
Is an Educational Level Affect Women’s Participation on Cervical
Cancer Screening?
A Systematic Review
Rafika Rosyda
1
, Budi Santoso
2
, Esti Yunitasari
1
1
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
2
Faculty of Medicine, Universitas Airlangga, Surabaya
Keyword: Cervical cancer, Cervical cancer prevention, Screening, Early detection, Education.
Abstract: Cervical cancer became fourth most common cancer case among women in the world. There were
approximately 528.000 new cases in 2012. Screening is the most proven method to prevent cervical cancer.
Level of education seems to be an important predictor of cancer screening participation. Nowadays, there is
a little strong evidence of this specific association. Therefore, a systematic review is necessary. This review
was guided by PICO framework to identified appropriate resources for relevant study. Search of the studies
were carried out by Pro-Quest and Medline, with keywords: “cervical cancer screening”, “Pap smear”,
“VIA” “screening program”, “socioeconomic factors”, “educational level” and “screening participation”.
From 904 studies found, 13 included for review. 11 of 13 (84,6%) reported that level of education were
positively associated with women’s participation on cervical cancer screening, and only 2 studies reported
that there is no association. This review conclude that women with higher educational level are more likely
to participate cervical cancer screening.
1 BACKGROUND
Cervical cancer became fourth most common cancer
among women and seventh in all cancer all over the
world. There were approximately 528.000 new cases
in 2012. In Western counties, cervical cancer
prevention effort was done by increasing HPV
vaccination (Cullen, Stokley, & Markowitz, 2014).
However, screening is the most proven method for
reducing rates of cervical cancer (de Blasio, Neilson,
Klemp, & Skjeldestad, 2012). There were some
evidences that Pap Smear, and VIA are associated
with decreasing mortality of cervical cancer
(Meggiolaro et al., 2016; Sankaranarayanan et al.,
2007).
There are some recommendations for cervical
cancer screening (Schwaiger, Aruda, LaCoursiere,
Lynch, & Rubin, 2013). In general, cervical
screening interval may once in 3 to 5 years
(Schwaiger et al., 2013). Screening policy could
affect screening participation. Other than that, there
are more various factors as well as the characteristic
of health system, sociocultural factors,
environmental factors, invitation method, and
individual factors such as age, occupation, and
education. Notably, level of education is one of
health determinant that could be an important
predictor of cancer screening participation (Damiani
et al., 2012).
Although there were a lot of studies had found
positive relationship between level of education and
participation on cervical cancer screening, some of
the results did not find statistically significant.
Nowadays, the strong evidence for this relationship
is still low. Therefore, this systematic review is
necessary. This systematic review assessed the
impact of educational level on women’s
participation on cervical cancer screening.
2 METHODS
The PICO framework was used to guide this
systematic review, with P: sexually active women,
with no symptom and history of female cancers, I:
higher level of education, C: lower level of
education, O: have ever done cervical cancer
screening in their lifetime.
482
Rosyda, R., Santoso, B. and Yunitasari, E.
Is an Educational Level Affect Women’s Participation on Cervical Cancer Screening?.
DOI: 10.5220/0008327204820488
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 482-488
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2.1 Search Strategy
Search of the studies were carried out by ProQuest
and Medline, with keywords: “cervical cancer
screening”, “Pap smear”, “VIA” “screening
program”, “socioeconomic factors”, “educational
level” and “screening participation”.
2.2 Assessment of the Studies
2.2.1 Eligibility
The inclusion criteria for this review:
- Studies published between 2008 – 2018,
- Articles published in English,
- The result section reported the relationship
between level of education and cervical cancer
screening participation.
The exclusion criteria for this review:
- Participants were women with history or family
history of cervical cancer,
- Participants with other disease (e.g. diabetes).
Methodological Quality:
The quality assessment consisted:
- The design of the study,
- Data collection,
- Selected bias,
- Statistical analysis conformity.
Quality assessment was done by rating each item
above as “strong”, “moderate”, or “weak”. As
consequence, the study would be “high quality” if
three of them were strong, with no weak. If there
was only one weak, study would be “moderate
quality”, and if there were more than one item rated
weak, the study would be “low quality”.
