
The Effectiveness of Kegel Exercise or Pelvic Floor Muscle Training
to Incontinence Urine for Client Post Trans Urethral Resection of
The Prostate
A Systematic Review
Yani Erniyawati
1
, Kusnanto
1
and Padoli
2
1
Faculty of Nursing, Universitas Airlangga, Kampus C Mulyorejo Surabaya 60115, Indonesia
2
Health Polytechnic State of Surabaya, Jl. Pucang Jajar Tengah 56 Surabaya, Indonesia
Keywords: Kegel Exercise or Pelvic Floor Muscle Training, Urine Incontinence, Trans Urethral Resection of The
Prostate.
Abstract: Background: Incontinence of urine found for client post a trans urethral resection of the prostate after the
release of the lapse of a catheter. Kegel exercise or Pelvic Floor Muscle Training useful to resolve
incontinence of urine. This exercise can increase muscle power of pelvic. Objective: The purpose of this
article was to explore research finding about effectiveness kegel exercise or pelvic floor muscle training client
with incontinence of urine post trans urethral resection of the prostate. Methods: The search was carried in
some data based electronically with use health discriptors pelvic floor muscle training and kegel exercise and
incontinence urine and prostatectomy within the last ten years published in English. Results on the search was
13 journals that meet the criteria. Conclusion: Kegel exercise or pelvic floor muscle training effective to
reduce incontinence of urine, improve erectil function cost and care more effective and improve the quality
of life significantly. Need more research on the effectiveness of kegel exercise or pelvic floor muscle training
to urinary incontinence, erectil function and quality of live for client post trans urethral resection of the
prostate on the duration of the execution of the exercise.
1 INTRODUCTION
Urinary incontinence (IU) is a disorder of the
fulfillment of elimination of urine. Urinary
incontinence can be a passage of urine, sometimes
only a very small amount (a few drops), very much,
or uncontrolled (occurring outside the desire)
(Smeltzer, 2009). IU is found on the client post-TURP
or Trans Urethral Resection of the Prostate when the
first control after the release of the catheter hose.
According Bruschini et al.2011, IU in the surgery of
benign prostatic hyperplasia (BPH) is rare, but 30-
40% of clients experiencing early IU.
According Bruschini et al., 2011IUcause post-
TURP very multufaktorial, including urinary
sphincter insufficiency (USI) or bladder dysfunction
(BD), which is defined as a decrease in development
or detrusor overactivity (DO). USI occur as a result
of injury to the sphincter mechanism andincontinence
is usually associated with BladderDisfungtion (BD),
which includes detrusor overactivity (DO).
Additionally DO associated with increased bladder
muscle tension with urinary retention that can lead to
IU.
Kegel exercises are exercises to strengthen the
pelvic floor muscles that will improve urethral
resistance and urinary control (Smeltzer, 2009). This
exercise was originally developed by Arnold Kegel in
1948 as a method of controlling incontinence in
women after childbirth.
This exercise is done by strained muscles hold off
on pubbocogeus (PC) (Widianti, 2010). Kegel.
exercise can be used to reduce the symptoms of all
types of urinary incontinence (Dumoulin, 2010)..
Kegel is done twice a day for 15 minutes for 6-8
seconds with a break of 6 seconds is very effective for
urinary incontinence in women (Kashanian et al.,
2011).
Kegel exercise has been used as a treatment for
urinary incontinence in elderly women (Aslan et al.,
2008; (Kashanian, et al, 2011), lowered complaint
dribling on the client post-TURP (Madjid, 2011),
Erniyawati, Y., Kusnanto, . and Padoli, .
The Effectiveness of Kegel Exercise or Pelvic Floor Muscle Training to Incontinence Urine for Client Post Trans Urethral Resection of The Prostate.
DOI: 10.5220/0008331807250733
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 725-733
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
725

accelerate wound healing perinium on mother normal
post partum (Ridlayanti, et al., 2011), effective
against urinary incontinence and quality of life in
post-TURP client ( (Zhang, et al, 2007).
Results of previous systematic review showed
that Kegel exercise is done before surgery had a
significant effect on urinary incontinence after TURP.
This review is conducted to assess the effectiveness
of Kegel exercises for urinary incontinence in the
client after TURP surgery.
2 METHODS
Research articles obtained from a search on line
English language articles in several databases include
Proquest, Science Direct, Jural nurses, Google
Scholar in the last 10 years (2007-2017). The
keywords used are pelvic floor muscle training and
Kegel exercise and incontinence of urine and
prostatectomy within the last ten years published in
English.
