
Reduce Stigmatization towards Schizophrenic Patients using
Acceptance and Commitment Therapy
Astri Haryanti and Nurul Hartini
Faculty of Psychology, Universitas Airlangga, Surabaya, Indonesia
Keywords: Acceptance and Commitment Therapy, Family, Schizophrenia, Stigma.
Abstract: People with mental disorders are more vulnerable to stigmas in society. Schizophrenia is a stigmatized
mental disorder. Stigmas can cause people with mental disorders, such as schizophrenia, to not receive the
right treatment. Families can associate with the stigmatization of the patient. Stigmatization from their
family can worsen the prognosis. Acceptance and Commitment Therapy (ACT) is an intervention that has
been proven to reduce stigmatization. This therapy encourages individuals to receive the internal experience
that occurs without trying to judge and simultaneously establish the behaviors that serve as the objectives to
be achieved. This research used quasi-experimental design using a single-subject design on four participants
(caregivers). Data collection techniques using the Attribution Questionnaire-27 (AQ-27). Data analysis was
conducted by using visual analysis to observe changes in each subject. The results of data analysis show that
Acceptance and Commitment Therapy can reduce stigmatization in each caregiver to schizophrenic patients.
The findings of this study can serve as a basis in supporting and improving families’ acceptance of patients’
conditions, to provide a better view of schizophrenic patients.
1 INTRODUCTION
Mental health problems in Indonesia need to receive
more attention because the number of mental
disorders continues to increase, creating a burden on
the state and a decline in human productivity over
the long term (Minister of Health Republic of
Indonesia, 2016). Based on the World Health
Organization (WHO) data (2017), mental health
problems such as depression are suffered by more
than 300 million people of all ages around the world,
and the number of people with schizophrenia
problems based on WHO data (2018) is more than
21 million people worldwide. In Indonesia, based
on data from Indonesia Health Research (Riskesdas)
2013 (Minister of Health Republic of Indonesia,
2016) revealed the prevalence of severe mental
disorders, such as schizophrenia reached about
400,000 people or as many as 1.7 per 1,000 people.
People with psychiatric problems are more
vulnerable to stigmas in society. Stigmas occur when
people give different labels to humans and mix
beliefs in with the culture of unwanted people or
negative stereotypes (Link and Phelan, 2001).
Stigmatization as described by the Goffman concept
(1963 as cited in Overton and Medina, 2008) was
related to social identity. He discussed that people
are stigmatized when they become disfavored or
rejected in society and then they become outcasts.
According to WHO (2016), stigma, discrimination,
and human rights violations are common in people
with schizophrenia. People with psychotic disorders
also have a high risk of human right violations, such
as long-term confinement in a shelter institution.
Stigma, discrimination, and the inability to
recognize mental disorders are still a major obstacle
to treatment. In Indonesia, the incorrect assumption
is made that mental disorders are related to the
supernatural (Minister of Health Republic of
Indonesia, 2015). Schizophrenic patients are also
often regarded as strange and dangerous people so
they do not immediately receive medical treatment
but are hidden or taken to “orang pintar” (Hawari,
2012). The conditions of schizophrenic patients
require attention regarding various aspects. Gerety
and Edwards (2014) revealed that schizophrenia can
affect someone’s well-being, shorten their life, and
can be one of the main causes of global disability.
This condition is often ignored and misunderstood
and is a heavy burden on the individual, family
members, and caregivers.
Haryanti, A. and Hartini, N.
Reduce Stigmatization towards Schizophrenic Patients using Acceptance and Commitment Therapy.
DOI: 10.5220/0008588002610266
In Proceedings of the 3rd International Conference on Psychology in Health, Educational, Social, and Organizational Settings (ICP-HESOS 2018) - Improving Mental Health and Harmony in
Global Community, pages 261-266
ISBN: 978-989-758-435-0
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
261

There has been no single treatment for
schizophrenia until now, but patients may have to
undergo lifelong treatment. Effective treatment for
patient with schizophrenia is medication and
psychosocial support (WHO, 2016). Families, as
part of providing support to schizophrenic patients,
have an important role in their treatment. Care and
the presence of a patient’s family members are
considered necessary because their involvement will
support the patient recovery process (Setyanto,
Hartini and Alfian, 2017).