2.2.2 Data Extraction
These following items were collected from each
study:
- Author, years of publication
- Design of the study
- Population size and targeted age
- Outcome
- Educational level
- Relationship between educational level and
screening participation
3 RESULTS
3.1 Included Studies
Twelve from Thirteen studies are cross sectional,
and one is case control. Studies selected for this
review obtained by the Swedish National Cervical
Screening Registry (Broberg et al., 2018),
Morehouse School of Medicine (Miles-Richardson,
Allen, Claridy, Booker, & Gerbi, 2017), The
KNHNES (Chang et al., 2017; Lee et al., 2013),
WHO’s Study on Global Ageing and Adult Health
(Akinyemiju, Ogunsina, Sakhuja, Ogbhodo, &
Braithwaite, 2016), GPMSSP (Gyulai et al., 2015),
University of Pittsburgh (Alfaro et al., 2015),
Karolinska Institutet (Östensson et al., 2015), New
Americans Community Services, and University of
Minnesota (Harcourt et al., 2014), European Health
Interview Survey for Spain (Martín-López et al.,
2012), ISTAT (Damiani et al., 2012), BRFSS and
ARF (Coughlin, Leadbetter, Richards, & Sabatino,
2008), and the JCUSH (Blackwell, Martinez, &
Gentleman, 2008).
Two studies were conducted in Sweden (Broberg
et al., 2018; Östensson et al., 2015), four studies in
US (Blackwell et al., 2008; Coughlin et al., 2008;
Harcourt et al., 2014; Miles-Richardson et al., 2017),
two studies in Korea (Chang et al., 2017; Lee et al.,
2013), and the other respectively in Canada
(Blackwell et al., 2008), El Salvador (Alfaro et al.,
2015), Spain (Martín-López et al., 2012), Italy
(Damiani et al., 2012), Hungary (Gyulai et al.,
2015). Twenty two different populations were
identified. Specifically, 10 studies analyzed one
population, and 3 studies analyzed more.
3.2 Quality Assessment
Based on the design of the study, twelve studies
rated “weak” due to cross sectional, and one study
rated “moderate” due to case control. Based on their
data collection, all studies rated “moderate” because
obtained by surveys. Based on selection bias, ten
studies rated “strong” (Akinyemiju et al., 2016;
