
Edinburgh Postpartum Depression Scale:
Ps
y
chometric Evaluation of the Indonesian Version
Anindya Dewi Paramita
1
, Andi Tenri Faradiba
2
and Puti Febrayosi
2
1
Faculty of Psychology, University of Pancasila, Srengseng Sawah, Jakarta, Indonesia
2
Faculty of Psychology, Center of Psychological Measurement, University of Pancasila, Srengseng Sawah, Jakarta,
Indonesia
Keywords: Postpartum depression, Edinburgh Postpartum Depression Scale (EPDS), psychometric evaluation
Abstract: Childbirth is a life-changing event. If the mothers are not able to adapt, major problems will arise and can
lead to depression. The Edinburgh Postpartum Depression Scale (EPDS) was the most popular screening
tools for detect the main symptom of depression in postpartum period. Developed by Cox, Holden &
Sagovsky (1987), now the EPDS has been translated into several languages such as France, Hebrew,
Swedish, Bangla, Chinese, including Indonesian. However, no one has published a comprehensive
psychometric evaluation of the Indonesian version of EPDS. The aim of this study was to investigate the
validity and reliability of the Indonesian version of the EPDS. A two-stage design was used in this study.
Stage I consisted of a process of translation and back-translation by language experts and compare it with
the original version. Stage II established the psychometric properties of the EPDS by examining the validity
and reliability of the scale using content validity index suggested by Lynn (1986) and internal consistency
using Cronbach’s alpha coefficient. Stage III examine the confirmatory factor analysis (CFA) to explore the
best model of postpartum depression measurement. The result shows that EPDS is a good tool to measure
postpartum depression in Indonesia.
1 INTRODUCTION
Childbirth is a huge milestone for every mother and
changes almost every aspect of their lives. Those
processes, starting from pregnancy, childbirth until
postpartum period cause physical, psychological and
social changes that may lead to stress (O’Hara,
1995). During postpartum period, the reproductive
organs was trying to return to their non-pregnant
state, which takes time about six weeks (Gjerdigen,
Froberg, Chaloner, & McGovern, 1993). For many
women, recovery from childbirth may experienced
discomfort for weeks, some face more serious
problem that may limit their daily function for some
time. They also need to adjust their way of life,
including disrupted sleep and daily routines which
can be challenging for mothers especially first timer
(Choudhury, Counts & Horvitz, 2013). When they
fail to manage those changes, new problem will arise
and they may end up depressed. According to Venis
& McCloskey (2008), some symptoms that
depressed mothers experience after childbirth are
mood swings, easily gets angry, fatigue, lost interest
to do daily and even sexual activities, trouble
sleeping and eating, and sometimes having thoughts
of harming themselves or their baby, that can occur
during the first two weeks after birth. This disorder
is called Post Partum Depression (PPD). In some
cases, mothers who had PPD had suicidal thoughts
or tendencies (O’Hara, 1995). This symptoms can
occurred since pregnancy until more than one year
after childbirth (Clark, Tluczek, & Wenzel, 2003;
Blum, 2007).
To prevent those mothers suffering from
postpartum depression, some professionals develop
a tool to detect depressive symptoms from mothers
after birth. One of most popular and widely used
tools to screen PPD is the Edinburgh Postpartum
Depression Scale (EPDS). The EPDS is a 10-item
self-rating scale designed to identify postpartum
depression (Cox, Holden, & Sagovsky, 1987). Since
then, several studies was conducted to validate and
translate this tool into several languages, such as
Frenchs, Hebrew, Bangla, Chinese, including
Indonesian (O’Hara, 1995). Eventhough the EPDS is
still commonly used as a research tool or for
professional purposes, its validity and reliability
410
Paramita, A., Faradiba, A. and Febrayosi, P.
Edinburgh Postpartum Depression Scale: Psychometric Evaluation of the Indonesian Version.
