2014. ‘Public stigma
towards patients with schizophrenia of ethnic
Malay: a comparison between the general public
and patients’ relatives’. Journal of Mental
Health, vol. 23, no. 4, pp. 176-180.
*Sanseeha, L, Chontawan, R, Sethabouppa, H,
Disayavanish, C &Turale, S 2009. ‘Illness
perspectives of Thais diagnosed with
schizophrenia’. Nursing and health Sciences, vol.
11, pp. 306-311.
*Seow, L, S, E, Chua, B, Y, Xie, H, Wang, J, Ong,
H, L, Abdin, E, Chong, S, A &Subramaniam, M
2017. ‘Corrct recognition and continuum belief
Mental Health Literacy in South East Asia in a Cultural Context: A Systematic Review
523

of mental disorders in a nursing student
population’. BMC Psychiatry, pp. 1-8
Steel, Z., Silove, D., Giao, N.M., Phan, T.T.B.,
Chey, T., Whelan, A., Bauman, A. and Bryant,
R.A., 2009. International and indigenous
diagnoses of mental disorder among Vietnamese
living in Vietnam and Australia. The British
Journal of Psychiatry, 194(4), pp.326-333.
Steel, Z., Marnane, C., Iranpour, C., Chey, T.,
Jackson, J.W., Patel, V. and Silove, D., 2014.
The global prevalence of common mental
disorders: a systematic review and meta-analysis
1980–2013. International journal of
epidemiology, 43(2), pp.476-493.
*Subramaniam, M, Abdin, E, Picco, L, Shahwan, S,
Jayegurunathan, A, Vaingankar, J,A& Chong, S,
A 2017. ‘Continuum belief and stigmatising
beliefs about mental illness: results from an
Asian community survey’, BJM Open, pp. 1-10
*Surjaningrum, E, R 2012. ‘Gambaran mental health
literacy kaderkesehatan’. Insan, vol. 14, no. 3,
pp. 194-202.
*Swami, V, Furnham, A, Kannan, K &Sinniah, D
2008. ‘Beliefs about schizophrenia and its
treatment in kotaKinabalu, Malaysia’.
International Journal of Social Psychiatry, vol.
54, no. 2, pp. 164-179.
*Swami, V, Loo, P, W &Furnham, A 2010. ‘Public
knowledge and beliefs about depression among
urban and rural Malays in Malaysia’.
International Journal of Social Psychiatry, vol.
56, no. 5, pp. 480-496.
*Ta, T, M, T, Zieger, A, Schomerus, G, Cao, T, D,
Dettling, M, Do, X, T, Mungee, A,
Diefenbacher, A, Angermeyer, M, C & Hahn, E
2016. ‘Influence of urbanity on perception of
mental illness stigma: a population based study
in urban and rural Hanoi, Vietnam’.
International Journal of Social Psychiatry, pp. 1-
11
*Tay, J, L, Chan, C, Y, W, Ho, Z, C & Lal, M 2017.
‘The ties that bind – A case report about
restraining a mentally unwell family member at
home for over a decade. Asian Journal of
Psychiatry, Vol. 26, pp. 146-148.
*Thai, Q, C, N & Nguyen, T, H 2018. ‘Mental
health literacy: Knowledge of depression among
undergraduate students in Hanoi,
Vietnam’,International Journal of Mental Health
System, pp. 1-8
*Tonsing, K.N 2017.’A review of mental health
literacy in Singapore’, Social Work in Health
Care, pp. 1-21.
*Westermeyer, J &Wintrob, R 1979. “Folk”
explanations of mental illness in Rural Laos.
American Journal Psychiatry, vol 136, no. 7, pp.
901-905
*Westermeyer, J. and Wintrob, R., 1979. " Folk"
criteria for the diagnosis of mental illness in rural
Laos: On being insane in sane places. The
American journal of psychiatry.
*Yeap, R & Low, W, Y 2009. ‘Mental health
knowledge, attitude and help-seeking tendency:
Malaysian context’, Singapore Medical Journal,
vol. 50, no. 12, pp. 1169 – 1176.
*Yeo, S, G, Parker, G, Mahendran, R, Jorm, A,F,
Yap, H, L, Lee, C &Loh, M, I 2001. ‘Mental
health literacy survey of psychiatrically and
generally trained nurses employed in a Singapore
psychiatric hospital’. International Journal of
Nursing Practise, vol. 7, pp. 414-421.
Ypinazar, V.A., Margolis, S.A., Haswell-
Elkins, M. and Tsey, K., 2007. Indigenous
Australians’ understandings regarding
mental health and disorders. Australian and
New Zealand Journal of Psychiatry, 41(6),
pp.467-478.
*Yuan, Q, Abdin, E, Picco, L, Vaingankar, J, A,
Shahwan, S, Jeyagurunathan, A, Sagayadevan,
V, Shafie, S, Tay, J, Chong, S, A &Subramaniam
2016. ‘Attitudes to mental illness and its
demographic correlates among general
population in Singapore’. Plos One, pp. 1-13
*Yuan, Q, Picco, L, Chang, S, Abdin, E, Chua, B, Y,
Ong, S, Yow, K, L, Chong, S, A &Subramaniam,
M 2017. ‘Attitudes to mental illness among
mental health professionals in Singapore and
comparisons with the general population’. Plos
One, pp. 1-14.
World Health Organization, 2017. Depression and
other common mental disorders: global health
estimates.
*List of works used for synthesis
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
524