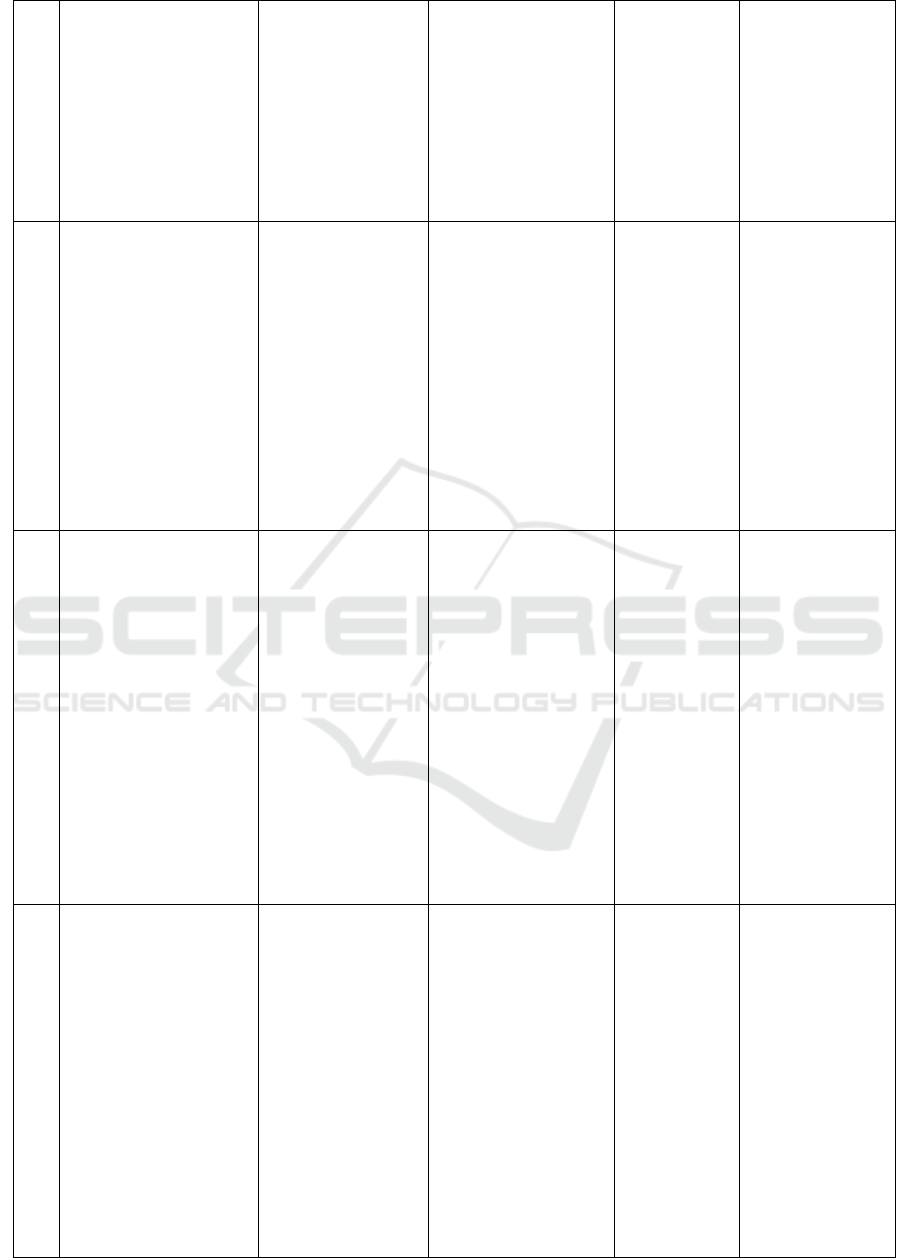
2.1 Selection Research
Results obtained 657 journals were selected, leaving
15 full text journals titled pelvic floor muscle training
or Kegel exercise. Of the 15 articles were selected and
gained back 13 journals that met inclusion criteria.
The inclusion criteria of this study were: 1) The
reporting of interventions Pelvic Floor Muscle
Training (PMFT) or Kegel exercise that aims to
reduce urinary incontinence, 2) uses the randomized
studies (RCT), 3) Original Research, 4) Do the clients
who suffered incontinence urine, 5) Published in
English.
Figure 1: Alogaritme Pencarian Artikel.
3 RESULTS
This review examines the effect of Kegel exercise or
Pelvic floor Muscle Training (PMFT) against urinary
incontinence (10 journals), quality of life (2 journals),
erectile dysfunction (1 journal). Design on 13
journals reviewed were all using the RCT were on
level 2 of 7 degrees level of evidence to the random
allocation. Ably uniform type of intervention that is
Pelvic floor muscle training (PMFT) or Kegel
exercise (KE).
PMFT or TO can degrade or improve urinary
incontinence significantly in the women (Kashanian
et al., 2011), can treat urinary incontinence in the
elderly (Aslan et al., 2008), showed a significant
increase of the resistance of the pelvic floor muscles
(Tibaek et al., 2007), improving the quality of life
(Centemero et al., 2010, Geraerts et al., 2015),
improves erectile function Geraerts et al., 2015),
menurunka urinary incontinence in the client post-
prostatectomy (Tibaek et al., 2007; Zhang, Strauss
and Laura, 2007; Overga, 2008; Centemero et al.,
2010; Yamanishi et al., 2010; Glazener et al., 2011;
Goode et al., 2011; Tienforti et al., 2012; Geraerts et
al., 2013).