DOI: 10.5220/0008590204100414
In Proceedings of the 3rd Inter national Conference on Psychology in Health, Educational, Social, and Organizational Settings (ICP-HESOS 2018) - Improving Mental Health and Harmony in
Global Community, pages 410-414
ISBN: 978-989-758-435-0
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

have been poorly studied until now. The aims of the
present study are to assess the validity and reliability
of the Indonesian version of EPDS and to find
practical recommendations of the EPDS tool
development.
2 MATERIALS AND METHODS
In this section we will explain the process, materials,
and plans of our research from the very beginning
until we examine the data.
2.1 Translation
A translation of the original EPDS into Indonesian
was followed by back-translation into English. Two
psychologists translated the questionnaire into
Indonesian and two professional translators
backward translated these into English. Then the
provisional version of the Indonesian questionnaire
was developed and pilot tested. The final version of
the questionnaire was developed after considering
few suggestions from pilot data.
2.2 Sample and Data Collection
The Indonesian version of the EPDS was
administered to mothers who had a baby under age
12 months. The samples were recruited from several
health care centres in Jakarta, Bogor and Depok
during they postnatal routine check-up or their
babies’ monthly visit to the health care. 252
mothers were included in this study. The entire
participant in this study agreed to participate with
signing the informed consent and brief explanation
of the study given to them before we delivered the
questionnaire.
2.3 Measure
The EPDS consists of 10 items and each item is
rated on a four-point scale (0 to 3), giving maximum
scores of 30. This scale covers common symptoms
of depression. It excludes somatic dimensions such
as fatigue and appetite variations which are normal
during the ante- and postnatal periods (Adouard,
Glangeaud-Freudenthal, & Golse, 2005). In short,
the 10 items measured depressive symptoms (“I
have been so unhappy that I have been crying”),
anxiety (“I have been anxious or worried for no
good reason”), and anhedonia (“I have looked
forward with enjoyment to things”). The original
EPDS has a 12.5 cut-off point that showed that score
13 and up indicates major postpartum depression,
but along the way research showed that the cut-off
point varies from one research to another, range
from 9 to 12.5. According to Cox, Holden &
Sagovsky (1987), a score from 0 to 9 indicated ‘not
depressed’, while scores of 10 to 12 represent
‘borderline’ and a score 13 or more is considered
postnatal depression.
2.4 Procedure
All subjects were recruited when coming for a
postnatal check-up or monthly visit for their baby’s
vaccination at the health care services. Each woman
was then asked by researcher to participate in this
study. After hearing the explanation about the
purpose of this study, reading the agreement and
signing a written informed consent, women who
agree to participate were asked to complete the
demographic data questionnaire and the EPDS.
2.5 Psychometric Properties
We examined content validity of the EPDS’s items
with Content Validity Index (CVI). According to
Lynn (1986), there are two types of CVIs. The first
type is content validity of individual items (I-CVI)
and the second is content validity of overall scale (S-
CVI). In order to examine CVI, three experts were
recruited to evaluate the relevance of the items and
the overall scale of Indonesian EPDS. We asked all
of the experts to rate each item’s relevance to
postpartum depression in a 4-point scale
questionnaire. Then, for each item, the I-CVI is
computed as the number of experts giving a rating of
either 3 or 4, divided by the total number of experts.
To examine the S-CVI, we are looking for the
proportion of items given a rating of quite/very
relevant by raters involved. We also measure item
validity using inter-item correlation. Reliability was
estimated by measuring internal consistency with
Cronbach’s alpha coefficient from the EPDS score.
We also performed a factor analysis of the EPDS to
investigate its internal structure.
2.6 Statistical Methods
Item validity was computed using Pearson
correlation. Internal consistency was performed
using Cronbach’s α with Statistical Package for
Social Sciences (SPSS) version 25.0 for Windows.
Confirmatory factor analysis (CFA) was conducted
using Lisrel 8.7.
