
Family Support, Self-efficacy, Motivation, and Treatment Adherence
in Multidrug-resistant Tuberculosis Patients
Tintin Sukartini, Ika Minarni and Candra Panji Asmoro
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
Keywords: Family Support, Self-efficacy, Motivation, Treatment Adherence.
Abstract: Multidrug resistance (MDR) is caused by treatment inadherence. Inadherence is known to increase the risk
of MDR tuberculosis (TB) by 2.3 times. Inadherence is prompted by a knowledge deficit, low self-efficacy,
and poor motivation. Family support could be a solution to adherence problems. This study aimed to
analyze the correlation of family support with self-efficacy, motivation, and treatment adherence in MDR
TB patients. A cross-sectional study involved 55 respondents who were selected using consecutive
sampling. The independent variable was family support. The dependent variables were self-efficacy,
motivation, and treatment adherence. Data were retrieved through the completion of a questionnaire then
analyzed statistically using the Spearman rank rho and Chi-square with α ≤ 0.05. Family support did not
significantly correlate with self-efficacy with p-value = 0.429 or (p ≥ 0.05). Family support significantly
correlated with motivation p-value = 0.043 r = 0.275 (p ≤ 0.05), and treatment adherence p-value = 0.037 or
(p ≤ 0.05). TB MDR treatment should optimize family involvement to increase motivation and adherence.
Further research suggests using counseling to improve family involvement in supporting MDR TB patients.
1 BACKGROUND
Multidrug-resistant tuberculosis (MDR TB) is the
tuberculosis (TB) disease that has resistance to
isoniazid (INH), rifampicin, and one or more anti-
tuberculosis drugs based on standardized laboratory
tests and occurs due to treatment failure, stopping
treatment, or improper treatment, resulting in the
occurrence of primary resistance (WHO, 2015). The
results showed that non-adherence of patients during
treatment increased the risk of developing MDR TB
by 2.3 times compared with patients who were
adhered to treatment (Farmani, 2015).
By 2015 it is estimated that 3.9% of new cases
and 21% of old cases will have MDR TB,
accounting for 580,000 cases. Indonesia ranks 4th in
MDR TB cases with an estimated 32,000 cases with
2.8% of new cases and 16% of old cases (WHO,
2016). Based on data from Infodatin Ministry of
Health Republic of Indonesia (2016) the number of
new cases of Pulmonary TB AFB (acid fast bacilli)
+ + in East Java, in 2016, Indonesia ranks second,
with 21,606 new cases. Data of preliminary study
results at the TB MDR clinic, Dr. Soetomo Hospital,
Surabaya indicated 64 MDR TB patients, a total of
40 adherent patients and 24 inadherent patients, who
refused to undergo intensive phase treatment.
Drug supervisors have a role in preventing the
occurrence of non-compliance medication. The
family of the patient can take that role. Glick et al. in
Maulidia (2014) explains that medication adherence
increases when patients receive support from the
family. Muhtar (2013) discusses the influence of
family empowerment in improving self-efficacy.
Patients with supportive families who promote
family empowerment interventions, including self-
care, had a higher self-efficacy than the control
group. Sukartini (2015) showed that social support
from family and officers, who had knowledge and
perceptions regarding TB, had a positive effect on
motivation for the adherence of treatment.
Deskhmund et. al (2017) state that one of the factors
that can improve treatment compliance is social
support.
Positive family support is needed in the
treatment of TB disease that requires long-term
medication. Support comprises of providing
information verbally or non-verbally, and real
assistance or action is given via social intimacy or is
gained through the presence of the family, who can
have an emotional or behavioral benefit to the
178
Sukartini, T., Minarni, I. and Asmoro, C.
Family Support, Self-efficacy, Motivation, and Treatment Adherence in Multidrug-resistant Tuberculosis Patients.
DOI: 10.5220/0008322301780182
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 178-182
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
recipient (Royce, S. et al., 2014). Problems found at
the TB clinic in the government hospital were
related to forms of non-adherence to treatment,
which tends to occur in patients with low family
support. The researcher intends to further examine
the relationship between family support and
compliance, motivation, and self-efficacy during the
treatment of multidrug-resistant tuberculosis (MDR
TB).
The purpose of this study is to analyze the
correlation of family support with self-efficacy,
motivation, and treatment adherence in MDR TB
patients.
2 METHODS
2.1 Design
This study used a cross-sectional design.
2.2 Sample
The population in this study are MDR TB patients
undergoing treatment at the MDR TB clinic during
November 2017. A consecutive sampling technique
was used in this study. The sample size was 55
respondents.
