
Family Support Relationships with Patient Adaptation Ability above
with Diagnosis Hallucination of Post Care
Lela Nurlela, Meiana Harfika and Laelani Eka Novitasari
Sekolah Tinggi Ilmu Kesehatan Hang Tuah Surabaya
Keywords: Family Support, Adaptability, Hallucination.
Abstract: Hallucinations are one of the most common symptoms of mental disorder, considered a peculiarity of others
in relation to society and conditions in the family. Family is the main support system that plays a role to
provide direct care in good health and illness. The purpose of this study identified the relationship of family
support to the adaptability of outpatients with post hospital hallucinatory diagnosis. Design of quantitative
research in form of descriptive correlation, using non probability sampling technique with purposive sampling
approach. Samples taken were patients of post-treatment hallucination, as many as 10 people. Independent
variable is family support, and dependent is adaptability. Instruments of family support are questionnaires of
Friedman and adaptation skills using questionnaires from Nursalam. Data were analyzed using Spearmen rho
test with result ρ 0.005. The result of the study shoe that most families provide good support, and the
adaptability of patients with hallucinations is largely adaptive. Based on correlation results obtained r = 0,807,
which means good family suppotr associated with adaptive ability of adaptation patiens. The implications of
this study indicate that family support has an effect on the adaptability of post-treatment hallucination patients,
so families need to provide good family support to enable patients to adapt adaptively.
1 INTRODUCTION
Mental disorder according to PPGDJ III is a
syndrome of a person's behavioral pattern typically
associated with a symptom of distress or impairment
in one or more important functions of human beings,
psychological, behavioral, biological, and disorder
functions not only lies in the relationship between the
person but also with society (Maramis, 2010).
Schizophrenia is a disease that affects the brain and
causes strange and disturbed thoughts, perceptions,
emotions, movements, and behaviors (Videbeck,
2010). This schizophrenia shows both negative and
positive symptoms. Positive symptoms or real
symptoms that include delusions, hallucinations,
disorganization of the mind, disorderly speech and
irregular behavior (Videbeck, 2008). Based on these
positive symptoms that drew considerable attention to
the problem of mental nursing is a matter of
hallucinations.
Signs and symptoms of hallucinations are often
shown, among others, by the change in behavior as
often laugh alone, hear something and speak for
themselves.sensory function. Other changes that
occur are a decrease in problem-solving ability,
orientation to time, place, and people, anxiety, and
changes in Hallmarks and hallucinations must be an
abnormal condition of a person who will be
considered an oddity of others in relation to society
and conditions in the family, such as sadding a head
in a certain direction, talking and laughing, and
pacing (Suwardiman, 2013)
The family is the main support system that
plays a role in providing direct care to every healthy
and ill situation of schizophrenic patients. Generally
families request the help of health workers if they are
unable to care for it (Keliat, 2002).
According to WHO (2007), estimates there are
about 450 million people in the world who have
mental health problems, at least 1 (one) out of 4 (four)
people in the world experiencing mental problems.
One of the most common mental disorders is
schizophrenia, which ranks 4th out of 10 major
diseases around the world, regarding this, reports that
25,000,000 people worldwide are experiencing
schizophrenia (Stuart, 2007). Indonesia based on
mental health data PUSLITBANG Depkes RI
(2007), as much as 0.46% of Indonesian people
suffering from schizophrenia and experiencing severe
psychotic disorders. While the prevalence of severe
626
Nurlela, L., Harfika, M. and Novitasari, L.
Family Support Relationships with Patient Adaptation Ability above with Diagnosis Hallucination of Post Care.
DOI: 10.5220/0008329906260630
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 626-630
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

mental disorders, such as schizophrenia is 1.7% or
400,000 people (Depkes, 2014). Our preliminary
study at Mental Hospital Menur Surabaya, on January
17, 2017 in Ithe last three months, there are 5,816
people who are registered as outpatient patients, and
237 people who are inpatient at Menur Mental
Hospital. While patients with hallucinatory nursing
diagnosis there are 98 people who do hospitalization.