Edinburgh Postpartum Depression Scale: Psychometric Evaluation of the Indonesian Version
411
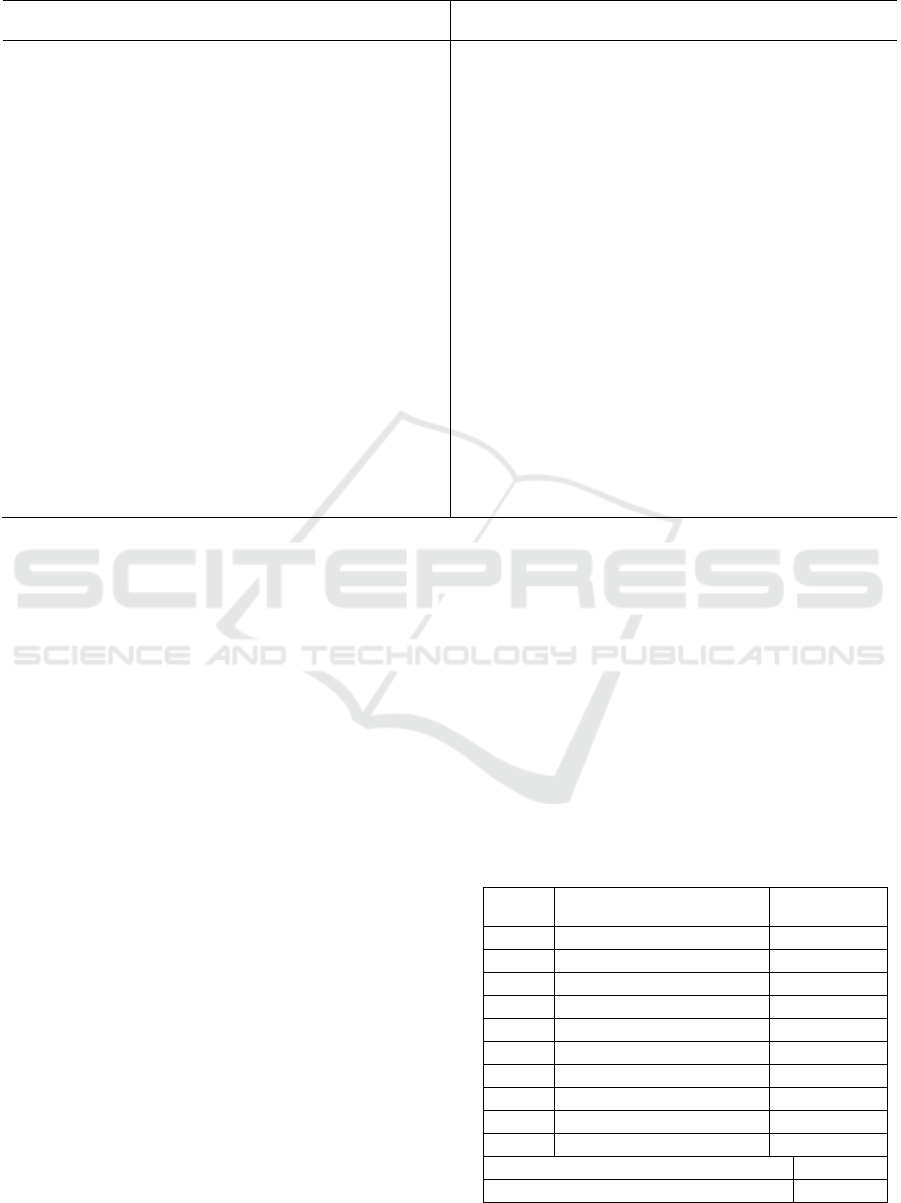
Table 1: The Edinburgh Postpartum Depression Scale
Original Version Translated Version
1. I have been able to laugh and see the funny side
of things.
2. I have blamed myself unnecessarily when things
went wrong
3. I have felt scared or panicky for not very good
reason
4. I have been so unhappy that I have had difficulty
sleeping
5. I have been so unhappy that I have been crying
6. I have looked forward with enjoyment to things
7. I have been anxious or worried for no good
reason
8. Things have been getting on top of me
9. I have felt sad or miserable
10. The thought of harming myself has occurred to
me
1. Saya bisa tertawa dan melihat sisi lucu dari
segala sesuatu
2.