PMFT performed before surgery showed a
significant increase in the durability of the pelvic
floor muscle after TURP, although the clinical
relevance improving the status of urodynamic no
difference. Process in getting the research articles
that are relevant to the use of keywords, obtained 13
articles in accordance with the inclusion criteria, then
the article is extracted. From the data extraction
carried out several synthesis in order to provide an
overview of The Effectiveness of Kegel Exercise or
Pelvic Floor Muscle Training to Incontinence Urine
for Trans Urethral Client Post Resection of the
Prostate .. The results of the extraction of the
synthesized research article can be seen in the table
below:
(Tibaek et al.,2007). The instrument used is the
DAN-PSS-1 questionnaire. The procedure has been
standardized intervention carried out by a
physiotherapist experienced and do not know to
jamming and the results of the initial test (Tibaek et
al., 2007).
PMFT can improve urinary incontinence in
women with or without kegelmaster (Aslan et al.,
2008; Kashanian et al., 2011). Three questionnaires
were used Incontinence Quality of Life (IQOL),
Incontinence Impact Questionnaire (IIQ) and its
Search on line of english articles in some
database including Proquest, Science direct,
Jurnal Ners, Google Scholar in the last 10
years (2007-2017)
Health discriptors
pelvic floor muscle
training and kegel
exercise and
incontinence urine and
prostatectomy
Eligible artikel
(n= 657)
Full text artikel
excludes, with
reason
(n= 15)
Artikel Full text
to review (n= 13)
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
726

complementary Urogenital Distress Inventory (UDI).
Pelvic floor muscle strength was evaluated using the
Oxford grading system (Kashanian et al., 2011).The
muscle strength was evaluated using digital tools
gained 52% in women who do PMFT and 48% who
did PMFT(Aslan et al., 2008).
Two journals were reviewed comparing the
effects of PMFT done since before and after post-
surgery (Centemero, et al, 2010) (Geraerts, et al,
2013). RESULTS p = 0.002, which means patients do
PMFT before and after surgery showed better results
compared to only do after surgery is PMFT
performed before surgery have an increased risk 0.41-
fold lower incontinence and 0.38-fold lower
incontinence in PMFT after surgery (Centemero, et
al, 2010).
One journal comparing whether behavioral
therapy with or without biofeedback and pelvic floor
electrical stimulation to the patient prostatectomy
urinary incontinence, urge incontinence episodes
showed an average decrease of 28 to 13 per week, or
a reduction of 55% after the behavioral therapy of
incontinence episodes while the average decline of 26
to 12 or 51% after the behavior and stimulation, but
there was no significant difference in the reduction of
incontinence between the treatment group and the
control group with p = 0.069 (Goode, et al, 2011)
Support groups can improve the effectiveness
PMFT (Zhang, et al, 2007). The group that only did
PMFT have a level higher urinary incontinence based
on a visual analog scale assessment of the group
PMFT a support group (4.7 vs. 3.2) and more groups
are using pads PMFT (85%) compared with the group
with the support group (50 (Zhang, et al, 2007).
Besides effect on urinary incontinence, PMFT
also affect erectile function in patients post
prostatectomi (Geraerts, et al, 2015). One is reviewed
journals show that PMFT can improve erectile
function in post-prostatectomy patients are
significantly (p = 0.0025) using the questionnaire
used is or International reindexs IIEF erectile function
(Geraerts, et al, 2015).
A decrease in urinary incontinence and erectile
function improvement has a positive correlation with
quality of life. Two journals state that kapatuhan
against PMFT can give a good effect on urinary
incontinence and quality of life (Zhang, et al, 2007)
(Centemero, et al, 2010)
4 DISCUSSION
The results of this review indicate that article 13
pelfic floor muscle training (PMFT) or Kegel exercise
effectively lower urinary incontinence, improve
erectile function and quality of life. In addition to the
single intervention that is PMFT, can also be
combined with a support group (Zhang, et al, 2007).
PMFT effective against urinary incontinence in men
due to the condition of the bladder muscles and
improved (Parekh in the (Zhang, et al, 2007)).
Research conducted (Zhang, et al, 2007) showed
that urinary incontinence in men better by combining
PMFT and support group. The combined effect
significantly to the quality of life especially in the
field of social events and the relationship of husband
and wife (Zhang, et al, 2007).
Research conducted by Goode et al.2011 states
that 16% of men who do PMFT with behavioral
therapy that can reduce the frequency of their urinary
incontinence is more than half the frequency. (Goode,
et al, 2011) also, say that the addition of biofeedback
and electrical stimulation did not promote behavioral
change in doing PMFT. Behavior terapy is a
technique that can be used to change a person's
behavior through teaching or improve their
knowledge (Goode, et al, 2011). This behavior occurs
because the changes after the teaching of the revenue,
one would think, act and behave (Notoatmojo
etal.,2012). Patients reflect behavioral therapy with a
positive attitude may be because the client has a
strong desire to heal and improve the quantity of their
lives.
