
Lifestyle Education Based on Electronic Media for Diabetes
Management
A Systematic Review
Komang Agus Jerry Widyanata
1
, Kusnanto
2
and Suprajitno
3
1
Magister of Nursing Student, Universitas Airlangga, Surabaya, Indonesia
2
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
3
Nursing Department, Poltekkes Malang, Indonesia
Keywords : Electronic, Lifestyle Education, Self-Management, Type 2 Diabetes.
Abstract : The number of deaths due to diabetes mellitus is still high and tends to increase, this is due to the lack of self-
management of patients with diabetes mellitus. The purpose of this research is to identify education with
electronic media to improve self-management of diabetes mellitus type 2. This study was used systematic
review with a literature search using online reference databases: ProQuest, EBSCOhost, PubMed, Scopus,
and Science Direct. The determination of the keyword is based on PICOT framework (P: diabetes mellitus
type 2, I: internet, computer, telephone, electronics, telehealth, C: -, O: behavior, lifestyle, blood sugar
control, self-management, T: 2009-2018). Studies were included if they described interventions with
electronic media targeted at patients with type 2 diabetes, focused on behavioral, biomedical, and
psychological changes. The review of 15 papers that met the criteria showed significant results in the use of
electronic media to the level of knowledge, confidence, nutrition intake, physical activity, self-efficacy and
empowerment. Electronic media also significantly affects biomechanics especially for HbA1c results.
Electronic media can be one of the right choices in providing self-management education of type 2 diabetes
mellitus.
1 BACKGROUND
Currently Indonesia is ranked fifth world as a
country that has the largest number of diabetes
mellitus cases (PERKENI, 2015). The International
Diabetes Federation notes that by 2013 there are 382
million people in the world who suffer from diabetes
mellitus, of which there are 175 million undiagnosed
and threatened progressively unconscious
complications resulting from without precautions.
Data for the year is expected to increase to 592
million people who will suffer diabetes mellitus in
2035 (IDF, 2013)
In addition to the increasing number of cases,
diabetes mellituS is also known to cause many
complications that are divided into two, they are
acute complications and chronic complications.
Acute complications include hypoglycemia, diabetic
ketoacidosis, and non-ketotic hyperosmolar, and
chronic complications are macroangiopathy,
microangiopathy and neuropathy (PERKENI, 2015).
The number of cases and complication problems put
the case of diabetes mellitus in the third rank cause
of the highest non-infectious disease mortality in
Indonesia in 2016 (Departemen Kesehatan RI,
2014).
The main goal in the management of diabetes
mellitus is the achievement of near-normal
glycemic. by self management diabetes mellitus
such as diet, exercise, blood sugar control and
Diabetes mellitus treatment (Gb & Premkumar,
2016). Individuals with chronic diseases such as
diabetes, require innovative methods of health
education, individuals claim that they want
information in as many formats as possible and as
early as possible after diagnosis. (Booth et al.,
2016). Making their own decisions for improving
blood sugar levels and performing related self
chosen actions and maintaining its long term
performance is the key element in diabetes self care
management (Gb & Premkumar, 2016)
International Diabetic Federation (2013) states
that at the individual level of diabetes self-
220
Widyanata, K., Kusnanto, . and Suprajitno, .
Lifestyle Education Based on Electronic Media for Diabetes Management.
DOI: 10.5220/0008323002200228
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 220-228
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

management education that integrates clinical,
behavioral and psychosocial aspects of diabetes self-
management should be available and sustainable.
Effective self-management can improve the health
of diabetes and prevent or delay the onset of
complications, yet difficult and complex to achieve.
This can be realized by allowing patients to
understand their condition, combined with a barrier
resolution for compliance(Dale, Caramlau, Sturt,
Friede, & Walker, 2009).
The use of technology in the treatment of
diabetes can facilitate improved communication
between nurses and patients, reliable data collection,
and the provision of a comfortable life for patients.
An important goal of treatment with electronic
media is to give patients the opportunity to maintain
their education effectively without interruption
(Tavşanli, 2013). Telenursing methods are beginning
to demand as health services to support patients in
home care (Higano, 2015). Telenursing refers to the
use of telecommunications and information
technology in the provision of remote nursing care,
which can help solve patient problems, reduce
distance and travel time, and maintain the health
status of patients at home (Higano, 2015).
According Tavşanli (2013) in his research on the
application of telenursing in patients with type 2 DM
recommends that more research to study the impact
of technical innovation on improving disease
management and medical results and prevention of
diabetes complications with good glycemic control
Computer-based tools represent one such approach
that helps support diabetes education provided by
healthcare professionals. Telephone interventions
are very important. Interesting because they are
relatively cheap, easily accommodated around
individual schedules, and possibly improved health
literacy skills than print interventions (Chamany et
al., 2015).
There is some evidence that the use of
Computer-based education can increase knowledge,
motivation, and self-care behavior in diabetics.