Blackwell et al., 2008; Broberg et al., 2018; Chang
et al., 2017; Coughlin et al., 2008; Damiani et al.,
2012; Gyulai et al., 2015; Lee et al., 2013; Martín-
López et al., 2012; Miles-Richardson et al., 2017)
because conducted nationwide and enrolled
representative sample. Then, based on statistical
analysis conformity, all studies rated “strong”.
Overall, all studies are in moderate quality.
Is an Educational Level Affect Women’s Participation on Cervical Cancer Screening?
483
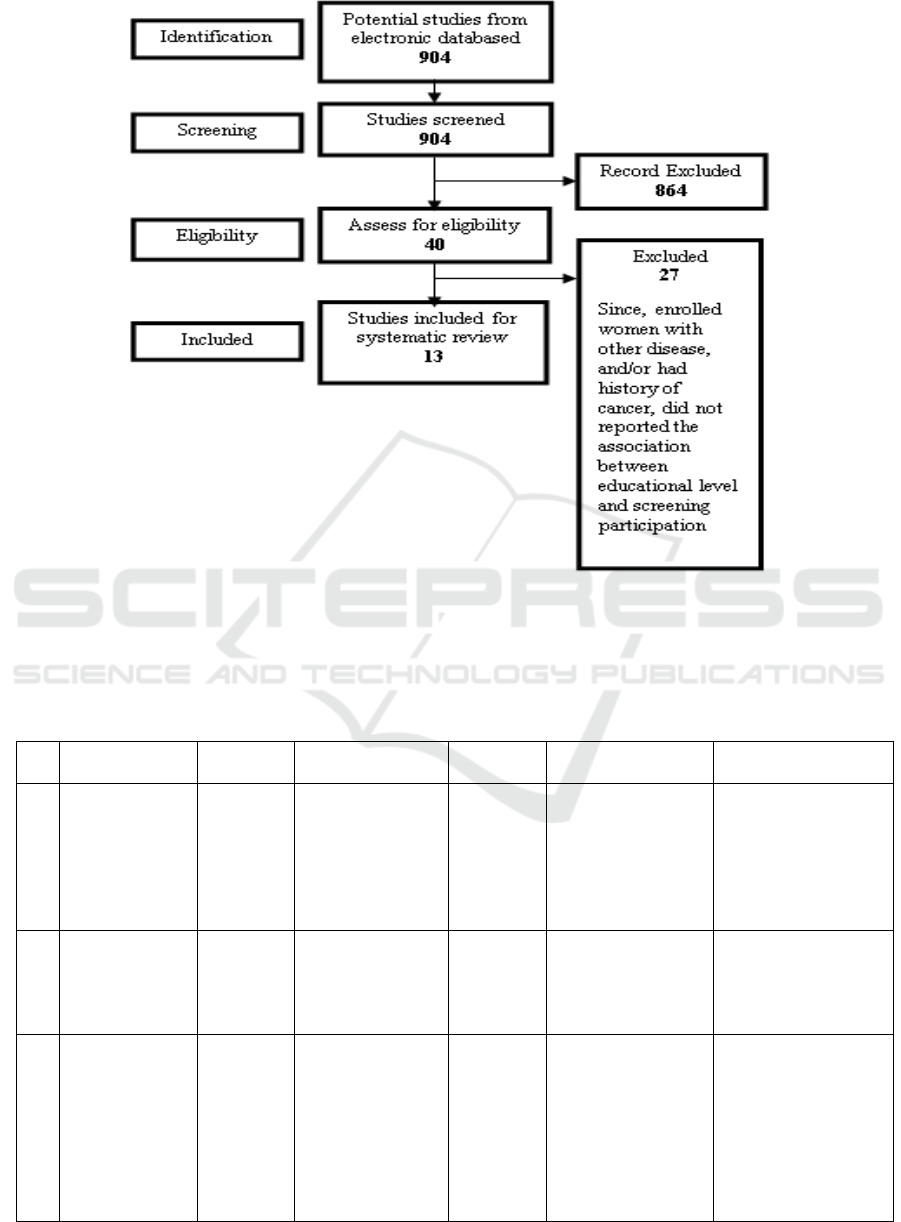
Figure 1: Review method.
3.3 Study Characteristic
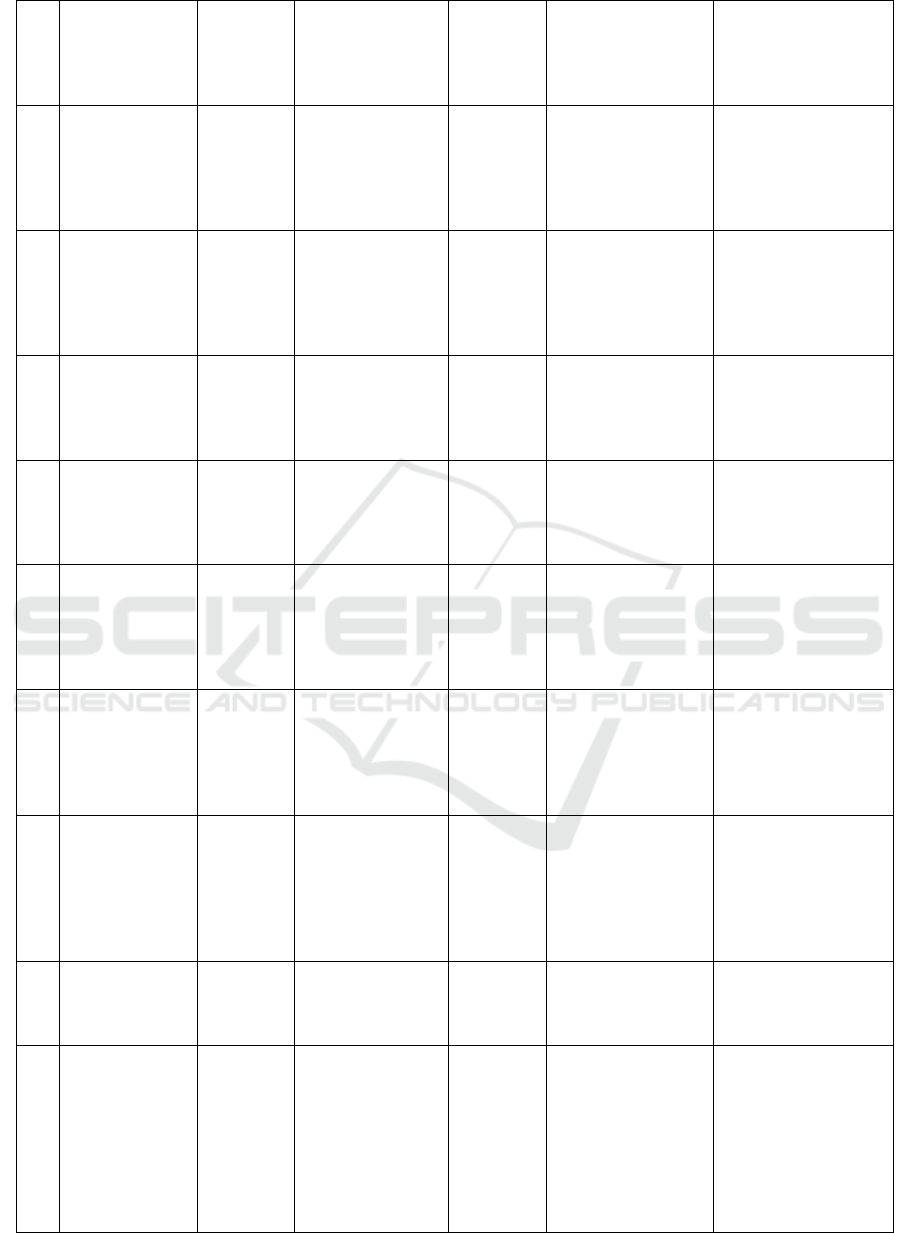
Table 1: Study Characteristic.
N
o
Author, Year of
Publication
Design
Populations,
Targeted Age
Outcome
Educational Level
Relationship
1
(Broberg et al.,
2018)
Case
control
1
Sweden;
Case; n=314.302
Control;
n=266.706
30-60 years old
Attended
pap smear
test
1. ≤ 9 years
2. 10-12 years
3. > 12 years
Women with lower
education were more
likely to not attend
cervical screening
2
(Chang et al.,
2017)
Cross
sectional
1
Korea; n=3.734
15-39 years old
Had pap
smear test
1. < 6 years
2. 6-9 years
3. 10-12 years
4. >12 years
Higher educational
levels associated with
participation in
cervical cancer
screening
3
(Akinyemiju et
al., 2016)
Cross
sectional
5
China; n=8.002
India; n=7.489
Mexico; 1.689
Russia; n=2.676
South Africa;
n=2.427
21-65 years old
Had pap
smear test
1. No formal
education
2. Primary
3. Secondary
4. University/
college
education,
significantly
increased cervical
cancer screening
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
484
4
(Alfaro et al.,
2015)
Cross
sectional
1
El Salvador;
n=409
30-49 years old
Had
cervical
cancer
screening
1. < Elementary
2. Middle school
3. > High school
There was no
association
between screening
participation and
educational level
5
(Östensson et
al., 2015)
Cross
sectional
1
Sweden; n=1.510
23-60 years old
Attended
cervical
cancer
screening
1. < High-school
2. High-school or
equal
3. > High-school
Educational levels
positively associated
with cervical cancer
screening
participation
6
(Harcourt et al.,
2014)
Cross
sectional