Families, who are an important part of handling
people with mental disorders, certainly do not all
accept the fact that their family members are
suffering from a disorder (Community Care for
People with Schizophrenia in India, 2012). Families
can become agents of stigmatization due to a lack of
adequate information and resources and the burden
of daily care that leads to strong social exclusion
behavior and the family’s distrust during recovery
(Sousa, Marques, Curral and Queiros, 2012). Living
with a patient with a mental disorder in a family
context can lead to a variety of negative emotions,
including fear of the patient’s reactions and
behavior, especially when the patient becomes
aggressive, which is often unpredictable. A family
may feel threatened by the patient, thus reject
acceptance and trigger the patient’s withdrawal
(Vicente, Mariano, Paiano, Waidman, and Marcon,
2013). Therefore, if a family is not ready when the
patient leaves hospital and returns to the family and
community, their attitude will tend to lead to
possible stigma and prejudice, even aggression
towards the patient.
Stigma is one of the factors that inhibits
intervention treatment; however, specific action to
reduce stigma in various mental illnesses has proved
beneficial and achieved better results. Reducing
stigma can be a way to reduce the risk of recurrence
and worse outcomes caused by the a stigmatized
environment (Shrivastava, Johnson, and Bureau,
2010).
Masuda et al. (2009) reveal that a high stigma of
mental health is associated with high psychological
distress. This condition is due to reducing
psychological flexibility. Psychological flexibility is
the ability to be open and full of any experience,
which drives value that leads to a worthwhile goal
(Hayes, Luoma, Bond, Masuda and Lilis, 2006, in
Masuda and Latzman, 2011). Acceptance and
commitment therapy (ACT) is proven to provide
positive clinical outcomes to improve psychological
flexibility (Hayes et al., 2006).
Several studies have shown that acceptance and
commitment therapy (ACT) can reduce stigma.
Masuda et al., (2007) differentiate the provision of
ACT and stigma-related education to people with
psychological disorders. The results showed that
both interventions could reduce the stigma attached
to psychological disorders. Participants with
emotions avoid, blend in with their thinking, and
unable to take value from difficult thoughts and
feelings, and when given educational interventions,
they are unable to benefit from such interventions.
This is in contrast to participants who received ACT
intervention, suggesting that interventions can
reduce their stigmatization.
Based on the above, it is necessary to provide
treatment in the form of acceptance and commitment
therapy to families to reduce their stigmatization
towards schizophrenia patients. The treatment is
expected to develop new understanding in increasing
the acceptance of family members who are affected
by schizophrenia. Finally, this is an effort to reduce
stigma and discrimination for people with mental
disorders, which result in the threat of human rights
on the deprivation experienced by mental health
patients.
2 METHOD
The research was conducted using a quasi-
experimental design, using single-subject design
with a reversal A-B design category. The aim of this
research is to know understand acceptance and
commitment therapy to reduce the stigmatization of
a family towards a schizophrenic patient in the
family. Inclusion criteria of the subjects in this study
were one family member who treated the
schizophrenia patient and still had a negative
judgment on the patient, which was measured using
the attribution questionnaire (AQ)-27 resulting in the
medium to high range. Exclusion criteria is domicile
outside the city of Surabaya. Based on the
measurement results there were four research
subjects.
This research used the attribution questionnaire
(AQ)-27 and the acceptance and action
questionnaire-stigma (AAQ-S). AQ-27 was
developed by Corrigan (2012) and consisted of nine
stereotypes of people with mental disorders,
including blame, anger, pity, help, dangerous, fear,
avoidance, separation, and coercion. Questionnaires
from each stereotype consisted of three items so
altogether there are 27 items. Data collection using
AAQ to measure the psychological flexibility that is
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
262
associated with stigmatization. AAQ-S consists of
21 items with a reliability of 0.84.