Booth et al., (2016) In addition, several studies have
demonstrated the efficiency of indirect forms of
preventive interventions such as telephone, letters,
and consultations via the Internet, may be better
suited to provide preventive interventions, for high-
risk populations at low cost, and allow treatment to
involve more people compared with face-to-face
method (Tokunaga et al., 2014).
The main purpose of this review is to identify the
study used Intervention-based electronic media
education to promote diabetes education and
lifestyle modification of adults with type 2 diabetes.
2 METHODS
2.1 Design
The design of this study is a systematic review,
synthesis of findings from a study comparing the use
of electronic media as a medium of education with
usual care in patients with diabetes mellitus.
2.2 Search Strategy
The method used in this systematic review begins
with topic selection, then the keyword is determined
to search the journal through several databases such
as ProQuest, Ebsco, PubMed, and Science Direct.
The determination of the keyword is based on
PICOT framework (P: diabetes mellitus type 2, I:
internet, computer, telephone, electronics, telehealth,
C: -, O: behavior, lifestyle, blood sugar control, self-
management, T: 2009-2018). A full of literature
search and study selection process in accordance
with the PRISMA guidelines. Studies are included
when describing interventions with electronic media
targeted at patients with type 2 diabetes, focusing on
behavior, biomedical, and psychological.
2.3 Sample
Based on the search results obtained 1072 articles
and 15 articles that meet the inclusion criteria. Each
study creates educational interventions using
electronic media designed to promote diabetes
education and some changes in health behavior.
From 15 journals reviewed 13 articles with
randomized control trial design (RCT) while 2
papers used quasi-experimental design. Each study
uses electronic media designed for the promotion of
diabetes education. There are 5 out of 15 reviewed
papers focusing on behavior change, 11 out of 15
papers focusing on biomedical changes, and 7 out of
10 papers focusing on the psychological aspects.
2.4 Eligibility Criteria
Articles selected for review based on studies that
match inclusion criteria. The inclusion criteria are
electronic use and are not limited by the type of
electronics used as educational media that target
adults with type 2 diabetes mellitus, focusing on
behavioral, biomedical, and psychological changes.
Studies that focus exclusively on glucose monitoring
or electronic health records/web portals to upload
data are not included.
Lifestyle Education Based on Electronic Media for Diabetes Management
221
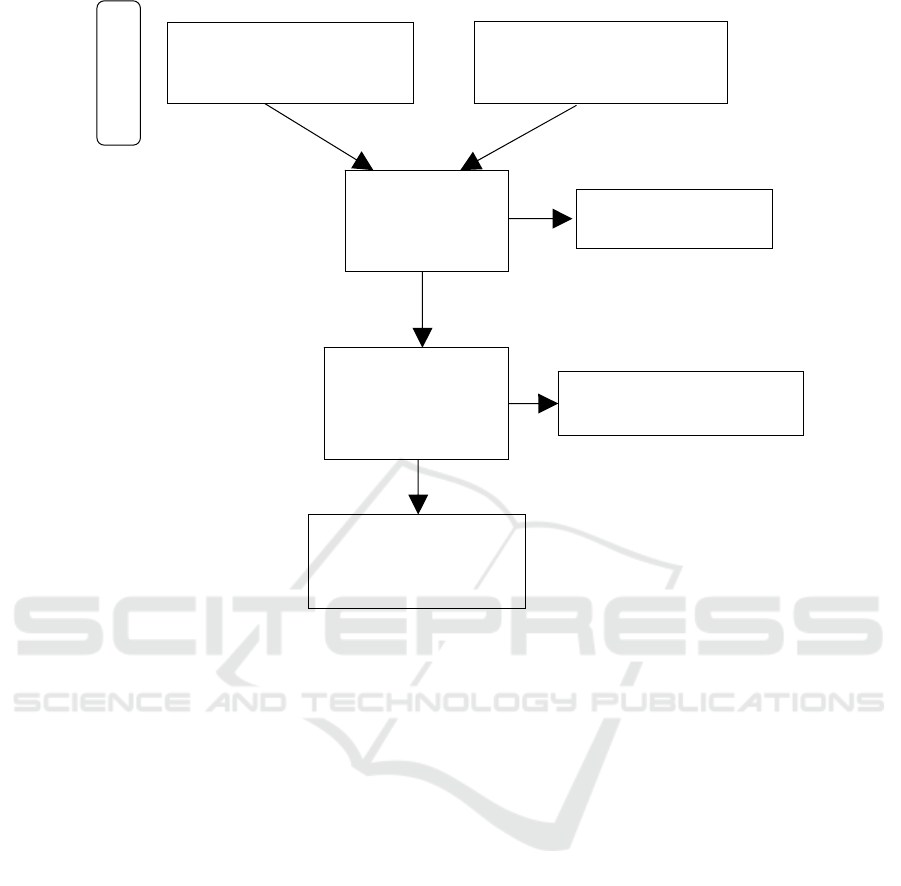
Figure. 1: flow diagram of search results for lifestyle education based on electronic media for diabetes management
according with the PRISMA guidelines.