Previous studies have found that 70% of the ten
families of patients do self-care patients sincerely,
usher patients treated, supervise patients taking
medication and invite patients to activity. It shows
that family support that includes emotional,
informational, instrumental and research support is
done by the client's family in following the
therapeutic regimen (Friedman, in Suwardiman
2013).
Hospital-based care is excluded from planning for
nursing action. Therefore, families are included in the
preparation to go home. The purpose of home
planning is not only aimed at patients so that family-
focused nursing care not only restores the patient's
condition but aims to develop and improve the
family's ability to cope with family health problems
(Keliat In Wahyuningrum, 2013)
Home services reinforce and enhance the services
provided by family members and relatives also
maintain the independence and dignity of quality
clients that are often lost even from the best
institutions (Videbeck, 2010). The family is the unit
closest to the patient, and is the "primary nurse" for
the patient. The family plays a role in determining the
care necessary for the patient at home. The success of
nurses in the hospital will be in vain if it is not
continued at home which then leads the patient to be
treated again (relapse). Participation will increase the
ability of the family from the beginning of home care,
so the possibility of relapse can be prevented
(Wahyuningrum, 2013).
Family social support can weaken the impact of
stress and directly strengthen the mental health of
individuals and families. Social support is an
important coping strategy for a family experiencing
stress. Family social support can also serve as a
preventive strategy to reduce stress and its negative
consequences. A person with schizophrenia with the
inability to perform a social function surely needs
support to become a stronger individual and self-
respecting, so as to achieve better healing and
improve social functioning. Without the support of
the patient's family will be difficult to recover,
experiencing worsening and difficult to adapt in the
community environment.
Family interventions need to be structured and
coordinated in a comprehensive care model to be
more effective in helping patients adapt. Based on the
phenomenon, the authors want to know whether there
is a relationship of family support on the ability of
adaptation in patients hallucinations post-care Mental
Hospital Menur Surabaya.
2 METHODS
This research design is Non-Experimental
(correlation analytic research) which aims to reveal
correlation relationship between family support with
adaptation ability, with cross sectional approach, that
is as a research to study correlation dynamics between
risk factors with effects that emphasize time
measurement/ observation family support data with
adaptability only one time at a time without any
follow-up.
The population in this study were: outpatients
with post-treatment hallucinogenic diagnosis of RSJ
Menur Surabaya for 15 people and family of patients
living in Surabaya area of 15 people.
The samples in this study were some outpatients
with post-hospitalized hallucinatory diagnoses. For
independent variables are family support and
variables depedent is the ability of adaptation. Data
collection with questionnaire filling and analyzed
using SPSS Rank Spearman statistical test at
significance level <0,05.
In conducting the research, the researcher
submits a research request to the Education
Installation and is followed up with a research permit
application from the education side to the Mental
Hospital Menur Surabaya.