Intervention using acceptance and commitment
therapy developed from the research of Masuda et
al. (2007) based on the manual acceptance and
commitment therapy (ACT) by Hayes et al. (1999).
Interventions were conducted based on six basic
principles of ACT compiled into five sessions,
including the discussion of problems and practice of
acceptance, diffusion, being present, self as context,
values, and committed action.
Data analysis of the single-subject design
research using visual analysis is presented in the line
graph. The graph shows a change in condition from
the baseline phase to the treatment phase. Visual
analysis provides a visualization of the changing
conditions of each research subject.
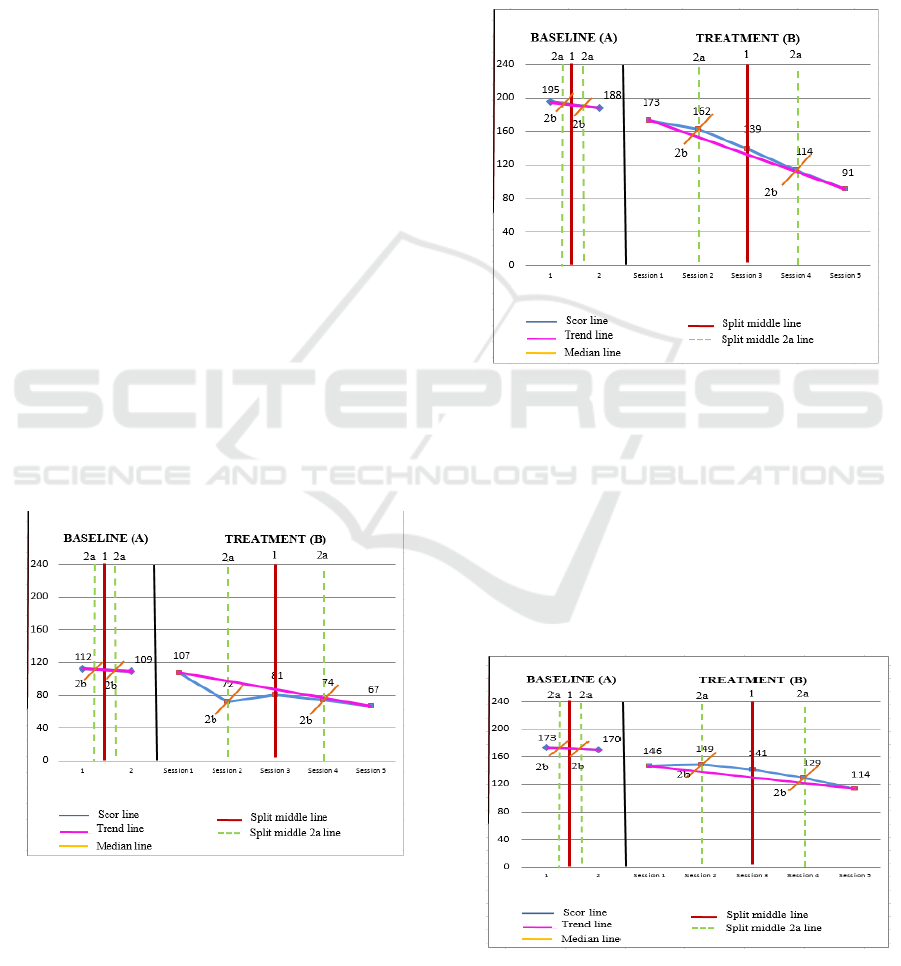
3 RESULT
The results of the visual analysis from each subject
is seen from the measurement with AQ-27. Data
collection were made twice during the baseline
phase (A) and five times during the treatment phase
(B). The condition of each can be explained as
follows:
3.1 Subject 1
Figure 1: Subject 1.
Subject 1 shows that there is a positive trend towards
the change in levels from the baseline phase to the
treatment phase, and that there is a two-point
reduction. The average values of the baseline phase
and the treatment phase decreases. This proves that
the subject’s condition has improved since the
treatment was given.
The analysis in subject 1 shows a 20% overlap of
data, which indicates that the treatment can influence
80% to reduce stigmatization.