3 RESULTS
3.1 Overview of Studies
Based on the search results obtained 1072 articles
and 15 articles that meet the inclusion criteria, 13
articles with randomized control trial design (RCT)
while 2 papers used quasi-experimental design.
Electronic media used from all articles are 8 articles
using telephone, 1 article using DVD, 1 article using
a computer, 1 article using television, 1 article using
videoconveren, and 3 articles using web based.
3.2 Outcome
There are three main results obtained in this review
that is the effect of electronic media as a medium of
education on behavioral, on biomedical, and on the
psychological aspects of patients with type 2
diabetes mellitus.
3.2.1 Behavioral Outcomes
Half of the studies reviewed looked for outcomes for
changes in activity (5/10). Changes in activities
assessed are diet and physical activity. Tokunaga et
al., (2014) reported that computer-based lifestyle
interventions decreased significantly greater energy
intake six months after baseline (p = 0.0099), Karim
et al., (2011) reported had no significant effect on
diabetic self-care behavior after obtaining a
multimedia-based (video) education intervention.
Educational interventions using telephone media can
increase physical activity and decrease nutrient
intake (p = 0.02) (Chamany et al., 2015; Swoboda,
et al., 2017). (Greef et al., 2011) reported that
behavioral modification interventions with the phone
increased their / day move in 2744, their total PA by
23 minutes / day (p <0.001) and decreased their
sedentary behavior by 23 minutes/day (p <0.05).
Additional records identified
through other sources
(n = 156)
Records excluded
(n=810)
Full text articles excluded
(n=18)
Records identified through
database searching
(n = 916)
Records screened
after duplicates
removed
(
n = 843
)
Full text articles
assessed for
eligibility
(n = 33)
Studies included in
integrative review
(n = 15)
Id
ent
ifi
cat
i
on
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
222
3.2.2 Biomedical Outcomes
The most widely measured biomedical outcome was
the HbA1c value. All of the biomedical assessments
all measured HbA1c (11/15). Eight research reported
a greater decrease in HbA1c values in the
intervention group than in the control group (Aguiar
et al., 2016; Chamany et al., 2015; Goodarzi et al,
2012; Karim et al, 2011; Moattari et al, 2012; Davis
et al, 2010; Tavşanli, 2013; Yoo An et al, 2010)
Education with telephone effective to decreases the
HbA1c value at six month compared with the
control group (p = 0.013) (Tavşanli, 2013).
Meanwhile, according to Tokunaga Metal., (2014)
no difference HbA1c in the intervention group with