Saya bisa tertawa dan melihat sisi lucu dari
segala sesuatu
3.
Saya menjadi lebih mudah panik atau merasa
takut tanpa alasan yang jelas
4.
Saya merasa tidak bahagia sehingga kesulitan
tidur
5.
Saya merasa tidak bahagia sehingga seringkali
menangis
6.
Saya lebih optimis dan gembira dalam melihat
hal-hal yang saya alami
7.
Saya merasa cemas dan khawatir tanpa ada
alasan yang jelas
8.
Segala sesuatu terasa sulit untuk saya kerjakan
9.
Saya merasa sedih atau sengsara
10. Pikiran untuk menyakiti diri saya atau bunuh diri
pernah terlintas dalam benak saya
3 RESULTS
Content Validity Study
Before finalizing the questionnaire, we pilot tested it
to some mothers who had experienced childbirth in
order to find out the readability of the items for
them. For face validity, the mothers found that the
EPDS is acceptable and easy to complete. They also
said that they able to understand what were the
meaning of each items. Then we asked three experts
to rate our item and overall scale’s relevance to
postpartum depression to examine the Content
Validity Index (CVI). There is a clinical
psychologist who had experienced at handling
depressed mothers, an obstetrician/gynaecologist,
and a nurse. According to Lynn (1986), each expert
is asked to rate the items on a 4-point ordinal scale
(1= not relevant, 2 =quite relevant, 3 =relevant, 4
=highly relevant). Then, for each item, the I-CVI is
computed as the number of experts giving a rating of
either 3 or 4. An item is categorized as relevant if all
of the experts are agree to rate the item 3 or 4. To
know the S-CVI, we computed the proportion of
items that rated 3 or 4 by the experts.
From the experts’ rating, we found out that all of
the items get the agreement from all the raters. The