3.2 Subject 2
Figure 2: Subject 2.
Subjects have decreased from the baseline phase to
treatment phase; this is shown by a downward trend
and positive change in level. The level change is
indicated by a score of 15 and an overlap of 0%,
which means there is a large influence on the
intervention.
3.3 Subject 3
Figure 3: Subject 3.
Reduce Stigmatization towards Schizophrenic Patients using Acceptance and Commitment Therapy
263
The result of the stability effect decreased, and
the level changed positively from the baseline to 24
after the intervention. It is also supported by overlap
percentages of 0%. This overlap condition indicates
that the intervention has a 100% effect, which is
positive in reducing stigmatization.
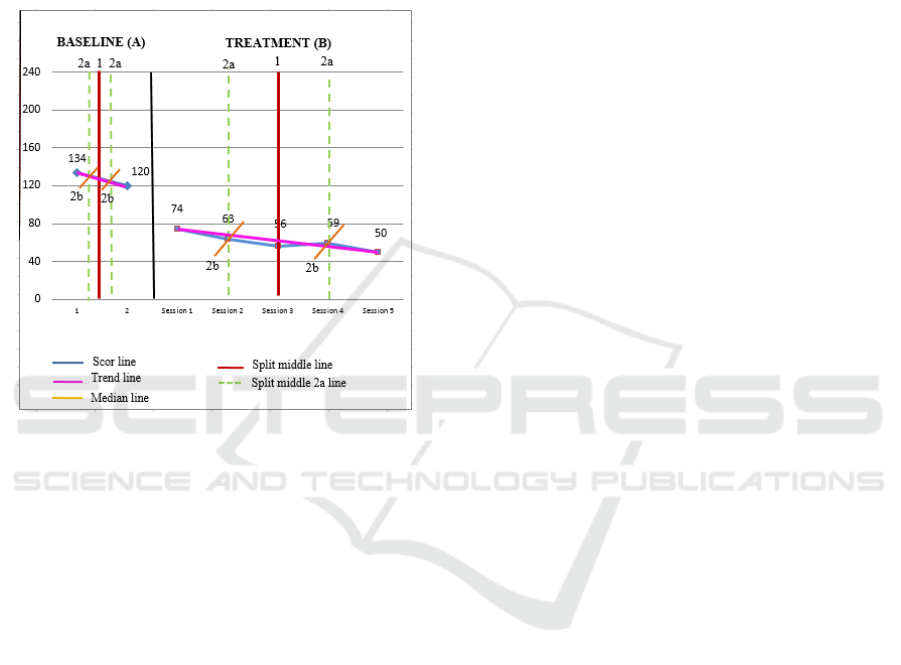
3.4 Subject 4
Figure 4: Subject 4
Subject 4 shows a decrease in stigmatization. This
can be seen from the stability effect with a
downward positive level change with a change in the
score of 46. Data shows an overlap of 0%, which
means that the intervention has a 100% effect. This
is substantial in reducing stigmatization.
3.5 Analysis AAQ-S
The result of the AAQ-S questionnaire analysis,
related to the psychological flexibility of each
subject is between 63 and 71. The entire subject
showed a high degree of psychological flexibility.
The results were not comparable to participants who
had low levels of psychological flexibility, so there
was only one group of participants with high
psychological flexibility.
4 DISCUSSION
Mental health problems are often associated with
stigma. Families often contribute to stigmatization.
Families may raise doubts over medical treatment
due to minimal changes in patients, which prompts
them to complain that the condition does not
demonstrate significant change. Also, there is an
emergence of the view that the patient is less
competent, which ultimately leads to the family’s
dissatisfaction with the patient’s condition. This
condition was also shown by some families of
relapsing study subjects; a lack of change in patients
causes the family to be disappointed with the
condition of the patients.
The results showed that acceptance and
commitment therapy can reduce the stigmatization
of schizophrenia patients for a family. Acceptance
and commitment therapy (ACT) in reducing
stigmatization is in line with previous studies.