the control group in the use of the computer as
educational media. Dale et al., (2009); Pacaud et al,
(2012) also reported no difference HbA1c in the
intervention group with the control group in the use
of telephone as educational media. Another
biomedical that is also measured is the body mask
index. The use of DVD-based educational media can
significantly reduce BMI (p <0.0001) (Aguiar et al.,
2016). However, telephone-based education
interventions have no effect on BMI (Karim et al.,
2011; Tokunaga et al., 2014).
3.2.3 Psychology Outcomes
There are seven studies reviewed with outcome
psychology. Psychology outcome that many in
measure is self efficacy (6/10). According to (Lari
et al, 2018) the use of teching cd base can improve
self efficacy of type 2 DM patients compared with
control group (P <0.001). Similarly, (Goodarzi et al.,
2012; Swoboda et al., 2017) support telephone
coaching intervention can improve self efficacy
significantly compared to the control group (0.002)
and also effectively reduce stress (0.004), Pacaud et
al., (2012) reports that there is an increase in self-
efficacy after education with web-based. Whereas
other research reported no effect of multimedia-
based education and telephone on self efficacy (Dale
et al., 2009; Karim et al., 2011). Other psychological
data reported by research that electronic-based
education can improve the empowerment of people
with diabetes mellitus type 2 (Zamanzadeh et al,
2016; Swoboda et al 2017)
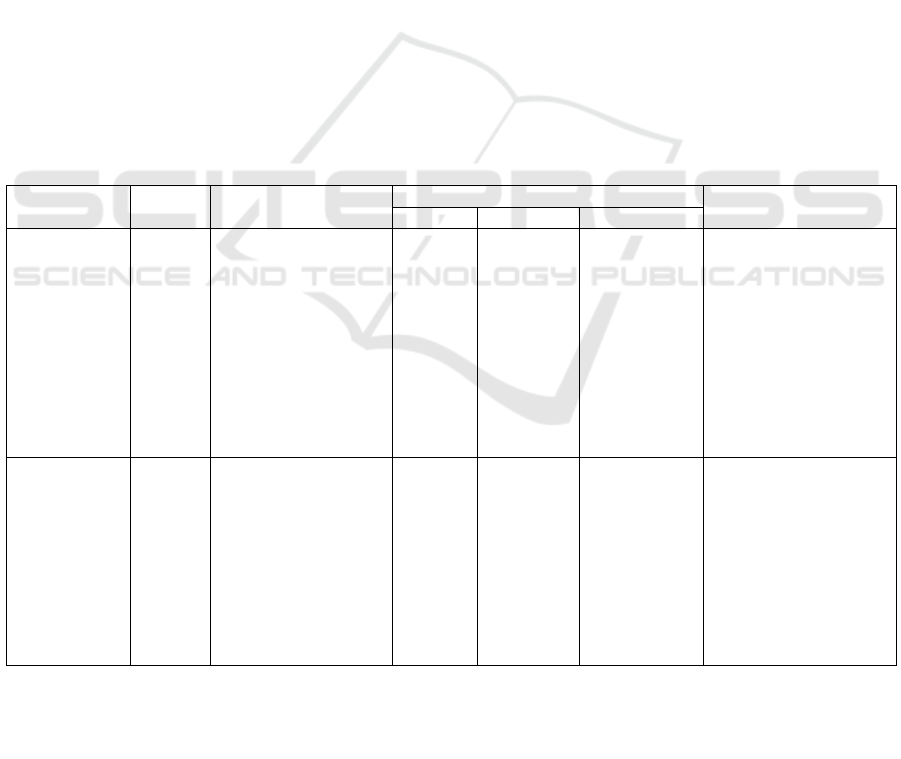
Table 1: Measured outcomes and results of electronic based type 2 diabetes studies meeting inclusion criteria
Author, year Study
Design
Sampel Outcome results
b
ehavio
r
b
iomedical
p
sycological
(Tokunaga-
nakawatase,
Nishigaki and
Taru, 2014)
RCT patients with diabetes
mellitus aged 30-60
years n=141
energy
intake
physical
activity
levels
BMI
HbA1c
Colesterol
a significantly greater
decrease in energy
within six months from
the beginning of the
intervention, compared
with control (p =
0.0099) and No
differences were found
in physical energy
expenditure.
(Zamanzadeh,
Zirak and
Hemmati,
2016)
RCT patients with type 2
diabetes n = 66
The
empowerment
There was a
significantly increased
empowerment in the
intervention group
compared with the
control group after
three months of
distance education (p
<0.00, EF = 1.16).
Lifestyle Education Based on Electronic Media for Diabetes Management
223
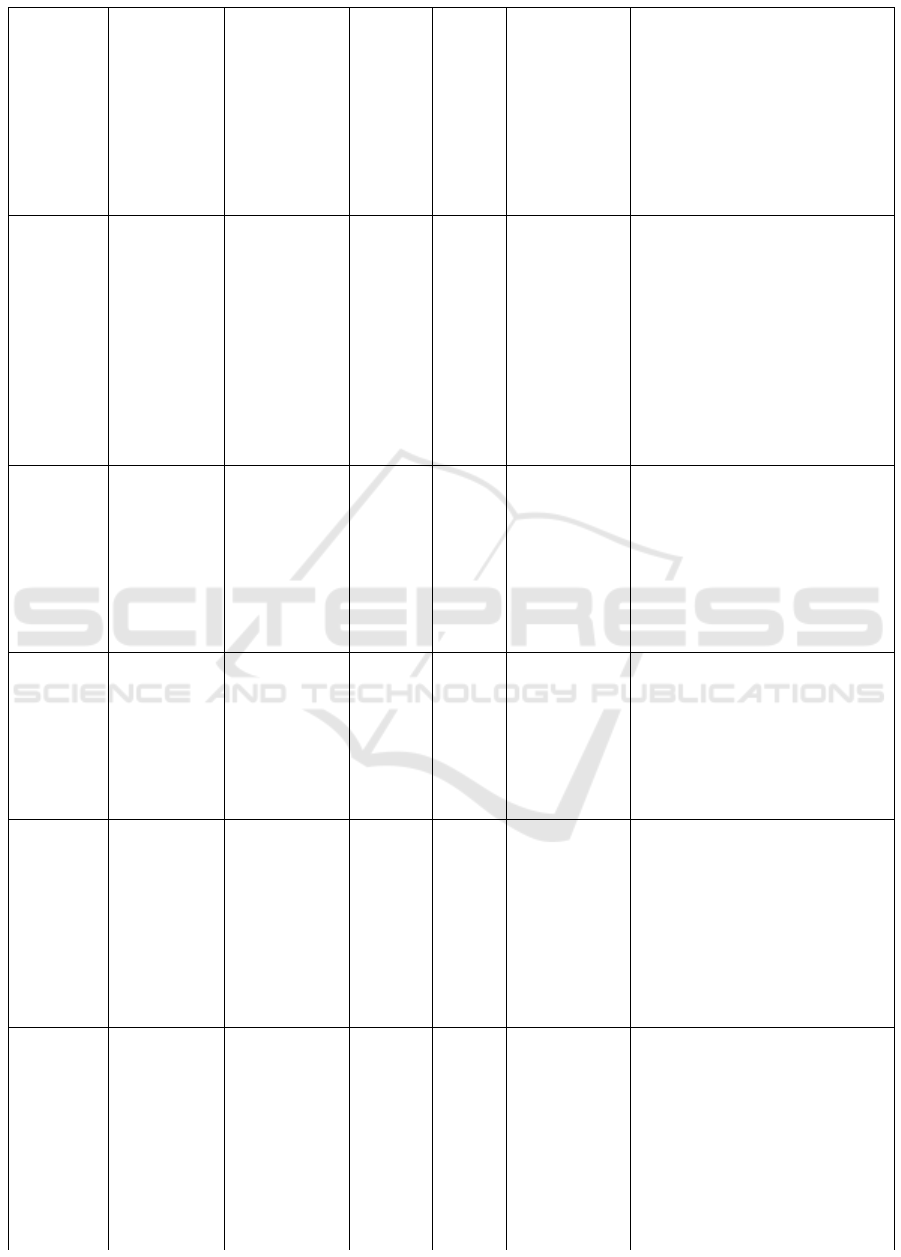
(Lari,
Tahmasebi
and
Noroozi,
2018)
quasi-
experimental
Patient with
type II
diabetes in the
city of
Bushehr, a
southwestern
province in
Iran.