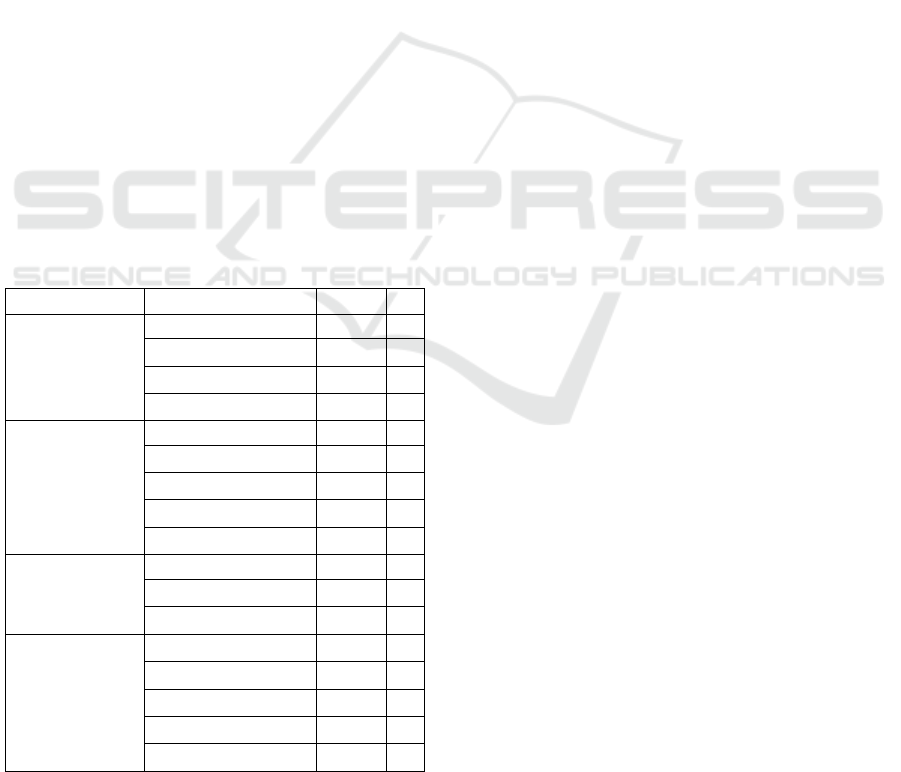
Table 1: Characteristics of multidrug-resistant patients.
Characteristic
Indicators
f (x)
%
Age
15–25 y.o.
7
13
26–45 y.o.
21
38
46–70 y.o.
27
49
Total
30
100
Education
Primary school
10
18
Junior high school
8
15
Senior high school
28
51
Bachelor
9
16
Total
55
100
Gender
Male
35
64
Female
20
36
Total
55
100
Profession
Housewife
10
20
Entrepreneur
11
18
Civil servant
4
8
Security
30
54
Total
55
100
The inclusion criteria for the sample in this study
are: MDR TB patients accompanied by family, aged
15–70 years, cooperative, able to communicate
verbally, and able to read and write.
2.3 Instrument
The instrument used was a questionnaire regarding
family support using the Source of Social Support
Scale (SSSS), a self-efficacy questionnaire, a
motivational questionnaire, and a compliance
observation sheet.
2.4 Data Collection
Data were collected using the questionnaire. Test
statistics in the study were analyzed using the
Spearman rank and Chi-square tests. The Spearman
rank test was used to analyze family support data
regarding self-efficacy and motivation. The Chi-
Square test was used to analyze family support
regarding adherence.
2.5 Ethical Clearance
This study obtained ethical clearance from the
Research Ethics Committee at Faculty of Medicine,
Universitas Airlangga: No. 418/EC/KEPK/FKUA/
2016.
3 RESULTS
Table 1 indicates that more than half of the
respondents in the study (70%) were between 26 and
45 years old; more than half (51%) of the
respondents have a high-school education
background; more than half (64%) of respondents
are male; and more than half (54%) of respondents
have background jobs with other categories such as
security guards and drivers.
Table 1 demonstrates that most patients are 46–
70 years old, graduates from senior high school,
male, and work in security.
3.1 Correlation of Family Support with
Self-efficacy in Multidrug-resistant
Tuberculosis Patients
Table 2 shows the results of the Spearman rho
statistics test, which determined that family support
does not significantly correlate with self-efficacy.