Masuda et al. (2007 shows that acceptance and
commitment therapy can reduce stigmatization in
subjects with either low or high levels of
psychological flexibility. In this study, the overall
subjects had high psychological flexibility. This will
ultimately make the subject’s condition to readily
improve over the course of the intervention process
since act itself attributes the role of psychological
flexibility in providing intervention.
Psychological flexibility is the process of
engagement with personal psychological events such
as thoughts, feelings without judgement, evaluations,
alterations, corrections or regulations. Psychological
flexibility enables a person to accept all events
without judgment, even if they are seemingly
negative thoughts and feelings, which ultimately
becomes a possibility for a person to have those
thoughts and feelings without making the impact of
those thoughts and feelings a truth or reality
(Masuda et al., 2009).
Psychological flexibility is associated with
mental health stigma. Mental health stigma is closely
related to negative psychological outcomes for
people who are stigmatized, including those with
psychological health disorders. Psychological
flexibility is found to be inversely related to mental
health stigma and negative psychological outcomes.
Further analysis revealed that the relationship
between mental health stigma and poor
psychological outcomes was partially considered by
such psychological flexibility (Masuda et al., 2009).
These conditions illustrate from the research subjects
that when they have high psychological flexibility, it
is easier for them to lower the stigma they have,
including the behavior they bring, and the burden
they feel to experience a positive change. This is in
line with research conducted by Hayes et al (2004)
to reduce the stigmatization of drug addict
counselors to their clients through ACT. The results
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
264

indicate that the stigmatization attitudes of the
counselor decreases after the intervention is
delivered. The intervention can reduce the burnout
of the counselor so that the intervention, in addition
to lowering stigma, also has the influence to promote
the welfare and effectiveness of their
professionalism.
In the family, acceptance is also an important
part of reducing stigmatization of schizophrenic
patients. Acceptance is an important part of
behavioral interventions, including ACT (Cordova et
al., 2001). Acceptance as an important part of the
ACT intervention process and is related to
psychological flexibility. ACT can increase
psychological flexibility to gain a more meaningful
life by directing the values of life (Butler, 2015).
Acceptance is part of creating a warm relationship,
fixing emotional issues, coping with mismatches,
and irreconcilable differences and problems that
cannot be resolved. Paul and Nadkarni (2014) state
that family support is an important part of stigma for
schizophrenic patients. Some families play a strong
role in supporting people recovering from
schizophrenia by expanding family acceptance to
reduce stigma and discrimination in schizophrenic
patients.
5 CONCLUSION
Based on the results of data analysis and the
discussion of research, it can be concluded that
acceptance and commitment therapy can reduce
stigmatization towards schizophrenic patients in
families. Reducing the stigmatization of each subject
is indicated by changes in the different
psychological dynamics between subjects. The
findings of this study can serve as a basis in helping
to increase family acceptance of the patient’s
condition to provide a better view of schizophrenic
patients. These conditions can improve the quality of
the relationship between the family and the patient to
improve their welfare and provide a better quality of
life.
REFERENCES
Amalia, E. and Sarosa, Y. S., 2015. Peran keluarga pada
penanganan skizofrenia. In: Lebih dekat dengan
skizofrenia. Surabaya: BKKM Fakultas Kedokteran
Universitas Airlangga, pp. 77-88.
Butler, L. et al., 2015. Running acceptance and
commitment therapy groups for psychosis in
community settings. Journal of Contextual Behavioral
Science.
COPSI, 2012. A manual for working with people with
schizophrenia and their families. India: Community
Care for People with Schizophrenia in India.
Corrigan, P., 2012. A toolkit for evaluating programs
meant to erase the stigma of mental illness. s.l.:Illionis
Institute of Technology.
Depression: Let's talk. (2017, 7 April). World Health
Organization [on-line]. Retrieved at 8 Mei 2017 from
http://www.who.int/mental_health/management/depres
sion/en/
Garety, P. A. and Edwards, T. M., 2014. Psychological
interventon in schizophrenia. Dalam: Living with
schizophrenia. USA: World Federation for Mental
Health, pp. 20-22.