n = 80
Psycal
activity
Self efficacy
Friend
support
There were significant
differences between the
intervention group and the
control group, health status (p =
0.032), self-efficacy (p <0.001),
peers support in physical activity
(p <0.001), physical activity (P
<0.001), (p <0.001) and
equivalent metabolic task (MET)
(p <0.001).
(Karim
and
Gerber,
2011)
RCT Ethnic
minorities
with type 2
diabetes
received care
from a local
clinic in
Chicago,
Illinois.
n = 129
Physical
activity
HbA1c Self efficacy The results obtained were an
increase in the number of oral
diabetes drugs (p = 0.017).
HbA1c (p = 0.06). There was no
difference between the
intervention and control groups
in self-efficacy, blood pressure,
and diabetes-related behaviors.
The exercise increased in the
control group compared with the
multimedia group (p = 0.016)
(Chamany
et al.,
2015)
RCT Adults with
diabetes
mellitus
n = 941
HbA1c
BMI
Pysical
activity
The results obtained decreased
HbA1c in the intervention group
0.9 and in the control group 0.5
(p = 0.01). Both groups
experienced similar
improvements in self-care
activities, medication adherence,
and intensification.
(Dale et
al., 2009)
RCT Pasient with
diabetes
melitus.
n=231
HbA1c
BMI
Self efficacy The results obtained are no
statistically significant difference
self-efficacy score (p = 0.68),
HbA1c (p = 0.87) or other
secondary outcome measures
between the intervention group
and the control group
(Swoboda,
Miller and
Wills,
2017)
RCT Patient with
diabetes
melitus from
a
metropolitan
area in the
Midwestern
United States
n=54
Healty
eating
indext
Self efficacy
Diabetes
empowerment
Diabetes
distress
The results obtained were
increased empowerment of
diabetes (p = 0.045), diet quality,
self-efficacy, diabetes
empowerment, and depressive
symptoms (all p <0.05) occurred
in the intervention group.
(Greef et
al., 2011)
quasi-
experimental
Patient with
diabetes
melitus in
endocrinology
department of
the Ghent
University
Hospital,
Belgium
n=92
Pysical
activity
The results obtained were
increased physical activity in the
intervention group compared
with the control group (p
<0.001). After 1 year the
intervention group still had total
physical activity (p <0.001).
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
224
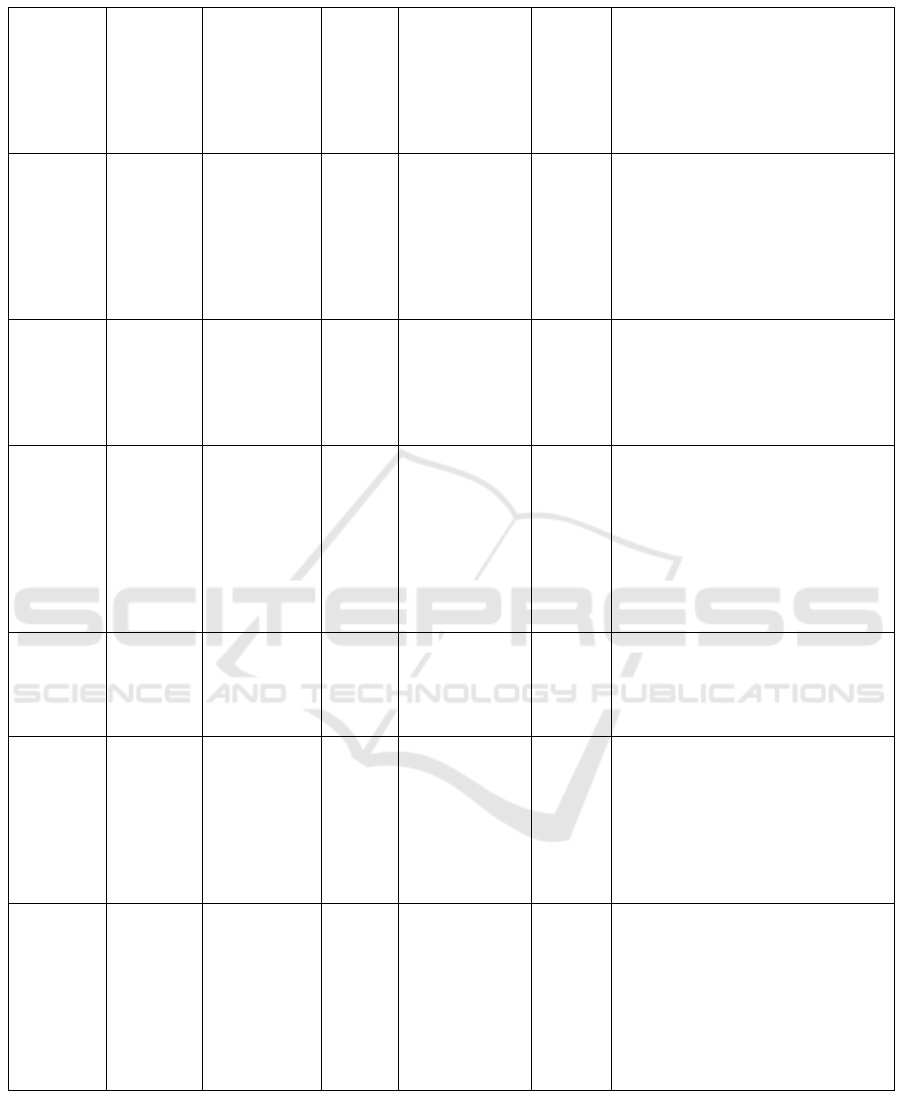
(Aguiar et
al., 2016)
RCT Men with
Type 2
diabetes,
New South
Wales,
Australia
n=101
HbA1c
BMI
weight
The results obtained were the
differences in weight loss between
the intervention group and the
control group (p <0.001), BMI (p
<0.05), and glycated hemoglobin
(P<0.002)
(Tavşanli,
2013)
RCT Patient with
diabetes
melitus
n=48
HbA1c
Blood glucose
The results obtained at the end of
six months monitoring that the
individual A1c levels in EG were
preprandial blood glucose levels of
diabetic patients in EG were lower