1
USA; n=421
≥ 18 years old
Had
cervical
cancer
screening
1. ≤ High school
2. > High school
There was no
association between
educational level and
cervical cancer
screening
participation
7
(Martín-López
et al., 2012)
Cross
sectional
1
Spain; n=7.634
25-64 years old
Had Pap
smear test
1. Primary
2. Secondary
3. University
Undergoing cervical
cancer screening
positively associated
with higher
educational levels
8
(Damiani et al.,
2012)
Cross
sectional
1
Italy; n=35.349
25-64 years old
Had 1 pap
smear test
1. < Primary
2. Secondary
3. > high-school
Education level were
positively associated
with attendance to
cervical cancer
screening
9
(Coughlin et
al., 2008)
Cross
sectional
1
USA; n=97.820
≥18 years old
Had Pap
smear test
1. < high-school
2. High-school
graduate/ GED
3. Some college/
technical school
4. College graduate
higher educational
levels related to
having cervical
cancer screening
10
(Blackwell et
al., 2008)
Cross
sectional
2
Canada; n=1.895
US; n=2.959
18-69 years old
Had Pap
smear test
1. < High-school
2. High-school
Diploma/ GED
3. Vocational
certificate
4. University
Educational levels
predict compliance
with cervical cancer
screening in Canada
(and nearly
did in the US)
11
(Gyulai et al.,
2015)
Cross
sectional
1
Hungary; n=
1539
25-65 years old
Had pap
smear test
1. Primary
2. Some Secondary
3. Secondary
4. Post-secondary
without diploma
5. College /
university
higher education
increases
participation
12
(Miles-
Richardson et
al., 2017)
Cross
sectional
1
USA; n=272.692
≥ 18 years old
Had pap
smear test
1. ≤ high school
2. Some college
3. College graduate
women with higher
level of education
were more likely to
be screened
13
(Lee et al.,
2013)
Cross
sectional
5
Korea; N=17.105
[1998]; n=2725
[2001]; n=1622
[2005]; n=2596
[2008]; n=2944
[2010]; n=2737
≥30 years old
Participat
ed
cervical
cancer
screening
1. ≤ elementary
2. Middle – high
school
3. ≥ university
Educational levels
influenced screening
participation. lower
educational levels
were less likely to be
screened
Is an Educational Level Affect Women’s Participation on Cervical Cancer Screening?