Family Support, Self-efficacy, Motivation, and Treatment Adherence in Multidrug-resistant Tuberculosis Patients
179
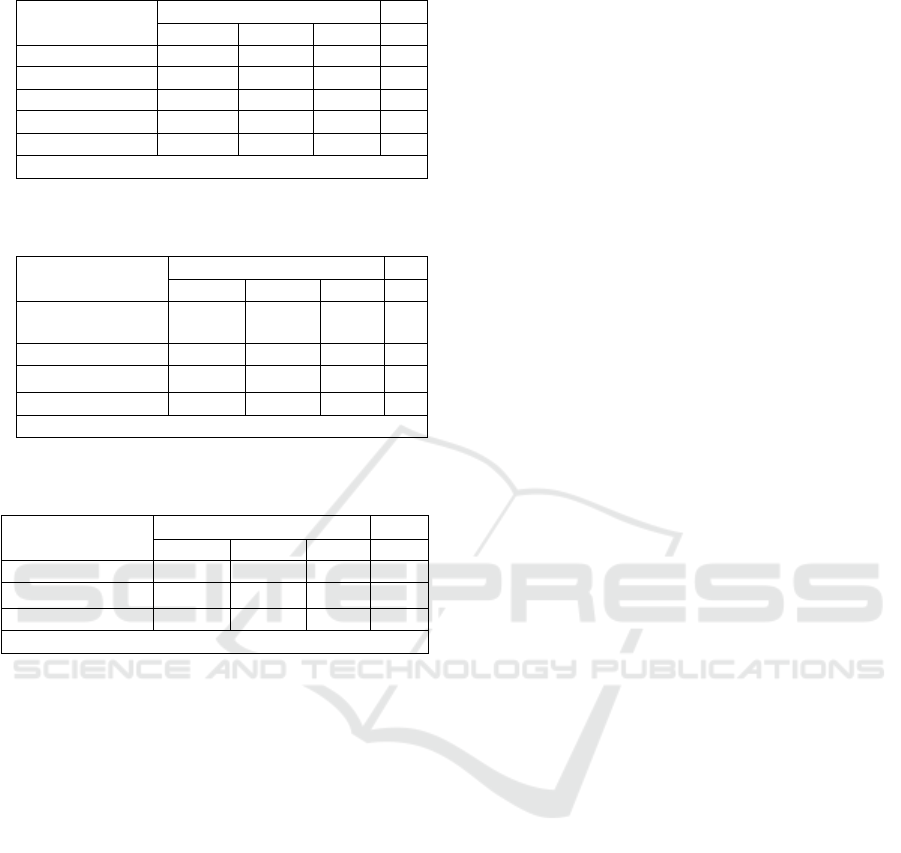
Table 2: Correlation of family support with self-efficacy.
Variable
Family support
Low
Moderate
High
Total
Self-efficacy
Low
1
2
0
3
Moderate
20
7
0
27
High
14
10
1
25
Total
35
19
1
55
Spearman rho p-value = 0.429
Table 3: Correlation of family support with motivation in
multidrug-resistant tuberculosis patients.
Variable
Family support
Total
Low
Moderate
High
Motivation
Low
9
0
0
9
Moderate
13
9
0
22
High
13
10
1
24
Total
35
19
1
55
Spearman rho p-value = 0.043 or (p ≤ 0.05)
Table 4: The correlation of family support with treatment
adherence in multidrug-resistant patients.
Variable
Family Support
Total
Low
Moderate
High
Adherence
7
9
0
17
Non-adherence
28
10
0
38
Total
35
19
1
55
Chi square p-value = 0.037
3.2 Correlation of Family Support with
the Motivation of Multidrug-
resistant Tuberculosis Patients
Table 3 shows the results of the Spearman rho test
statistical test regarding the correlation of family
support with patient motivation.
3.3 The Correlation of Family Support
with Treatment Adherence in
Multidrug-resistant Tuberculosis
Patients
Table 4 shows the results of the Chi-square test,
which indicated a significance of p = 0.037. These
results showed a significant correlation between
family support and treatment adherence.
4 DISCUSSION
A small percentage of respondents demonstrated
moderate self-efficacy but low family support. The
results of the statistical tests indicated no significant
correlation between family support and self-efficacy
in MDR TB patients.
The results of this study are not consistent with
work by Hendiani, Sakti and Widayanti (2012),
which suggests that family members supporting as
drug supervisors do have a correlation with self-
efficacy in pulmonary TB patients. The results
showed that patients who had positive perceptions of
family support in supervising drug had a higher self-
efficacy. Self-efficacy is not only formed by family
support, but also by knowledge, attitude, high self-
esteem, feelings of sufficient ability, confidence to
act, and trust their ability to change situations
(Notoatmodjo, 2010).