than that of prepregulated diabetic
blood glucose in CG significantly.
(Goodarzi
et al.,
2012)
RCT Patient with
diabetes
melitus
n=81
HbA1c,
cholesterol
triglycerides
HDL
LDL
Self
efficacy
The results obtained were
significant differences between
experimental groups compared with
HbA1c control (p = 0.0024), LDL
(p = 0,019), cholesterol (p = 0.002),
and self efficacy (p <0.001).
(Pacaud et
al., 2012)
RCT Patient with
diabetes
melitus
n=79
HbA1c Self
efficacy
The results of the comparison
between the intervention group and
the control group were increased
diabetes knowledge (p = 0.005),
self efficacy (p = 0.019), and self-
care (p = 0.006). Not significant
between group differences in
HbA1C
(Moattari
et al.,
2012)
RCT Patient with
diabetes
melitus
n=48
HbA1c
total
cholesteroHDL
LDLl
The results of the differences
between the intervention and
control groups were HbA1c (p
<0.001) and LDL (P <0.02)
(Yoo et
al., 2010)
RCT Patient with
diabetes
melitus
n=40
HbA1c
blood pressure,
body
mass index,
triglycerides,
HDL
LDL
The result was a significant
decrease in HbA1c value in the
intervention group compared with
the control group (p = 0.031), but
no other value difference between
the groups
(Davis et
al 2010)
RCT Patient with
diabetes
melitus
n=165
HbA1c
LDL
The results obtained were
significant decreases in the first 6
months of HbA1c values in the
intervention group compared with
the control group (p = 0.003),
baseline to 12 months (p = 0.004),
and LDL cholesterol from baseline
to 12 months (p = 0.02
Lifestyle Education Based on Electronic Media for Diabetes Management
225

4 DISCUSSION
People with a family history of type 2 diabetes often
lack sufficient knowledge of lifestyle behaviors in
preventing diabetes and it is difficult for medical
professionals to motivate them to change their
lifestyle habits (Tokunaga et al., 2014). An effective
and efficient medium is needed to assist in the
delivery of information to patients.
This study synthesizes evidence of the use of
electronic media in the provision of lifestyle
education in people with type 2 diabetes mellitus.
The most widely used electronic media is the
telephone. There are 7 papers that use the phone as
an educational media and the each other use
computers, CDs, DVD, multimedia (television) and
web-based.
Two studies have shown improvement in diit
after obtaining educated electronic education
(Swoboda et al., 2017; Tokunaga-nakawatase et al.,
2014). These two studies use different electronic
media, one using a computer (Tokunaga-nakawatase
et al., 2014) and one using a telephone (Swoboda et
al., 2017). This shows that the use of the phone is
not necessarily better than the computer and vice
versa. Two studies have also shown improvement in
physical activity after receiving telephone-based
education interventions (Chamany et al., 2015;
Greef et al., 2011).