3 RESULTS
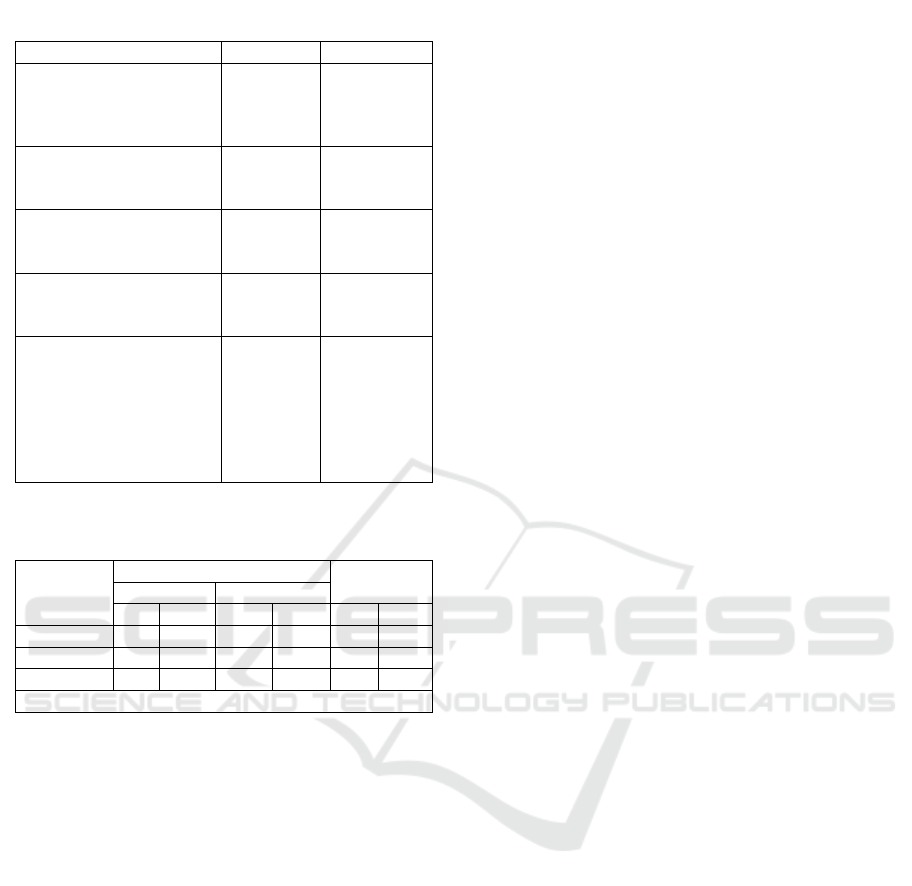
The distribution of family characteristics including
age, sex, recent education, occupation, outpatient
relationships with hallucinatory diagnoses in Poli
Jiwa Mental Hospital Menur Surabaya are shown on
table 1.
From the tabulation results show that the relation
of family support with the ability of adaptation of
outpatient with hallucinatory diagnosis in psychiatric
Mental Hospital Menur and obtained data that from
10 respondents who were given good family support
and have adaptive adaptation capability of 6 people
(100%), which provided good family support and
adaptive adaptive adaptability of 1 person (25%),
Family Support Relationships with Patient Adaptation Ability above with Diagnosis Hallucination of Post Care
627
which provided good family support and had
maladaptive adaptability of 3 people (75%). Based on
rho spearmen test result obtained p = 0,005 where H1
accepted if p <0,05 mean there is relation of family
support with ability of adaptation patient
hallucination.
4 DISCUSSION
Family support is a process that occurs over a lifetime
with varying nature and type of support (Friedman,
2010). Among them are emotional support,
information support, instrumental support and
assessment support. Such support forms a single
family support unit, especially for family members
who have health problems such as hallucinations.
Family support has a value of each (60%) for good
support, and (40%) for moderate support. This is
supported by Friedman's (2010) research, that family
support is very important to meet the psychosocial
needs of family members such as, caring for each
other, love, warmth and mutual support among family
members (Friedman, 2010). Researchers assume,
family support is very useful for hallucination
patients, especially affective function as an internal
function of the family
The results showed (60%) of the family provided
good emotional support. According to Friedman
(2010), it can be explained that emotional support as
the primary family coping goal to meet an adaptation.
Researchers assume that, emotional support can be
realized in the form of affection, trust, attention,
listening and listening. So this emotional support that
encourages an atmosphere of feeling achieves
compliance in the adaptability of the hallucinatory
patient. Emotional support is also needed to
strengthen the family in order to avoid the
psychosocial impact due to family members who
have hallucinations.