485

4 DISCUSSION
This review found that 84,6% studies reported that
women with higher level of education are more
likely to participate cervical cancer screening
compare with women with lower level of education.
Overall, this review confirms that the risk of
participating cervical cancer screening is affected by
education.
Similar review found that there was positive
association between educational level and some
health-related behavior, one of them is screening
participation (Cutler & Lleras-Muney, 2010). The
reason is Well-educated women may have better
interest, and better access to resources and
information, so they have better knowledge about
health issue and behavior to improve their health.
Also, they have greater awareness of risks (Adams,
2010; Hahn & Truman, 2015). Simply, sufficiency
of current knowledge has a positive influence on
health-promoting behavioral options.
The argument of this finding is health literacy
has positive association with level of education.
Health literacy is an individual capacity to get,
process, and figure out the necessary information
and basic health service to determine health-related
decisions. One of the important factor that can
determine health literacy is level of education.
People with higher educational level were found to
demonstrated higher health literacy skill. (van der
Heide et al., 2013). Well-educated people are more
likely to completely understand the information and
instructions. Furthermore, people with higher level
of health literacy can increase the likelihood of
communication to health care providers that can lead
to better outcomes. Simply, low health literacy skill
can be a barrier in access health information, health
service, and disease prevention.
People with high capacity of health literacy also
have a higher capacity to be informed that screening
is necessary to prevent cervical cancer. This means
that the association between educational level and
some health behaviors – in this case cervical cancer
screening participation – is affected by health
literacy skill.
Cervical cancer screening participation is also
affected by the type of health care system and its
accessibility, screening policy, environmental,
sociocultural, and factors at individual level such as
age, race, insurance coverage and occupation
(Blackwell et al., 2008; Coughlin et al., 2008;
Damiani et al., 2012). In addition, cultural factors
can predict cervical cancer screening participation
and may be related with educational level. Some
studies reported that low cervical cancer screening
participation was caused by low knowledge about
screening guideline, along with various cultural
factors, such as negative attitudes toward illness and
misunderstanding about risk factors and screening
practices (Cadet, Burke, Stewart, Howard, &
Schonberg, 2017; Luque et al., 2015; Madhivanan,
Valderrama, Krupp, & Ibanez, 2016). Furthermore,
there is a correlation between cervical cancer
screening and some of the health-related behaviors,
including unhealthy diet, obesity, lack of physical
activity, and tobacco and alcohol consumption
(Damiani et al., 2012; Martín-López et al., 2012).
All factors above should be considered as they
may lead to be confounders in the evaluation of the
role of education level on cervical cancer screening
participation. Nevertheless, all included studies
conformed their analysis to those possible
confounding factors.
5 CONCLUSIONS
Women with higher educational level have a higher
risk to participate cervical cancer screening. This
finding can be considered in decision-making
processes to reduce the inequalities and increase
women’s participation on cervical cancer screening.
Overall, this review confirms that more educated
women are more likely to have cervical cancer
screening.
