
Family Knowledge and Attitudes to Improve Medication Adherence
in Patients with Pulmonary Tuberculosis
Lailatun Nimah, Rini Sartika and Makhfudli
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
Keywords: Knowledge, Attitude, Family, Medication Adherence of Pulmonary Tuberculosis.
Abstract: Many Pulmonary Tuberculosis (TB) patients forget to take medication because of lack of support from their
families due to a lack of knowledge and attitude. This study aimed to analyze the relationship between the
knowledge and attitude of families and adherence to taking medication in patients with pulmonary
tuberculosis at Perak Timur Health Center. This is a cross-sectional study. The population of this study
comprised of the families of patients treated at Perak Timur Health Center. The number of research samples
was 110 respondents while for the inclusion criteria, consecutive sampling was used. The dependent
variables were knowledge and family attitude in patients of pulmonary TB, while the independent variable
was medication adherence in TB patients. Data were collected using questionnaires. The data were analyzed
using Spearman. Results indicated that a correlation between family knowledge and TB medication
adherence (p = 0,000) with contingency coefficient (C) = 0,655. Family attitudes and medication adherence
of pulmonary tuberculosis patients (p=0,000) with contingency coefficient (C) = 0.926. It can be concluded
that there is a relationship between the knowledge and attitude of families and compliance in taking
medication in patients of TB. Family knowledge and attitude is good in relation to medication adherence.
Researchers are further advised to examine the analysis of factors related to adherence in taking pulmonary
TB Medication. Suggestions can be made for education about pulmonary TB, especially regarding disease
transmission, accuracy in taking medication, and time to take medication for TB patients.
1 BACKGROUND
Tuberculosis (TB) is a contagious infectious disease
caused by the bacterium Mycobacterium
Tuberculosis that can attack various organs,
especially the lungs (Depkes RI, 2016). Pulmonary
tuberculosis (TB) is a curable disease but many
patients stop treatment prematurely. TB patients
often discontinue their own treatment if they feel the
symptoms of the disease have been lost or reduced.
Many factors that affect the success of TB treatment
include regular medicine taking, family support,
community, social stigma, level of knowledge, and
environment. Non-adherence to TB treatment is
significantly associated with unemployment, low
status occupation, low annual income and cost of
travel to the TB treatment facility (Ii & Urin, 2007).
Pulmonary tuberculosis problems are a challenge
for countries all over the world. TB incidences from
year to year are increasing (WHO, 2017). The World
Global Tuberculosis Report says Indonesia ranks
second with the highest number of tuberculosis cases
in the world. The number of pulmonary TB patients
in Indonesia by 2016 was 156,723 people, those who
completed treatment was 11,427 (6.1%) and those
who experienced successful treatment was 141,980
(75.4%) (WHO, 2017). The incidences of confirmed
pulmonary TB in Indonesia rose significantly from
7% in 1999 to 13% in 2003. This indicator decline
from 2003 to 2014 but by 2015 had increased again
to 14% (Depkes RI, 2016).
All patients who have not been treated
previously, and do not have other risk factors for
drug resistance, should receive a WHO-approved
first-line treatment regimen using quality assured
drugs. The initial phase should consist of two
months of isoniazid, rifampicin, pyrazinamide, and
ethambutol. The continuation phase should consist
of isoniazid and rifampicin given for four months.
Doses of antituberculosis drugs should conform to
WHO recommendations. Fixed-dose combination
drugs may provide a more convenient form of drug
administration (TB Care I & United States Agency
for International Development, 2014).
Nimah, L., Sartika, R. and Makhfudli, .
Family Knowledge and Attitudes to Improve Medication Adherence in Patients with Pulmonary Tuberculosis.
DOI: 10.5220/0008319900290032
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 29-32
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
29
The duration of treatment in patients with
pulmonary TB greatly affects adherence of patients
in taking the drug. Poor treatment, heavy financial
burden (Lei et al., 2016), illiteracy, being divorced
or widowed, lacking health insurance and being
migrants (Xu et al. 2009) are factors of non-
adherence therapy. Family support is indispensable
in the treatment of pulmonary TB patients. One
fundamental principle of the Family Health Strategy
is to build bonds between the health team and the
referred community and to maintain the care offered
to individuals and families over time, through a
proactive attitude in view of health-disease problems
(de Souza et al., 2010).
2 METHODS
The method used in this research is cross sectional
with the population being the families of lung
tuberculosis patients at Perak Timur Health Center.
The sample comprises of families of patients with
pulmonary TB, who were seeking treatment at Perak
Timur Health Center and undergoing treatment of
anti-tuberculosis drug from October 23 to November
11, 2017. Inclusion criteria are: 1. Families who care
for patients with pulmonary TB who are undergoing
anti-tuberculosis drug treatment; 2. Families, caring
for pulmonary TB patients, who can read and write;
3. Families who have become drug supervisors; 4.
Patients who have had pulmonary TB for more than
15 years; and 5. TB patients who can read and write.