The results showed (60%) of the family provided
good information support. According to Friedman
(2010), the form of information support provided by
the family is to provide advice or advice, advice or
directions and provide important information that is
needed by the patient hallucinations in improving
health status. Researchers assume that, the support of
information provided to the family hallucinations of
patients is one form of family health care function in
maintaining the state of health of family members in
order to maintain high productivity. Thus, it is
important that information relief efforts for
hallucinations patients to improve the spirit and
motivation of patients hallucinations in order to
improve their adaptability optimally.
The results showed (60%) of the families
provided good instrumental support. According to
Friedman (2010), the objective family burden
includes the family burden in the conduct of caring
for one family member experiencing hallucinations,
including in this objective family burden the financial
cost, for care and treatment, shelter, food and
transportation. The instrumental support of the family
is a function of the economy and the function of
health care that the family applies to sick family
members. The researcher assumed that, paying
attention to regularly escorting the patient to a mental
health facility, consulting the progress of patient care
and maintaining medication adherence and providing
activity to the hallucinator. This should be done even
if the burden of families to access mental health is
very difficult, especially related to family finances..
The results showed (60%) of the families
provided good assessment support. According to
Friedman (2010) family assessment support is a form
of affective function of the family against
hallucinating patients who can improve the health
Table 1: Distribution of family characteristics.
Category Frequency Percentage
Age
a. 15 – 35 years
b. 36 – 55 years
C. 56
–
75
y
ears
2
5
3
20%
50%
30%
Gender
a. Male
b
. Female
4
6
20%
80%
Last education
a. Junior
b
. Senio
r
2
8
20%
80%
Employment
a. Work
b
. Does not wor
k
7
3
70%
30%
Relationship with
patients
a. mother
b. Husband
c. Brother
d. Brotherk
e. Children
4
1
1
2
1
40%
10%
20%
10%
10%
Table 2: The Correlation between family support with
adaptability of patients with hallucination.
Family
Support
Ada
p
tabilit
y
Total
Ada
p
tive Malada
p
tive
f % f % f %
Goo
d
6 100 0 0 6 100
Mediu
m
1 25 3 75 4 100
Total 7 70 3 30 10 100
S
p
erman Rho Test
p
=0.005
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
628

status of patients hallucinations. Through the support
of this assessment, patient hallucinations will gain
recognition of their ability as small and simple as
anything. Researchers assume that the patient's ability
to observe activities from the family as a form of
direct assessment support will increase self-esteem
and patient recognition in the eyes of the family and
the environment. Thus, the adaptability of patients
with hallucinations will gradually improve with
improved assessment support.
Adaptability has a value of each (70%) for
adaptive adaptability, and (30%) are maladaptive.
This is supported by Ambari's research (2010), there
are several factors that can affect the ability of
individual adaptation, namely the existence of social,
spiritual, assessment, and psychological needs.
Researchers assume that maladaptive adaptability is
affected by a lack of basic needs to adapt, such as lack
of family support, and unfulfilled desires.
Adaptation research results show (70%) of
adaptive social responses. This is in accordance with
research Ambari (2010), which states that high
adaptability is greatly influenced by social response.
Researchers assume that, social response can describe
the individual can interact with the environment well,
so the environment can provide an assessment of the
individual, whether adaptive adaptive or maladaptive.
Adaptation study results show (70%) of adaptive
psychological responses. This is in accordance with
the research Ambari (2010), adaptability depends on
the level of stress a person. Researchers assume that,
the adaptability of patients hallucinations tend to
change, because the level of stress experienced by
patients hallucinations tend to change.
Adaptation study results show (70%) assessment
responses in adaptive family support. In accordance
with Ambari's (2010) study, it shows that, patients
with hallucinations are not easy to remember the
stigma of society against "madmen" who consider as
individuals with strange behavior and difficult to
recover and experience social isolation, thus making
patients feel inferior and avoid social contact.