REFERENCES
Adams, R. J. (2010). Improving health outcomes with
better patient understanding and education. Risk
Management and Healthcare Policy, 3(3), 61–72.
https://doi.org/10.2147/RMHP.S7500
Akinyemiju, T., Ogunsina, K., Sakhuja, S., Ogbhodo, V.,
& Braithwaite, D. (2016). Life-course socioeconomic
status and breast and cervical cancer screening:
analysis of the WHO’s Study on Global Ageing and
Adult Health (SAGE). BMJ Open, 6(11), e012753.
https://doi.org/10.1136/bmjopen-2016-012753
Alfaro, K. M., Gage, J. C., Rosenbaum, A. J., Ditzian, L.
R., Maza, M., Scarinci, I. C., … Cremer, M. L. (2015).
Factors affecting attendance to cervical cancer
screening among women in the Paracentral Region of
El Salvador: a nested study within the CAPE HPV
screening program. BMC Public Health, 15(1), 1058.
https://doi.org/10.1186/s12889-015-2360-7
Blackwell, D. L., Martinez, M. E., & Gentleman, J. F.
(2008). Women’s compliance with public health
guidelines for mammograms and pap tests in Canada
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
486

and the United States: an analysis of data from the
Joint Canada/United States Survey Of Health.
Women’s Health Issues : Official Publication of the
Jacobs Institute of Women’s Health, 18(2), 85–99.
https://doi.org/10.1016/j.whi.2007.10.006
Broberg, G., Wang, J., Östberg, A.-L., Adolfsson, A.,
Nemes, S., Sparén, P., & Strander, B. (2018). Socio-
economic and demographic determinants affecting
participation in the Swedish cervical screening
program: A population-based case-control study.
PLOS ONE, 13(1), e0190171.
https://doi.org/10.1371/journal.pone.0190171
Cadet, T. J., Burke, S. L., Stewart, K., Howard, T., &
Schonberg, M. (2017). Cultural and emotional
determinants of cervical cancer screening among older
Hispanic women. Health Care for Women
International, 38(12), 1289–1312.
https://doi.org/10.1080/07399332.2017.1364740
Chang, H. K., Myong, J.-P., Byun, S. W., Lee, S.-J., Lee,
Y. S., Lee, H.-N., … Park, T. C. (2017). Factors
associated with participation in cervical cancer
screening among young Koreans: a nationwide cross-
sectional study. BMJ Open, 7(4), e013868.
https://doi.org/10.1136/bmjopen-2016-013868
Coughlin, S. S., Leadbetter, S., Richards, T., & Sabatino,
S. A. (2008). Contextual analysis of breast and
cervical cancer screening and factors associated with
health care access among United States women, 2002.
Social Science & Medicine, 66(2), 260–275.
https://doi.org/10.1016/j.socscimed.2007.09.009
Cullen, K. A., Stokley, S., & Markowitz, L. E. (2014).
Uptake of Human Papillomavirus Vaccine Among
Adolescent Males and Females: Immunization
Information System Sentinel Sites, 2009–2012.
Academic Pediatrics, 14(5), 497–504.
https://doi.org/10.1016/j.acap.2014.03.005
Cutler, D. M., & Lleras-Muney, A. (2010). Understanding
differences in health behaviors by education. Journal
of Health Economics, 29(1), 1–28.
https://doi.org/10.1016/j.jhealeco.2009.10.003
Damiani, G., Federico, B., Basso, D., Ronconi, A.,
Bianchi, C. B. N. A., Anzellotti, G. M., … Ricciardi,
W. (2012). Socioeconomic disparities in the uptake of
breast and cervical cancer screening in Italy: a cross
sectional study. BMC Public Health, 12(1), 99.
https://doi.org/10.1186/1471-2458-12-99
de Blasio, B. F., Neilson, A. R., Klemp, M., &
Skjeldestad, F. E. (2012). Modeling the impact of
screening policy and screening compliance on
incidence and mortality of cervical cancer in the post-
HPV vaccination era. Journal of Public Health, 34(4),
539–547. https://doi.org/10.1093/pubmed/fds040
Gyulai, A., Nagy, A., Pataki, V., Tonté, D., Ádány, R., &
Vokó, Z. (2015). Survey of Participation in Organised
Cervical Cancer-Screening Programme in Hungary.
Central European Journal of Public Health, 23(4),
360–364. https://doi.org/10.21101/cejph.a4068
Hahn, R. A., & Truman, B. I. (2015). Education Improves
Public Health and Promotes Health Equity.