S-CVI was 1.00, meaning that 100% of the total
items were judged content valid. Qualitatively, all
three experts gave suggestions related to the item’s
wording to item number six (“I have looked forward
with enjoyment to things”) and number eight
(“Things have been getting on top of me”). Based on
the input from the experts, we need to adjust the
linguistic structure and use of words to make the
items’ readability better and avoid the participants
get confused. Then we revised both items according
all of the suggestion and then pilot tested the EPDS
to the participants.
Table 2: Computation of I-CVI and S-CVI of the
EPDS with three expert raters
Item Number in Agreements Item CVI
13 1
23 1
33 1
43 1
53 1
63 1
73 1
83 1
93 1
10 3 1
Mean I-CVI = 1,00
S-CVI = 1,00
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
412
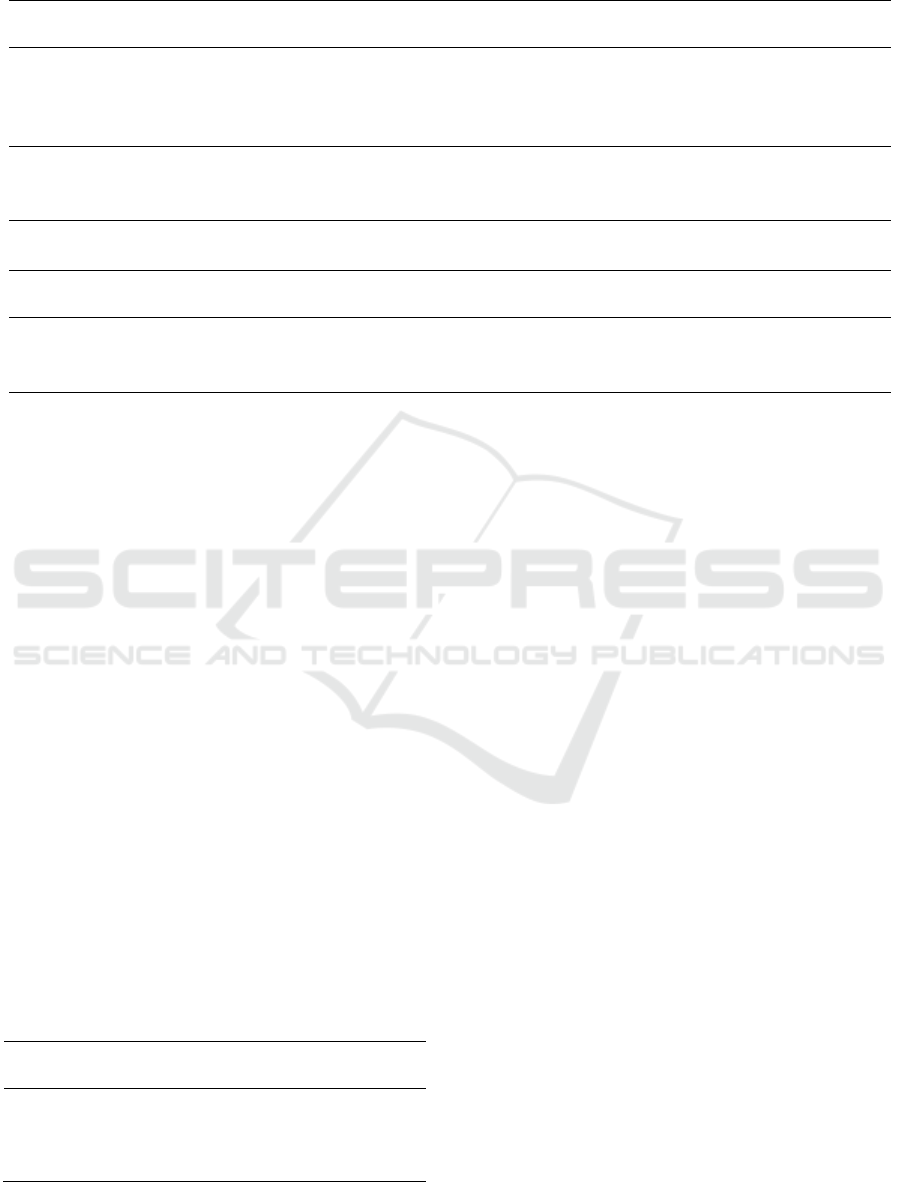
Tabel 3: Factor Loading Postpartum Depression – second order unidimensional model
Dimension Item
Factor Loading
Coefficients
Std. Error T-value Notes
Depression
ITEM-4 0,657 0,050 13.128
ITEM-5 0,698 0,047 14.878
ITEM-9 0,708 0,053 13.467
ITEM-10 0,684 0,078 8.820
Anxiety
ITEM-2 0,535 0,059 9.113
ITEM-3 0.651 0,054 12.068
ITEM-7 0.631 0,061 10.421
Anhedon
ITEM-1 0.434 0,109 3.993
ITEM-8 0.471 0,102 4.625
Factor Dimension
Factor Loading
Coefficients
Std. Error T-value Notes
Postpartum
Depression
Depression 0.963 0.068 14.098
Anxiety 0.812 0.071 11.499
Anhedon 1.184 0.228 5.190
Reliability Study
Reliability was estimated by the measure of the
internal consistency using the Cronbach’s alpha
coefficient. The internal consistency assessed for the
global EPDS scale was 0.706.
Factor Analysis Study
Our factor analysis suggests that a three factor
model would be better fit than a unidimensional one.