The Spearmen rho statistical test results found a
significant relationship between family support and
motivation in patients with MDR TB. According to
John Elder (Notoatmodjo, 2007), motivation is an
interaction between behavior and environment, so
can increase, decrease, or maintain behavior. This
result is consistent with a study by Sutarno and
Utama (2012), which indicates that social support
from family and health workers, and sufficient
knowledge and perceptions about TB, has a positive
effect on motivation for treatment. According to
Mohammadi (2009) motivation is needed to
encourage patients to be actively involved in the
control of the disease.
The correlation between family support and
motivation in MDR TB patients indicates that
families can encourage MDR TB patients to
consistently adhere to treatment programs. Family
support has a positive effect on respondents'
motivation to seek treatment.
Most respondents who demonstrated non-
adherence to treatment of MDR TB, had insufficient
family support. The results of the Chi-square
statistics test indicated that there was a significant
correlation between family support and MDR TB
patient compliance. The results of the study are
consistent with Maulidia (2014), who showed a
significant correlation between family support and
treatment adherence for tuberculosis patients.
The results of the study are consistent with
Hutapea (2009), who studied the effect of family
support on treatment adherence. The results
indicated that there is an influence of family support
on the regularity of taking medication. More than
half of respondents take medication once daily. The
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
180

statistics of these two studies equally emphasize the
impact of family support on patient treatment
adherence.
The results are consistent with Wilson et al.
(2016) who suggest that video-based education
regarding TB for families be successfully
implemented in busy and resource-limited outpatient
settings, and can provide a potentially efficient and
low-cost effective strategy towards optimizing
patient understanding, acceptance, and compliance
with TB treatment recommendations
This study is consistent with work by
Castelnuovo (2013) who conducted a review of
compliance in anti-tuberculosis treatment. The risk
factors for defaulting treatment were: distance from
the hospital, not being on the first course of TB
medication, lack of repeated smears, unit transfer
after the intensive phase, experiencing side effects,
having no family support, poor knowledge about TB
treatment, being more than 25 years old, and the use
of public transport.
Sagbakken, Frich and Bjune (2008) investigated
barrier and enablers in the management of
tuberculosis treatment, through a qualitative study.
Their result showed that patients with limited access
to financial or practical help from relatives or friends
experienced barriers to adherence during the early
stages of treatment.
Akshata and Chakrabarthy (2016) studied the
management of multidrug-resistant tuberculosis
(MDR TB). They discovered that monitoring is the
key to successful outcomes. Their results indicated
that early diagnosis of MDR TB, and adequate
clinical monitoring during treatment, is essential.
Identifying adverse drug reactions, other co-
morbidities, and their optimal management are keys
to success.
Adherence is a behavior that can be planned for.
Treatment adherence is the result of interaction
planning for internal and external factors of MDR
TB patients. Family support is an external
reinforcing factor as well as an enabling source of
support when MDR patients become less motivated
to seek treatment. Constant family support will form
consistent patient compliance behavior.
5 CONCLUSIONS
Family support has no significant correlation with
self-efficacy but has a significant correlation with
motivation and adherence to the treatment of
multidrug-resistant tuberculosis (MDR TB).
REFERENCES
Akshata, J. S., Chakrabarthy, A. (2016). Management of
multidrug resistant tuberculosis (MDR-TB) -
Monitoring is the key to successful outcome. Egyptian
Journal of Chest Diseases and Tuberculosis. Volume
65, Issue 2, 1 April 2016, Pages 447-450
Aisyah (2013). Hubungan persepsi, pengetahuan TB
paru dan PMO dengan kepatuhan berobat pasien TB
paru di puskesmas kecamatan Jatinegara Jakarta
Timur. Tesis, FKM-UI
Bildenhann, A. (2015). Assesment of Knowledge and
Attitudes on Latent Tuberculosis Treatment
Acceptance in a South West. Dayton, Ohio:Wright
State Univerity.
Castelnuovo B (2013). A review of compliance to anti
tuberculosis treatment and risk factors for defaulting
treatment in Sub Saharan Africa. African Health
Sciences 2010; 10(4): 320 - 324
Darmadi (2010). Analisis kualitatif perilaku kepatuhan
menelan obat pasien tuberkulosis Paru di 4
Puskesmas Wilayah Kabupaten Ketapang tahun 2000
(http://www.lontar.ui.ac.id//opa
c/themes/libri2/detail.jsp? id=70978 &lokasi=lokal)
akses 30 Juli 2017
Departemen Kesehatan Republik Indonesia. (2008).
Pedoman Nasional Penanggulangan TBC. Jakarta:
Bhakti Husada.
Dhewi, G. I., Armiyati, Y., & Supriyono, M. (2011).