Research conducted by (Overga, et al, 2008)
which distinguish whether there are differences
PMFT effect on urinary incontinence after radical
prostatectomy surgery guided by a physiotherapist to
be done alone showed that the group who received
training physiotherapist guided reduction of urinary
incontinence significantly more than their coaching
clients themselves with p = 0,001 with a time of 3
months. This is probably due to oversight,
respondents were more focused and to be serious in
doing the exercises. (Goode, et al, 2011) stated that
the client's behavior can be influenced by the
presence of a stimulus. The stimulus could be
anything, including guidance from a physiotherapist.
(Centemero, et al, 2010), (Geraerts, et al,
2013) states that PMFT were performed before
surgery and continued after surgery the results are
more significant in reducing urinary incontinence
than PMFT is done after surgery. This is likely caused
because the muscles of the pelvic longer getting
stimulation. To get the muscles of the body are
obvious, of course, will not be obtained in practice
only occasionally, the client should exercise regularly
followed by a gradual increase in training volume
within a specific time period. The combination of
The Effectiveness of Kegel Exercise or Pelvic Floor Muscle Training to Incontinence Urine for Client Post Trans Urethral Resection of The
Prostate
727

these two things will greatly affect muscle
enlargement process (Ongko et al., 2016).
Tibaek et al., 2006 proves that PMFT performed
before surgery resulted in a significant improvement
in pelvic floor muscle endurance after TURP is a
significant increase of 86% occurred after training (p
= 0.004). (Geraerts, et al, 2015) found that clients
with post radical prostatectomy (RP) who
experienced erectile disfunction at least 12 months
after RP after PMFT for 3 months to recover erectile
function better (P = 0.025) and showed an increase
klimaksuria with p = 0.004. This is probably due to
the PMFT conducted both before and after surgery
can improve the strength and pelvic floor muscle
mass and can accelerate blood circulation and
improve muscle bulbocavernosus. Widianti 2010
says that stimulation of the pelvic floor muscles will
build muscle mass that can strengthen the
pubococcygeus muscle (PC) supports muscle
bulbocavernosus and muscle iskhiokavernosus so as
to make the penis erect very loudly anytime they
want, improving blood circulation in the penis, can
enhance sexual stamina, increase the volume and the
intensity of ejaculation, improve urinary flow.
5 CONCLUSION
The purpose of this systematic review is to assess the
effectiveness of the use of pelfic floor muscle training
or Kegel exercise as a therapeutic intervention in
post-TURP urinary incontinence clients. Some
studies showed that significantly reduces urinary
incontinence, treatment costs, improve erectile
function and quality of life of the client. Further
studies on the duration of the execution of the
exercise.
REFERENCES
Aslan, E. et al. (2008) ‘Bladder training and Kegel exercises
for women with urinary complaints living in a rest
home’, Gerontology, 54(4), pp. 224–231. doi:
10.1159/000133565.
Bruschini, H. et al. (2011) ‘Urinary incontinence following
surgery for BPH: The role of aging on the incidence of
bladder dysfunction’, International Braz J Urol, 37(3),
pp. 380–386. doi: 10.1590/S1677-
55382011000300012.
Centemero, A. et al. (2010) ‘Preoperative Pelvic Floor
Muscle Exercise for Early Continence After Radical
Prostatectomy : A Randomised Controlled Study’, 57,
pp. 1039–1044. doi: 10.1016/j.eururo.2010.02.028.
Geraerts, I. et al. (2013) ‘Influence of Preoperative and
Postoperative Pelvic Floor Muscle Training ( PFMT )
Compared with Postoperative PFMT on Urinary
Incontinence After Radical Prostatectomy : A
Randomized Controlled Trial’, European Urology.
European Association of Urology, 64(5), pp. 766–772.
doi: 10.1016/j.eururo.2013.01.013.
Geraerts, I. et al. (2015) ‘Pelvic fl oor muscle training for
erectile dysfunction and climacturia 1 year after nerve
sparing radical prostatectomy : a randomized controlled
trial’. Nature Publishing Group, (August), pp. 1–5. doi:
10.1038/ijir.2015.24.
Glazener, C. et al. (2011) ‘Urinary incontinence in men
after formal one-to-one pelvic-floor muscle training
following radical prostatectomy or transurethral
resection of the prostate (MAPS): Two parallel
randomised controlled trials’, The Lancet. Elsevier Ltd,
378(9788), pp. 328–337. doi: 10.1016/S0140-
6736(11)60751-4.
Goode, P. S. et al. (2011) ‘Behavioral Therapy With or
Without Biofeedback and Pelvic Floor Electrical
Stimulation for Persistent Postprostatectomy
Incontinence’, 305(2).