In Touhy and McVey’s (2008) confirmatory
analysis, three factors were found; which were
identified as ‘non-specific depressive symptoms’
(items 4, 5, 9, 10), ‘anhedonia’ (items 1, 6, 8) and
‘anxiety’ (items 2, 3, 7). Based on the first order
unidimensional model, item number six was found
not valid since its inter-item correlation is zero,
which means this item is not clearly measure the
dimensions it wants to measure. Construct validity
measurement shows that the P value > 0.05 and
RMSEA < 0.050. This means that postpartum
depression model second order unidimensional was
fit with the data. The P value index and RMSEA will
be presented in table below:
Tabel 4: Model fit criterion – EPDS second order
unidimensional
Model Fit
Criterion
Model Fit Index
Chi Square 31.049
P Value 0.1524
RMSEA 0.034
CFI 0.988
4 DISCUSSIONS
Our study confirms that this Indonesian version of
EPDS is a good tool for screening depression after
childbirth in mothers, in line with the conclusion of
some previous studies on EPDS validations (Cox,
Holden & Sagovsky, 1987; Adouard dkk., 2005).
There are some limitations must be considered along
the research process. Although it has pretty good
face validity for the mothers, result shown that this
Indonesian EPDS has one item classified as not
valid, that is item number six. CVI, inter-item
correlation and factor analysis proofed that item
number six is not good enough to measure
depression. Based on the suggestions the experts
gave upon item number six, we need further research
to retest the revised and reviewed version of item
number six. We assumed that it might be related
with the diction used to make translated version of
item six that is not fit with the cultural values and
way of living of Indonesian people.
For further research, there are some things that
we have to explore more about EPDS in Indonesian
language, such as the sensitivity of the cut-off score,
broaden the number and diversity of the sample, and
try to explore the concurrent or discriminant
evidence to continue the validation study.
Edinburgh Postpartum Depression Scale: Psychometric Evaluation of the Indonesian Version
413

REFERENCES
Adouard, F., Glangeaud-Freudenthal, N. M. C., & Golse,
B. (2005). Validation of the Edinburgh postnatal
depression scale (EPDS) in a sample of women with
high-risk pregnancies in France. Archives of Women’s
Mental Health, 8, 89-95.
Blum, L. D. (2007). Psychodinamics of Postpartum
Depression. Journal of Psychoanalytic Psychology,
24(1), 45-62.
Choudhury, M.D., Counts, S., & Horvitz, E. (2013).
Predicting Postpartum Changes in Emotion and
Behavior via Social Media. Paper presented at CHI
2013: Changing Perspective, Paris, France.
Clark, R., Tluczek, A., & Wenzel, A. (2003).
Psychotherapy for postpartum depression: a
preliminary report. American Journal of
Orthopsychiatry, 73(4), 441-454.
Cox, J., Holden, J., & Sagovsky, R. (1987). Detection of
postnatal depression: Development of the 10-item
Edinburgh Postnatal Depression Scale. British Journal
of Psychiatry, 105, 782-786.
Cox, J., & Holden, J. (2003). Perinatal Mental Health: A
Guide to the Edinburgh Postnatal Depression Scale
(EPDS). London: Gaskel – The Royal College of
Psychiatrists.
Gjerdingen, D.K., Froberg, D.G., Chaloner, K.M., &
McGovern, P.M. (1993). Changes in Women's
Physical Health During the First Postpartum Year.
Archieve of Family Medicine, 2, 277-283.
Guedeney, N., & Fermanian, J. (1998). Validation study of
the French version of the Edinburgh Postnatal
Depression Scale (EPDS): new results about use and
psychometric properties. Eur Psychiatry, 13, 83-89.
Lynn, M.R. (1986). Determination and quantification of
content validity. Nursing Research, 35, 382–385.
O'Hara, M. W. (1995). Postpartum Depression: Causes
and Consequences. New York: Springer-Verlag.
Touhy, A., & McVey, C. (2008). Subscales measuring
symptoms of non-specific depression, anhedonia, and
anxiety in the Edinburgh Postnatal Depression Scale.
British Journal of Clinical Psychology, 47, 153-169.
Venis, J. A., & McCloskey, S. (2008). Postpartum
Depression Demystified: An Essential Guide for
Understanding and Overcoming the Most Common
Complication after Childbirth. New York: Marlowe
& Company.
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
414