In biomedical results, four studies showed
improvement of glycemic profile (HbA1c) compared
with control group (Aguiar et al., 2016; Chamany et
al., 2015; Karim et al, 2011; Tavşanli, 2013).
Interventions applied were education with phone
media (Chamany et al., 2015; Tavşanli, 2013) with
DVD-multimedia (Aguiar et al., 2016) and
television multimedia in patient waiting room
(Karim & Gerber, 2011). While the other 3 studies
show the opposite result where educational
intervention with computer electronic media
(Tokunaga-nakawatase et al., 2014) and telephone
(Dale et al., 2009) did not show significant result in
lowering HbA1c.
Further research is needed to examine effective
methods of using electronic as an educational
medium and an optimal utilization pattern is
required and how the pattern varies according to the
target behavior / outcomes by individual users with
the assumption of some optimal "dose" interaction
with the required electronic-based program (Cotter,
Durant, Agne, & Cherrington, 2014). Another point
that is also often measured in the biomedical aspect
is BMI, from three studies that measured BMI
showed no effect of electronic-based educational
intervention on BMI (Karim & Gerber, 2011;
Tokunaga-nakawatase et al., 2014). This is because
it requires a continuous program in a long time to
generate changes in the value of BMI.
Psychology results in some studies focus more
on self efficacy. Self efficacy is a belief in one's
ability to perform a task that will produce the desired
result. Utilizing self-efficacy counseling skills is an
effective way to improve patient compliance with
self-care activities (Gb and Premkumar, 2016).
There are four studies showing that electronic-based
education intervention can increase self efficacy
significantly (Goodarzi et al., 2012; Lari et al., 2018;
Pacaud et al., 2012; Swoboda et al., 2017) and two
studies show no influence (Dale et al., 2009; Karim
and Gerber, 2011). This is because many factors
influence the self-efficacy so that it is required to
tightly control the other variables that may affect.
Factors that may affect self efficacy are the
previous positive and negative experiences
experienced by others, other people's experiences,
support or ambition from others, psychological and
emotional conditions (Bandura, 1994). In addition to
self-efficacy other factors assessed are stress and
empowerment. Electronic-based education can
reduce stress and increase the empowerment of
people with diabetes mellitus type 2 (Zamanzadeh,
Zirak and Hemmati, 2016; Swoboda, Miller and
Wills, 2017). The greatest challenge of any kind of
educational intervention including by involving
electronic media is to achieve patient adherence to
healthy behaviors over time.
5 CONCLUSIONS
The rapid development of informatics technology
can be utilized in the provision of optimal health
services in patients, especially patients with diabetes
mellitus type 2. Use of electronic media is the most
widely used is the telephone due to its practicality.
The use of electronic media can be an option in
providing educational intervention in patients with
diabetes type 2 can be more effective and efficient.
The study discussed in this paper demonstrates the
ability of electronic-based education interventions to
successfully reach patients and promote appropriate
lifestyle modifications. The results shown can be
concluded that the use of electronic media as an
educational medium in diabetes patients is effective
in changing the behavior, blood sugar control and
patient psychological aspects. This intervention
provides an appropriate choice to facilitate
independent management processes outside of
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
226

clinical settings. However, further research on
utilization patterns that conforms to the assumption
of some optimal "dose" interaction with the
necessary electronic-based programs is required.
REFERENCES
Aguiar, E. J., Morgan, P. J., Collins, C. E., Plotnikoff, R.
C., Young, M. D., & Callister, R. (2016). Efficacy of
the Type 2 Diabetes Prevention Using LifeStyle
Education Program RCT. American Journal of
Preventive Medicine, 50(3), 353–364.
https://doi.org/10.1016/j.amepre.2015.08.020
Bandura. (1994). Self-efficacy. In V. S. Ramachaudran
(Ed.) Encyclopedia of human behavior (Vol. 4, pp. 71-
81). New York: Academic Press.
Booth, A. O., Lowis, C., Hunter, S. J., Dean, M.,
Cardwell, C. R., & Mckinley, M. C. (2016).
Development and Evaluation of a Computer - Based ,
Self - Management Tool for People Recently
Diagnosed with Type 2 Diabetes, 2016.
https://doi.org/10.1155/2016/3192673
Chamany, S., Walker, E. A., Schechter, C. B., Gonzalez, J.
S., Davis, N. J., Ortega, F. M., … Silver, L. D. (2015).
Telephone Intervention to Improve Diabetes Control.
American Journal of Preventive Medicine, 1–10.
https://doi.org/10.1016/j.amepre.2015.04.016
Cotter, A. P., Durant, N., Agne, A. A., & Cherrington, A.
L. (2014). Journal of Diabetes and Its Complications
Internet interventions to support lifestyle modi fi
cation for diabetes management : A systematic review
of the evidence ☆ , ☆☆. Journal of Diabetes and Its
Complications, 28(2), 243–251.
https://doi.org/10.1016/j.jdiacomp.2013.07.003
Dale, J., Caramlau, I., Sturt, J., Friede, T., & Walker, R.