Kashanian, M. et al. (2011) ‘European Journal of Obstetrics
& Gynecology and Reproductive Biology Evaluation of
the effect of pelvic floor muscle training ( PFMT or
Kegel exercise ) and assisted pelvic floor muscle
training ( APFMT ) by a resistance device (
Kegelmaster device ) on u’, 159, pp. 218–223. doi:
10.1016/j.ejogrb.2011.06.037.
Madjid, A., Irawaty, D. and Nuraini, T. (no date) ‘Pasien
Pasca Transurethral Resection of the Prostate Melalui
Kegel ’ S Excercise’.
Notoadmojo, S. (2012). Promosi Kesehatan dan Perilaku
Kesehatan. Jakarta: Rineka Cipta.
Ongko, J. 2016. Fitness Trainer Study Guide. APKI: Jakarta
Overga, M. (2008) ‘Does Physiotherapist-Guided Pelvic
Floor Muscle Training Reduce Urinary Incontinence
After Radical Prostatectomy ? A Randomised
Controlled Trial’, 54, pp. 438–448. doi:
10.1016/j.eururo.2008.04.021.
Smeltzer, S. C., Bare,B. (2009). Texbook of Medical
Surgical Medikal Nursing (11 th ed.) Philladelphia:
Lipincott Williams & Wilknis.
Tibaek, S. et al. (2007) ‘Pelvic floor muscle training before
transurethral resection of the prostate : A randomized ,
controlled , blinded study’, (November 2006). doi:
10.1080/00365590601183584.
Tienforti, D. et al. (2012) ‘Daniele Tienforti , Emilio Sacco
, Francesco Marangi , Alessandro D ’ Addessi , Marco
Racioppi , Gaetano Gulino , Francesco Pinto , Angelo
Totaro , Daniele D ’ Agostino and Pierfrancesco Bassi’,
pp. 1004–1011. doi: 10.1111/j.1464-410X.2012.10948.
Widianti, A. T., Proverawati, A. (2010). Senam Kesehatan
Aplikasi Senam Untuk Kesehatan. Yogyakarta: Nuha
Medika.
Yamanishi, T. et al. (2010) ‘Randomized, placebo
controlled study of electrical stimulation with pelvic
floor muscle training for severe urinary incontinence
after radical prostatectomy’, Journal of Urology.
Elsevier Inc., 184(5), pp. 2007–2012. doi:
10.1016/j.juro.2010.06.103.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
728
Zhang, A. Y., Strauss, G. J. and Laura, A. S. (2007) ‘and a
Support Group on Urinary Incontinence’, 34(1), pp 43
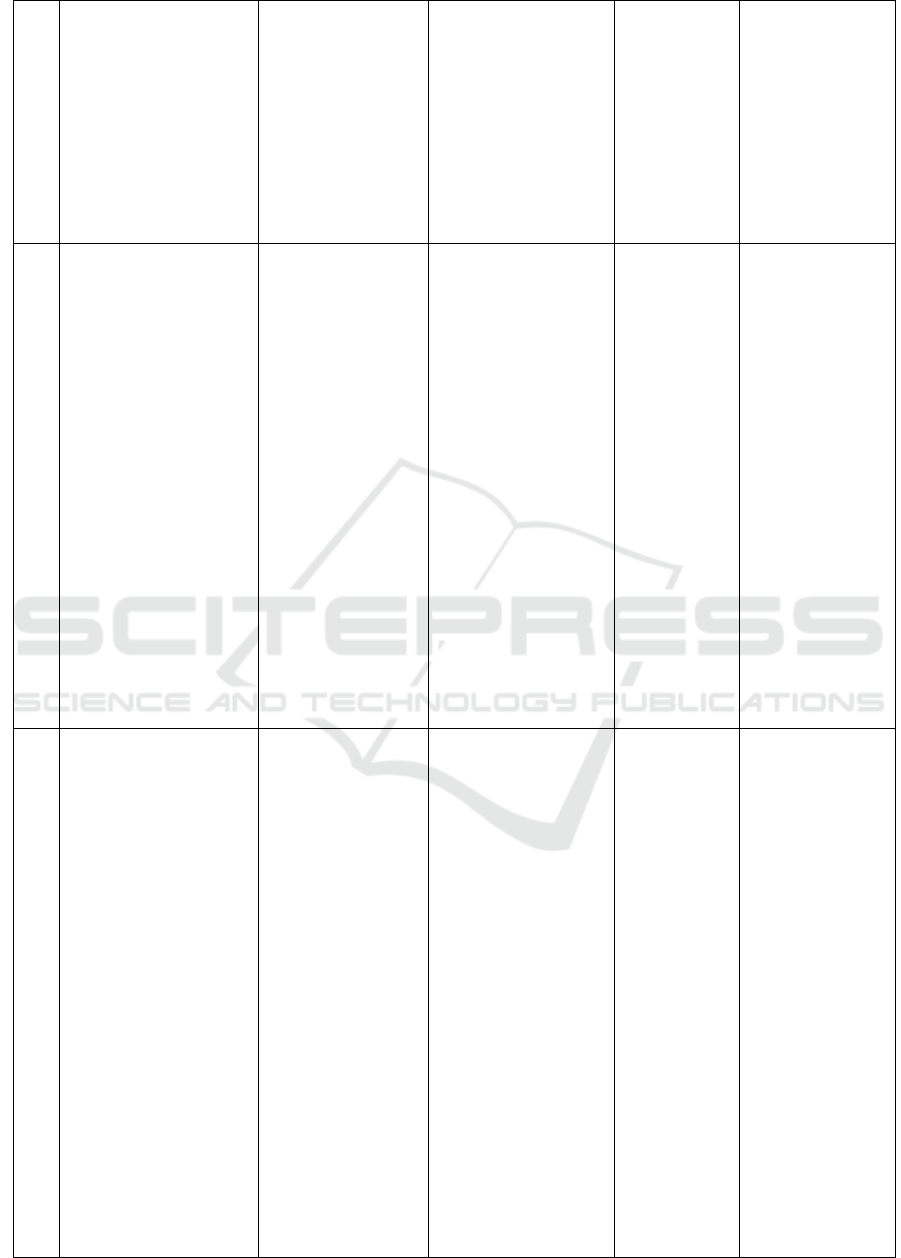
APPENDIX 2
No
Title
Design, Instrumen
Variable
Sample
Result
1
Evaluation of the effect
of pelvic floor muscle
training (PFMT or Kegel
exercise)
and assisted pelvic floor
muscle training
(APFMT) by a
resistance device
(Kegelmaster device) on
urinary incontinence in
women: a randomized
trial
Kashanian, M., Ali,
Shadab Shah., Nazemi,
Mitra., Bahasadri,
Shohreh.
2011
RCT
- Incontinence
Quality Of Life
(IQOL)
- Incontinence
Impact
Questionnaire
(IIQ)
- Urogenital
Distress Inventory
(UDI)
- pelvic floor muscle
training (PFMT or