Gaudino, B. A. and Herbert, J. D., 2006. Acute treatment
of inpatient with psychotic symptoms using
acceptance and commitment therapy: Pilot result.
Behavior Research and Therapy, Volume 44, pp. 415-
437.
Hawari, D., 2012. Skizofrenia: Pendekatan holistik (bpss)
bio-psiko-sosial-spiritual edisi ketiga. Jakarta: FKUI.
Hayes, S. C. et al., 2004. The impact of acceptance and
commitment training and multicultural training on the
stigmatizing attitudes and professional burnout of
substance abuse counselors. Behavior Therapy,
Volume 35, pp. 821-835.
Hayes, S. C. et al., 2006. Acceptance and commitment
therapy: Model, process, and outcomes. Psychological
Faculty Publications, Volume 101.
Hayes, S. C., Strosahl, K. D. and Wilson, K. G., 1999.
Acceptance and commitment therapy: An experiental
approach to behavior change. New York: Guilford
Press.
Kementerian Kesehatan RI, 2013. Riset Kesehatan Dasar,
Jakarta: Badan Penelitian dan Pengembangan
Kesehatan.
Link, B. G. and Phelan, J. C., 2001. Conceptualizing
stigma. Annu. Rev. Social, Volume 27, pp. 363-385.
Masuda, A. et al., 2009. The relation between
psychological flexibility and mental health stigma in
acceptance and commitment therapy: A preliminary
process investigation. Behavior and Social Issues,
Volume 18, pp. 25-40.
Masuda, A. and Latzman, R. D., 2011. Examining
association among factor-analitycally derived
components of mental health stigma, distress, and
psychoogical flexibility. Personality and Individual
Differences, Volume 51, pp. 435-438.
Overton, S. L. and Medina, S. L., 2008. The stigma of
mental illness. Journal of Counseling & Development,
Volume 86, pp. 146-151.
Paul, S. and Nadkarni, V. V., 2014. A qualitative study on
family acceptance, stigma, and discrimination of
persons with schizophrenia in an Indian metropolis.
International Social Work, 60(1), pp. 84-99.
Peran Keluarga Dukung Kesehatan Jiwa Masyarakat
(2016, 6 October). Minister of Health Republic of
Indonesia [on-line]. Retrieved at 8 Mei 2017 from
Reduce Stigmatization towards Schizophrenic Patients using Acceptance and Commitment Therapy
265

http://www.depkes.go.id/article/view/16100700005/pe
ran-keluarga-dukung-kesehatan-jiwa-masyarakat.html
Perilaku Bermartabat Bantu Pulihkan Gangguan Jiwa
(2015, October 10). Minister of Health Republic of
Indonesia [on-line]. Retrieved at 4 Maret 2017 from
http://www.depkes.go.id/pdf.php?id=15101900005.
Setyanto, A. T., Hartini, N. and Alfian, I. N., 2017.
Penerapan social support untuk meningkatkan
kemandirian pada penderita skizofrenia. Wacana,
9(17).
Shrivastava, A., Johnston, M. and Bureau, Y., 2012.
Stigma of mental illness-1: Clinical Reflections. Mens
Sana Monogr, pp. 70-84.
Sousa, S. d., Marques, A., Curral, R. and Queiros, C.,
2012. Stigmatizing attitudes in relatives of people with
schizophrenia: a study using the attribution
questionnaire AQ-27. Trends Psychiatric Psychther,
34(2), pp. 186-197.
Stop Stigma dan Diskriminasi Terhadap Orang dengan
Gangguan Jiwa (2014, Oktober 10). Minister of Health
Republic of Indonesia [on-line]. Retrieved at 2 Maret
2017 from
http://www.depkes.go.id/article/view/201410270011/s
top-stigma-dan- diskriminasi-terhadap-orang-dengan-
gangguan-jiwa-odgj.html.
Vicente, J. B. et al., 2013. Acceptance of patients with
mental illness: A family perspective. Rev Gaucha
Enferm, 34(2), pp. 54-61.
ICP-HESOS 2018 - International Conference on Psychology in Health, Educational, Social, and Organizational Settings
266