Researchers assume that, the patient's assessment
response is very important to be heard by the family.
so that families are able to provide better support and
patients can reinteract with their environment
Adaptation research results show (70%) spiritual
response in adaptive family support. In accordance
with the research of Ambari (2010), that patient
hallucinations can surrender to God for what trials are
given. Researchers assume that, hallucinations who
have adaptive spiritual responses, are able to accept
circumstances and submit to God
Performed statistical test of spearmen rho
obtained result 蟻 = 0,005 <伪 = 0,05, with value r =
0,802 which belong to perfect category (0,8 - 1) so it
can be concluded that H1 accepted, and H0 rejected.
The results showed that, hallucinations patients were
given good family support and had adaptive
adaptability of 6 people (60%). According to
Friedman (2010), the result of providing good family
support can make the hallucination patient has
adaptive adaptability. This shows the functioning of
the family of the hallucination patient, especially the
affective function as the internal function of the
family to meet the psychosocial needs of family
members such as caring for each other's love of
warmth and mutual support among family members.
Researchers assume that the family is the most
comfortable person for the hallucination patients. The
family can boost the spirit and motivation to behave
adaptively by providing good family support. As well
as providing appropriate care and treatment facilities.
Family support is the attitude, action, and acceptance
of the family to members of the family experiencing
hallucinations with varying nature and type of
support, including emotional support, information
support, instrumental support and assessment
support. Such support forms a single family support
unit, especially for family members who have health
problems such as hallucinatory problems with the
involvement of family support.
Good family support has a significant effect on the
rate of adaptation of hallucinatory patients (85.7%).
The results are supported by Friedman's (2010) study,
which shows the functioning of the patient's family in
the sub-province, especially the affective function as
the internal function of the family to meet the
psychosocial needs of family members such as caring
for each other, love, love, warmth and mutual support
among family members.
5 CONCLUSIONS
Most families of hallucinations give good family
support that provided in the form of emotional
support, information, instrumental and assessment.
Most post-treatment hallucinations have adaptive
adaptability in social, psychological, judgmental, and
spiritual responses. Good family support is highly
correlated with adaptive post-treatment adaptive
adaptability..
Family Support Relationships with Patient Adaptation Ability above with Diagnosis Hallucination of Post Care
629

REFERENCES
Andarmoyo, Sulistyo. (2012). Keperawatan Keluarga;
Konsep Teori, Proses dan Praktik Keperawatan.
Yogyakarta : Graha Ilmu.
Ambarsari, R.D., & Sari, E.P. (2012). Penyesuaian diri
caregives orang dengan skizofrenia (ODS). Jurnal
Psikologika, 17(2).
Ambari, P.K.M. (2010). Skripsi Hubungan antara
dukungan keluarga dengan keberfungsian sosial pada
pasien skizofrenia pasca perawatan di rumah sakit.
Bandung: UNDIP
Damaiyanti, Mukhripah & Iskandar. (2012). Asuhan
Keperawatan Jiwa. Bandung. Refika Aditama.
Dermawan, Deden & Rusdi. (2013). Keperawatan Jiwa;
Konsep dan Kerangka Kerja Asuhan Keperawatan
Jiwa. Yogyakarta : Gosyen Publishing
Davies, Teifion & Craig, TKJ (editor). (2009). ABC
Kesehatan Mental. Jakarta : EGC.
Fahanani, Fitrianan Gebyar. (2010). Hubungan
pengetahuan tentang gangguan jiea dengan dukungan
keluarga yang mempunyai anggota keluarga
Skizofrenia di RSJD Surakarta. Suarakarta. Skripsi
tidak dipublikasikan.
Friedman, Marilyn M. (2010). Buku Ajar Keperawatan
Keluarga: Riset, Teori, dan Praktek. Jakarta : EGC
Hamid, Achir Yani S, dan Ibrahin, Kusman (Editor).
(2014). Pakar Teori Keperawatan dan Karya Mereka.
Jakarta : Elsevier.
Hawari, D. (2012). Skizofrenia pendekatan holistik BPSS.