Kegel exercise)
- assisted pelvic floor
muscle training
(APFMT) by a
resistance device
(Kegelmaster device)
- urinary incontinence
in women
A sample size
of 76 patients
(38 in each
group)
Pelvic floor
muscle exercises
(PMFT ) or Kegel
exercise with or
without the aid of
resistance which
device was
conducted twice a
day for 15 minutes
during 6-8 seconds
with breaks 6
seconds each
session with the
duration of 12
weeks does not
show a significant
difference which
means that both
this method
effective for the
repair of
incontinence of
urine in women.
2
Bladder Training and
Kegel Exercises for
Women with Urinary
Complaints Living in a
Rest Home.
Aslan, Ergul., Komurcu,
Nuran., Beji, Nezihe K.,
Yalcin, Onay. 2008
RCT
- Quality of Life
Scale,
- Mini-Mental Test
- The Rankin Scale
- Bladder Training
- Kegel Exercises
- Urinary Incontinence
for Women
Sample 64
patient, 33
treatment, 31
control. After
8 week and 6
month follew
up treatment
group 7
dropped and 1
died, control
group 5
dropped and 1
died.
Bladder
exercises and
Kegel exercises
performed on
women aged 65
years and over
with urge
incontinence
urgency for 6-8
weeks were found
to be statistically
and significantly
decreased in
frequency and
nocturia. So this
therapy can be
used easily as an
effective treatment
of urinary
incontinence in
elderly women
who live at home.
3
Pelvic floor muscle
training before
transurethral resection of
the prostate: A
RCT
- DAN-PSS-1
questionnaire
- Observation
- PMFT
- TURP
- 26 PMFT
group
- 23 control
group
Pelvic floor
muscle exercises
performed before
surgery showed a
significant
The Effectiveness of Kegel Exercise or Pelvic Floor Muscle Training to Incontinence Urine for Client Post Trans Urethral Resection of The
Prostate
729
randomized, controlled,
blinded study
Tibaek, S., Klarskov, P.,
Lund, H.B., Thomsen,
H., Andresen, H.,
Schmidt, J.C., &
Niemann, O.M. (2007)
increase muscle
endurance of the
post-TURP
muscle, although
clinically the
correlation of
post-TURP
urodynamic status
increase was no
difference
4
Preoperative Pelvic Floor
Muscle Exercise for Early
Continence After Radical
Prostatectomy
Centemero, P., Rigatti, L.,
Giraudo, D., Lazzeri, M.,
Lughezzani, G., Zugna,
D., Montorsi, F., Rigatti,
P., Guazzani, G. (2010).
RCT
- International
Continence
Society (ICS)
standards
- PMFT
- Early Continence
Intervention
group= 59
Control
group: 59
The results
obtained with
pelvic floor
muscle exercises
performed before
and continued
after prostate
surgery showed
significant results
can decrease
incontinence
incidence and
improve quality of
life.