International Journal of Health Services, 45(4), 657–
678. https://doi.org/10.1177/0020731415585986
Harcourt, N., Ghebre, R. G., Whembolua, G.-L., Zhang,
Y., Warfa Osman, S., & Okuyemi, K. S. (2014).
Factors Associated with Breast and Cervical Cancer
Screening Behavior Among African Immigrant
Women in Minnesota. Journal of Immigrant and
Minority Health, 16(3), 450–456.
https://doi.org/10.1007/s10903-012-9766-4
Lee, M., Park, E.-C., Chang, H.-S., Kwon, J. A., Yoo, K.
B., & Kim, T. H. (2013). Socioeconomic disparity in
cervical cancer screening among Korean women:
1998–2010. BMC Public Health, 13(1), 553.
https://doi.org/10.1186/1471-2458-13-553
Luque, J. S., Tarasenko, Y. N., Maupin, J. N., Alfonso, M.
L., Watson, L. C., Reyes-Garcia, C., & Ferris, D. G.
(2015). Cultural Beliefs and Understandings of
Cervical Cancer Among Mexican Immigrant Women
in Southeast Georgia. Journal of Immigrant and
Minority Health, 17(3), 713–721.
https://doi.org/10.1007/s10903-014-0117-5
Madhivanan, P., Valderrama, D., Krupp, K., & Ibanez, G.
(2016). Family and cultural influences on cervical
cancer screening among immigrant Latinas in Miami-
Dade County, USA. Culture, Health & Sexuality,
18(6), 710–722.
https://doi.org/10.1080/13691058.2015.1116125
Martín-López, R., Hernández-Barrera, V., de Andres, A.
L., Carrasco-Garrido, P., de Miguel, A. G., &
Jimenez-Garcia, R. (2012). Trend in cervical cancer
screening in Spain (2003–2009) and predictors of
adherence. European Journal of Cancer Prevention,
21(1), 82–88.
https://doi.org/10.1097/CEJ.0b013e32834a7e46
Meggiolaro, A., Unim, B., Semyonov, L., Miccoli, S.,
Maffongelli, E., & La Torre, G. (2016). The role of
Pap test screening against cervical cancer: a systematic
review and meta-analysis. La Clinica Terapeutica,
167(4), 124–139.
https://doi.org/10.7417/CT.2016.1942
Miles-Richardson, S., Allen, S., Claridy, M. D., Booker,
E. A., & Gerbi, G. (2017). Factors Associated with
Self-Reported Cervical Cancer Screening Among
Women Aged 18 Years and Older in the United States.
Journal of Community Health, 42(1), 72–77.
https://doi.org/10.1007/s10900-016-0231-5
Östensson, E., Alder, S., Elfström, K. M., Sundström, K.,
Zethraeus, N., Arbyn, M., & Andersson, S. (2015).
Barriers to and Facilitators of Compliance with Clinic-
Based Cervical Cancer Screening: Population-Based
Cohort Study of Women Aged 23-60 Years. PLOS
ONE, 10(5), e0128270.
https://doi.org/10.1371/journal.pone.0128270
Sankaranarayanan, R., Esmy, P. O., Rajkumar, R.,
Muwonge, R., Swaminathan, R., Shanthakumari, S.,
… Cherian, J. (2007). Effect of visual screening on
cervical cancer incidence and mortality in Tamil
Nadu, India: a cluster-randomised trial. The Lancet,
370(9585), 398–406. https://doi.org/10.1016/S0140-
6736(07)61195-7
Schwaiger, C. B., Aruda, M. M., LaCoursiere, S., Lynch,
Is an Educational Level Affect Women’s Participation on Cervical Cancer Screening?
487

K. E., & Rubin, R. J. (2013). Increasing Adherence to
Cervical Cancer Screening Guidelines. The Journal
for Nurse Practitioners, 9(8), 528–535.
https://doi.org/10.1016/j.nurpra.2013.05.013
van der Heide, I., Wang, J., Droomers, M.,
Spreeuwenberg, P., Rademakers, J., & Uiters, E.
(2013). The Relationship Between Health, Education,
and Health Literacy: Results From the Dutch Adult
Literacy and Life Skills Survey. Journal of Health
Communication, 18(sup1), 172–184.
https://doi.org/10.1080/10810730.2013.825668
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
488