Jakarta: FKUI
Hidayato, W.C. (2013). Pengauh terapi religious zikir
terhadap peningkatan kemampuan mengkontrol
halusinasi pendengaran pada pasien halusinasi di RSJD
Dr. Amini Gondhoutomo Semarang. Diunduh pada
tanggal 18 mei 2017 pukul 12.06 WIB.
Ibrahim, H Ayub Sani. (2011). Skizofrenia; Spliting
Personality. Tangerang : Jelajah Nusantara.
Jaya, Kusnadi. (2015). Keperawatan Jiwa. Tangerang :
Binarupa Aksara.
Keliat, Budi Anna. 2016. Prinsip dan Praktik Keperawatan
Kesehatan Jiwa. Stuart; Edisi Indonesia. Jakarta.
Elsevier.
Keliat, Budi Anna., dan Pasaribu, Jesika (Editor). (2016).
Prinsip dan Praktik Keperawatan Kesehatan Jiwa
Stuart. Jakarta : Elsevier.
Kusumawati, Farida & Hartono, Yudi. (2012). Buku Ajar
Keperwatan Jiwa. Jakarta : Salemba Medika.
Mubarak, Wahid Iqbal & Chayatin, Nurul. (2009). Ilmu
Kesehatan Masyarakat Teori dan Aplikasi. Jakarta :
Salemba Medika.
Nasir, Abdul & Muhith, Abdul. (2011). Dasar-dasar
Keperawatan Jiwa Pengantar dan Teori. Jakarta :
Salemba Medika.
Nursalam. (2011). Konsep dan Penerapan Metodologi
Penelitian Ilmu Keperawatan; pedoman skripsi, tesis,
dan instrumen penelitian keperawatan. Jakarta :
Salemba Medika.
Potter, Patricia A & Perry, Anne G. (2009). Fundamental
Keperawatan Edisi 7. Jakarta : Salemba Medika.
Prabowo, Hendy P. (2007). Interaksi Keluarga pada Remaja
Penderita Skizofrenia; Tinjauan Psikokultural Jawa.
Semarang. Skripsi tidak dipublikasikan.
Prasetyo. (2016). Hubungan Faktor Demografi Dengan
Kualitas Hidup Pasien Skizofrenia. Diunduh pada
tanggal 18 mei 2017 Pukul 12.07 WIB.
Stuart, G.W. (2016). Principles and practice of psychiatric
Nurshing. (10 th Ed). Elsevier : Mosby.
Suwardiman, Deni. (2011). Hubungan Antara Dukungan
Keluarga Dengan Beban Keluarga Untuk Mengikuti
Regimen Terapeutik Pada Keluarga Klien Halusinasi
Di RSUD Serang. Depok : Tesis Publikasi.
Ulpa, Delia. (2013). Dukungan Dengan beban Keluaraga
mengikuti regimen terapeutik anggota keluarga yang
mengalami halusinasi. Diunduh pada tanggal 18 mei
2107 pukul 00.06 WIB
Ullatifah, Wahid A. (2015). Hubungan Dukungan
Psikososial Keluarga Dengan Lama Rawat Inap Pasien
Skizofrenia Di Rumah Sakit Jiwa Daerah Surakarta.
Surakarta. Diunduh pada tanggal 14 desember 2016
Pukul 14.48 WIB.
Videbeck, Sheila L. (2008). Buku Ajar Keperawatan Jiwa.
Jakarta : EGC.
Videbeck, Sheila L. (2010). Buku Ajar Keperawatan Jiwa.
Jakarta : EGC
Wahyuningrum, Irma. Hubungan Dukungan Keluarga
Dengan Durasi Kekambuhan Pasien Skizofrenia Di
Rumah Sakit Jiwa Daerah Dr. Amino Gondhoutomo
Semarang. Semarang. Skripsi tidak dipublikasikan
Yusuf, AH et all. 2015. Buku Ajar Keperawatan Kesehatan
Jiwa. Jakarta : Salemba Medika.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
630