(2009). Patient Education and Counseling Telephone
peer-delivered intervention for diabetes motivation
and support : The telecare exploratory RCT, 75, 91–
98. https://doi.org/10.1016/j.pec.2008.09.014
Departemen Kesehatan RI. (2014). Pusat Data dan
Informasi Kementerian Kesehatan RI: Situasi dan
Analisis Diabetes. Jakarta.
Gb, M., & Premkumar, J. (2016). Eff ects of a Behavioral
Intervention on Self-Effi cacy , Self- Care Behavior
and HbA1c Values among Patients with Type 2
Diabetes Mellitus, 1–6.
Goodarzi, M., Ebrahimzadeh, I., Rabi, A., Saedipoor, B.,
& Jafarabadi, M. A. (2012). Impact of distance
education via mobile phone text messaging on
knowledge , attitude , practice and self efficacy of
patients with type 2 diabetes mellitus in Iran, 1–8.
Greef, K. P. De, Deforche, B. I., Ruige, J. B., Bouckaert,
J. J., Tudor-locke, C. E., Kaufman, J., &
Bourdeaudhuij, I. M. De. (2011). Patient Education
and Counseling The effects of a pedometer-based
behavioral modification program with telephone
support on physical activity and sedentary behavior in
type 2 diabetes patients. Patient Education and
Counseling, 84(2), 275–279.
https://doi.org/10.1016/j.pec.2010.07.010
Higano, K. (2015). The Effects of Telenursing with Goal
Attainment Scaling in Diabetic Patients
: A Case
Report International Journal of Nursing & Clinical
Practices, 2, 6–8.
International Diabetes Federation (IDF) . (2013). IDF
Diabetes Atlas Sixth Edition, International Diabetes
Federation (IDF).
Karim, M. A. K. S. S. A. G. N. O. P. B. S., & Gerber, J. J.
Y. K. B. S. (2011). A Diabetes Education Multimedia
Program in the Waiting Room Setting, 2, 178–188.
https://doi.org/10.1007/s13300-011-0007-y
Lari, H., Tahmasebi, R., & Noroozi, A. (2018). Diabetes
& Metabolic Syndrome : Clinical Research & Reviews
Effect of electronic education based on health
promotion model on physical activity in diabetic
patients. Diabetes & Metabolic Syndrome: Clinical
Research & Reviews, 12(1), 45–50.
https://doi.org/10.1016/j.dsx.2017.08.013
Moattari, M., Hashemi, M., & Dabbaghmanesh, M. H.
(2012). The impact of electronic education on
metabolic control indicators in patients with diabetes
who need insulin : a randomised clinical control trial,
1–7. https://doi.org/10.1111/j.1365-
2702.2012.04200.x
Pacaud, D., Kelley, H., Downey, A. M., & Chiasson, M.
(2012). Successful Delivery of Diabetes Self-Care
Education and Follow-Up through eHealth Media.
Canadian Journal of Diabetes, 36(5), 257–262.
https://doi.org/10.1016/j.jcjd.2012.08.006
PERKENI. (2015). Pengelolaan dan pencegahan diabetes
melitus tipe 2 di indonesia 2015.
Richard M. Davis, Angela D. H itch, Muhammad M.
Salaam, W illiam H. Herman, Ingrid E. Zimmer-
Galler, E. J. . M.-D. (2010). T e le H e a lth Im p ro
ves D ia b e te s S e lf-M a n a g e m e n t in an U n d e
rs e rv e d C om m unity, 33(8).
https://doi.org/10.2337/dc09-1919.
Swoboda, C. M., Miller, C. K., & Wills, C. E. (2017).
Patient Education and Counseling Impact of a goal
setting and decision support telephone coaching
intervention on diet , psychosocial , and decision
outcomes among people with type 2 diabetes. Patient
Education and Counseling, (2016).
https://doi.org/10.1016/j.pec.2017.02.007
Tavşanli, N. G. (2013). The use of videophone technology
( telenursing ) in the glycaemic control of diabetic
patients : a randomized controlled trial.
https://doi.org/10.7243/2050-0866-2-1
Tokunaga-nakawatase, Y., Nishigaki, M., & Taru, C.
(2014). lifestyle-modification support program using
Lifestyle Intervention Support Software for Diabetes
Prevention ( LISS-DP ) for people with a family
history of type 2 diabetes in a medical checkup
setting : A randomized controlled trial. Primary Care
Diabetes, 8(3), 207–214.
https://doi.org/10.1016/j.pcd.2014.01.007
Yoo, H., An, K., & Ph, D. (2010). Web-Based
Comprehensive Information System for Self-
Lifestyle Education Based on Electronic Media for Diabetes Management
227

Management of Diabetes Mellitus, 12(5).
Zamanzadeh, V., Zirak, M., & Hemmati, M. (2016).
Diabetes & Metabolic Syndrome : Clinical Research &
Reviews Distance education and diabetes
empowerment : A single-blind randomized control
trial. Diabetes & Metabolic Syndrome: Clinical
Research & Reviews.
https://doi.org/10.1016/j.dsx.2016.12.039
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
228