5
Influence of Preoperative
and Postoperative Pelvic
Floor Muscle Training
(PFMT) Compared with
Postoperative PFMT on
Urinary Incontinence
After Radical
Prostatectomy
Geraerts, I., Poppel, H.
V., Devoogdt, N., Joniau,
S., Cleynenbreugel, B. V.,
Groef, A. D., Kampen, M.
V. (2013)
RCT
- visual analog
scale (VAS)
concerning their
subjective
feelings about UI
- Complete the
International
Prostate
Symptom Score
(IPSS) a
questionnaire to
assess voiding
symptoms.
- The King’s
Health
Questionnaire
(KHQ),
- PMFT
- Urinary
Incontinence
Experiment
group: 91
Control
group: 89
There was no
significant
difference in
PMFT results in
pre and post
patients with
postoperative, but
quality of life
improved more
rapidly in the
group performing
PMFT before and
after surgery.
6
Urinary incontinence in
men after formal one-to-
one pelvic-fl oor muscle
training following radical
prostatectomy or
transurethral resection of
the prostate (MAPS)
Glazener, C., Boachie, C.,
Buckley, B., Cochran, C,
et al. (2011)
RCT
- ICIQ-UI SF
questionnaire
- quality-adjusted
life year (QALY)
- PMFT
- Urinary
incontinence
- Quality of live
Trial 1:
intervention
group= 205
respondent,
control
group=206
respondent
Trial 3:
intervention
group= 220
respondent,
control
group=222
respondent
This study
compared the
effects of PMFT
on urinary
incontinence in
patients following
prostate radical
surgery and trans
urethral prostate
resection between
control and
intervention
groups. The
results obtained no
significant
differences
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
730
between the two
groups, ie, the
intervention did
not change the
incidence of
urinary
incontinence and
quality of life in
both groups and
reported no
adverse effects.
7
Does Physiotherapist-
Guided Pelvic Floor
Muscle Training Reduce
Urinary Incontinence
After Radical
Prostatectomy?
Overgard, M., Angelsen,
A., Lydersen, S.,
Merkued, S. (2008)
RCT
- the questionnaire
UCLA-PCI
(University of
California, Los
Angeles, Prostate
Cancer Index)
- PMFT
- Urinary
incontinence
Intervention
group= 42
(with PMFT)
Control
group= 43
(without
PMFT)
There was no
statistically
significant
difference for
PMFT performed
3 times 10
contractions daily
at home for 3
months, after 6
months there was
a clinical
difference and
after 1 year there
was a statistically
significant and
clinical difference
of PMFT effect in
reducing urinary
incontinence on
patients post
radical
prostatectom.
8
Randomized, Placebo
Controlled Study of
Electrical Stimulation
With Pelvic Floor Muscle
Training for Severe
Urinary Incontinence
After Radical
Prostatectomy
Yamanishi, T., Mizuno,
T., Watanabe, M., Honda,
M., Yoshida, K. (2010).
RCT
- ICIQ-SF
- KHQ
- Electrical
stimulation with
PMFT
- Incontinence
26
intervention
group
30 control
group
PMFT before and
continued after
surgery. For active
Stimulation 50 Hz
square wave 300
pulse duration and
5 seconds. At, 5
seconds off duty
cycle is applied for
15 minutes twice
daily with anal
electrode.
Stimulation of
shock is limited to
3 mA with 2 sec at
13 seconds found
that electrical
stimulation
combined with
PMFT can result
in recovery of
urinary
incontinence in
post-operative
The Effectiveness of Kegel Exercise or Pelvic Floor Muscle Training to Incontinence Urine for Client Post Trans Urethral Resection of The
Prostate
731

prostatectomy
patients every
month
9
Efficacy of an assisted
low-intensity programme
of perioperative pelvic fl
oor muscle training in
improving the recovery
of continence after
radical prostatectomy: a
randomized controlled
trial
Tienforti, D., Sacco, E.,
Marangi, F., et al. (2011)
RCT
- (International
Consultation on
Incontinence
Questionnaire on
Urinary
Incontinence [
ICIQ-UI ] [ ICIQ
]
- Overactive
Bladder [ OAB ]
- University of
California, Los
Angeles- Prostate
Cancer Index [
UCLA-PCI ] ,
- biofeedback (BFB)
combined with an
assisted low-
intensity
programme of
postoperative
perineal
physiokinesitherapy
in reducing the
incidence, duration
- urinary
incontinence
Overall, 34
consecutive
patients were
eligible and
32 were
available for
the fi nal
analysis: 16
patients for
each study
group
Pelvic floor
muscle exercises
performed three
times a day for 10
minutes with 5
contractions and 5
seconds of rest
after removal of
catheter tube at
home under
supervision and
evaluated thrice
for 6 months
showed that the
preoperative
biofeedback
combined with
PMFT was
significantly more
effective rather
than standard
treatments in
improving urinary
incontinence
recovery.