Hubungan Antara Pengetahuan, SIkap Pasien dan
Dukungan Keluarga dengan Kepatuhan Minum Obat
Pada Pasien TB Paru di BKPM Pati. Semarang:
Program Studi S1 Ilmu Keperawatan Stikes
Telogorejo.
Deskhmund, RD, Caroline, MD. & Nutherford, LS.
(2017). Social support a key factor for adherence to
multidrug-resistant Tuberculosis treatment.
http://dx.doi.org /10.1016./j.itjb.2017.05.03
Farmani, P. (2015). Prediktor Ketidakpatuhan Minum
Obat Tuberkulosis (TB) pada Pasien dengan
Pengobatan Kategori 1 di Puskesmas Kota Denpasar
pada Tahun 2011-2012. Denpasar: FK Unud
Hendiani, N., Sakti, H. & Widayanti, C. G. (2012). The
relationship between perceived family support as drug
consumption controller/ pengawas minum obat
(PMO)’s and self-efficacy of tuberculosis patients in
BPKM Semarang region. Jurnal Psikologi, Vol. 1 (1)
94-105
Hidayati, L. (2012). Pengaruh hypertension self-
management program terhadap perubahan self-
efficacy, self-care behaviour dan tekanan darah
penderita hipertensi di puskesmas Mojo. Tesis.
Universitas Airlangga.
Hutapea. (2009). Pengaruh dukungan keluarga terhadap
kepatuhan minum OAT. Jurnal Respirologi Indonesia.
29 (2).
Kementerian Kesehatan RI. (2016). Petunjuk Teknis
Manajemen Dan Tatalaksana TB Anak.Jakarta:
Kementerian Kesehatan RI.
Family Support, Self-efficacy, Motivation, and Treatment Adherence in Multidrug-resistant Tuberculosis Patients
181

Kholifah, S.N. (2014). Self-management intervention
sebagai upaya peningkatan kepatuhan pada
penderita DM. Jurnal Ners, Vol. 9 (1) 143-150.
Maulidia, DF. (2014). Hubungan Antara Dukungan
Keluarga dan Kepatuhan Minum Obat Pada Pasien
Tuberkulosis di Ciputat (Skripsi). Jakarta: UIN
Mohammadi, E., Abedi, H.A., Gofranipour, E., Jalali, F &
Kazemnejad, A. (2009). Evaluation of 'partnership
care model' in the control of hypertension.
International Journal of Nursing Practice, 12, 153-
159.
Muhtar (2013). Pengaruh pemberdayaan keluarga dalam
meningkatkan self-efficacy dan self-care activity
keluarga dan penderita tuberkulosis paru di kota Bima,
Nusa Tenggara Barat. Tesis, FKp-UNAIR.
Notoatmodjo, S. (2010). Ilmu Perilaku Kesehatan. Jakarta:
Rineka Cipta.
Nursalam. (2013). Metodologi penelitian: Pendekatan
praktis (edisi 3). Jakarta: Salemba Medika
Rekam Medik RSUD Dr. Soetomo. (2017).
Data kejadian TB MDR bulan Juli-September 2016.
Surabaya: RSDS
Royce, S. Carls, F. Bare, T. & Gates, G. (2014)
Identification of Multidrug Resistance in Previously
Treated Tuberculosis Patients: a Mixed Methods
Study in Cambodia. NIH Public Access: Inj.
Tuberculosis Lugn Disease. November; 18(11): 1299–
1306.doi:10.5588/ijtld.14.0116
Sukartini, T. (2015). Pengembangan model peningkatan
kepatuhan. Jakarta: Disertasi. Universitas Indonesia.
Sutarno, S., & Utama, G.A., (2012). Faktor-faktor yang
mempengaruhi motivasi berobat penderita tuberculosis
paru di Pekalongan tahun 2012. Jurnal
Ilmiah Widya, Vol. 1 (1) 2012
Sagbakken, M., Frich, J.C., and Bjune, G (2008). Barrier
and enablers in the management of tuberculosis
treatment in Addis Ababa, Ethiopia: a qualitative
study. BMC Public Health.
(https://bmcpublichealth.biomedcentral.com/articles/1
0.1186/1471-2458-8-11)
WHO. (2016). World statistics of Tuberculose Prevalence.
New York: World Health Organization
Wilson, J.W., Ramos, J.G., Castillo, F., Catellanos, E.F.,
Escalante, P. (2016). Tuberculosis patient and family
education through videography in El Salvador.
Journal of Clinical Tuberculosis and Other
Mycobacterial Diseases. Volume 4, 1 August 2016,
Pages 14-20
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
182