10
Effects of Combined
Pelvic Floor Muscle
Exercise and a Support
Group on Urinary
Incontinence and Quality
of Life of
Postprostatectomy
Patients
Zhang, A., Strauss, G. J.,
Siminoff, L. A. (2007)
RCT
- Los Angeles,
Prostate Cancer
Index
- American
Urological
Association
Symptom Index
- visual analog
scale (VAS)
- Combined Pelvic
Floor Muscle
Exercise and a
Support Group
- Urinary
Incontinence and
Quality of Life
Support
group= 14
Control
group= 15
PMFTs performed
four to seven days
per week at home
and attending bi-
weekly group
meetings have
lower urinary
incontinence rates.
11
Behavioral Therapy With
or Without Biofeedback
and Pelvic Floor
Electrical Stimulation for
Persistent
Postprostatectomy
Incontinence
Goode, P. S., Burgio, K.
I., Johnson, T. M., et al.
(2011)
RCT
- The American
Urological
ssociation (AUA-
7) symptom index
- InternationaL
ProstateSymptom
Score quality-of-
life question
- Behavioral Therapy
- Pelvic Floor
Electrical
Stimulation
- Persistent
Postprostatectomy
Incontinence
Behaviour :70
Behaviour
plus:70
Control: 68
Clients who were
in the PMFT
behavior therapy
group who
performed for 8
weeks with fifteen
contractions with
10 seconds of
relaxation had a
significant
decrease of an
average of 55% in
incontinence
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
732
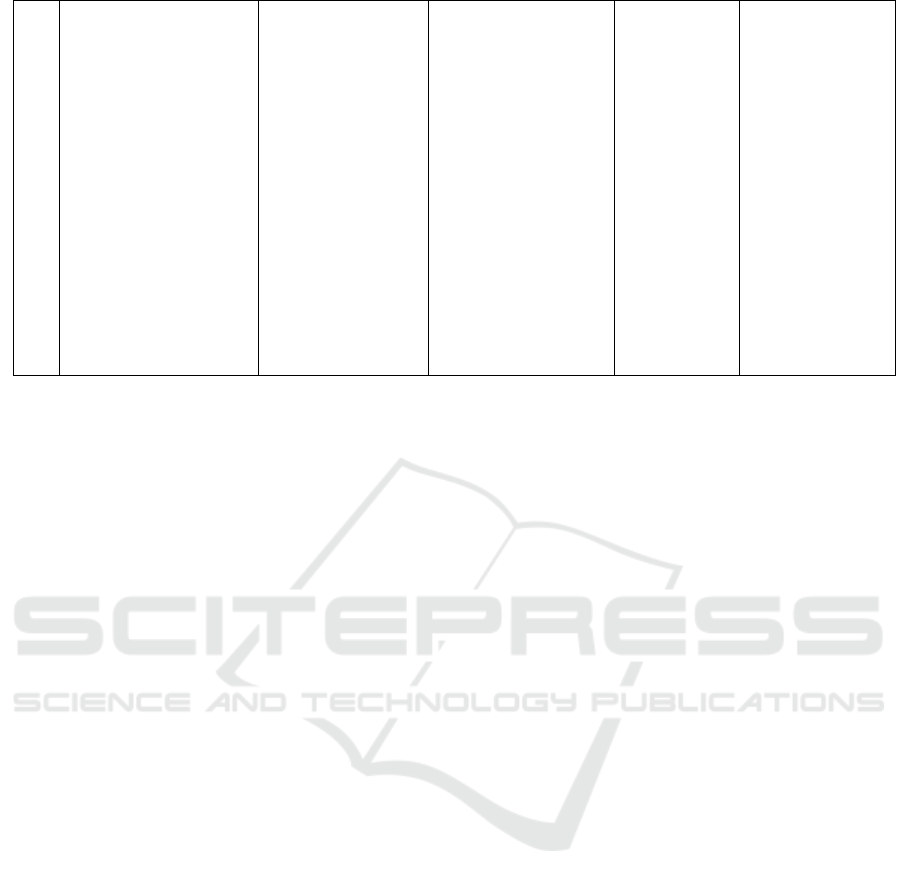
12
Pelvic floor muscle
training for erectile
dysfunction and
climacturia 1 year after
nerve sparing radical
prostatectomy: a
randomized controlled
trial
Geraerts., Poppel, H. V.,
Devoogdt, N. Et al (2015)
RCT
- IIEF-EF
- a visual analog
scale
- Pelvic floor muscle
training
- erectile dysfunction
Treatment
group: 16
Control
group: 17
Clients with post
radical
prostatectomy
(RP) who had
erectile
dysfunction at
least 12 months
after RP after
PMFT for 3
months
experienced better
erectile function
recovery with (P =
0.025) and showed
an increase in
climaxuria with p
= 0.004.
The Effectiveness of Kegel Exercise or Pelvic Floor Muscle Training to Incontinence Urine for Client Post Trans Urethral Resection of The
Prostate
733