Exclusion criteria are: 1. TB patients who have
accompanying diseases such as diabetes mellitus,
hypertension, and others; and 2. Patients’ family
members aged less than 18 years. Total sampling is
used for this research. The number of samples in this
study comprised of 110 respondents. Independent
variables are the knowledge and attitude of the
family. The dependent variable is medication
adherence in patients with pulmonary TB. The
ethical clearance was conducted at the Faculty of
Nursing of Airlangga University and was approved
on November 6, 2017 with the certificate number
553-KEPK.
Samples were collected using consecutive
sampling and data were collected using
questionnaires. Questions in the questionnaire were
in four parts: 1. Demographic data including age,
education and gender; 2. Family knowledge about
TB consisting of 12 closed questions; 3. Family
attitudes toward pulmonary TB patients comprising
12 questions; and 4. Patient adherence to taking
pulmonary TB drugs, comprising four closed
questions. Data analysis of the knowledge level and
attitude of family regarding medication compliance
was done using the Spearman Rank statistic test.
3 RESULTS
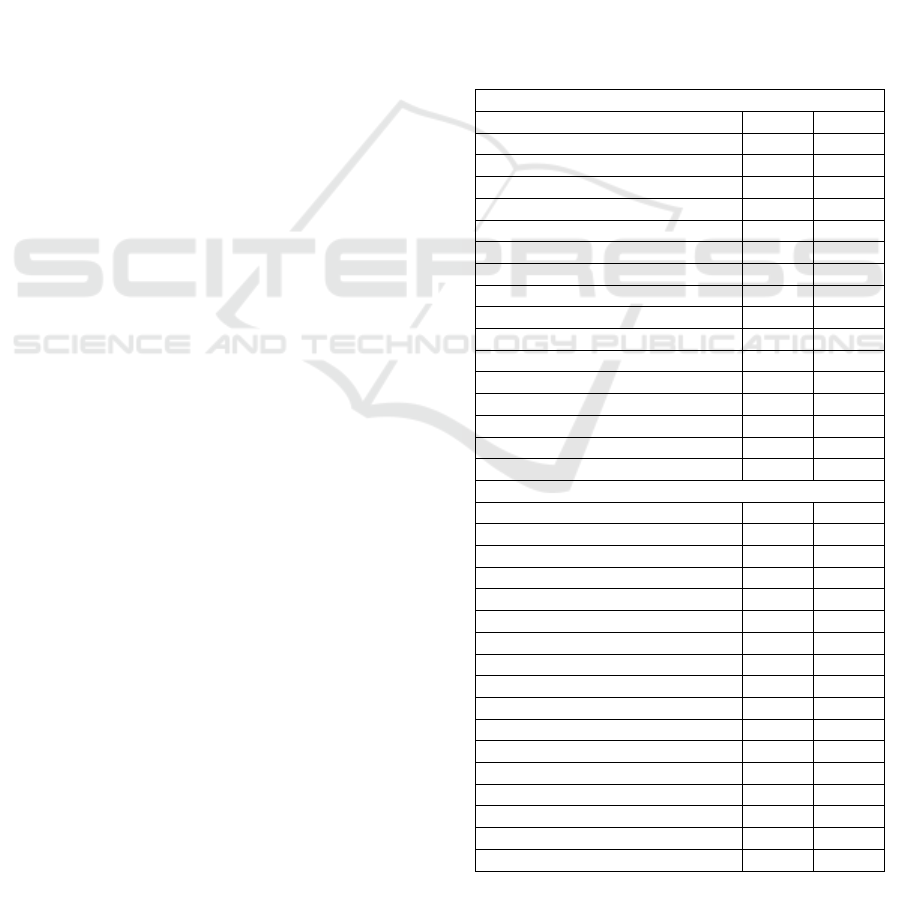
The table shows that most of the families that care
for patients include working women with their most
recent education in elementary school and aged
between 18 and 65 years. Characteristics of patients
based on Table 1 are mostly male with a recent
primary school education, all aged 18–65 years, and
mostly employed.
Table 1: Family and patient demographic
characteristic data.
Characteristic Famil
y
Gende
r
f %
Male 45 40.9
Female 65 59.1
Total 110 100
Last education f %
Elementar
y
School 45 40.9
Junior Hi
g
h School 21 19.1
Senior High School 44 40
Total 110 100
A
g
ef %
18
–
65
y
ears 110 100
66
–
79
y
ears 0 0
Total 110 100
Work f %
Employee 92 83.6
Unem
p
lo
y
ment 18 16.4
Total 110 100
Patient
Gende
r
f %
Male 57 51.8
Female 53 48.2
Total 110 100
Last education f %
Elementary School 47 42.7
Junior High School 24 21.8
Senior High School 39 35.;5
Total 110 100
A
g
ef %
18
–
65
y
ears 101 91.8
66
–
79 years 9 8.2
Total 110 100
Work f %
Em
p
lo
y
ee 62 56.4
Unem
p
lo
y
ment 48 43.6
Total 110 100
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
30
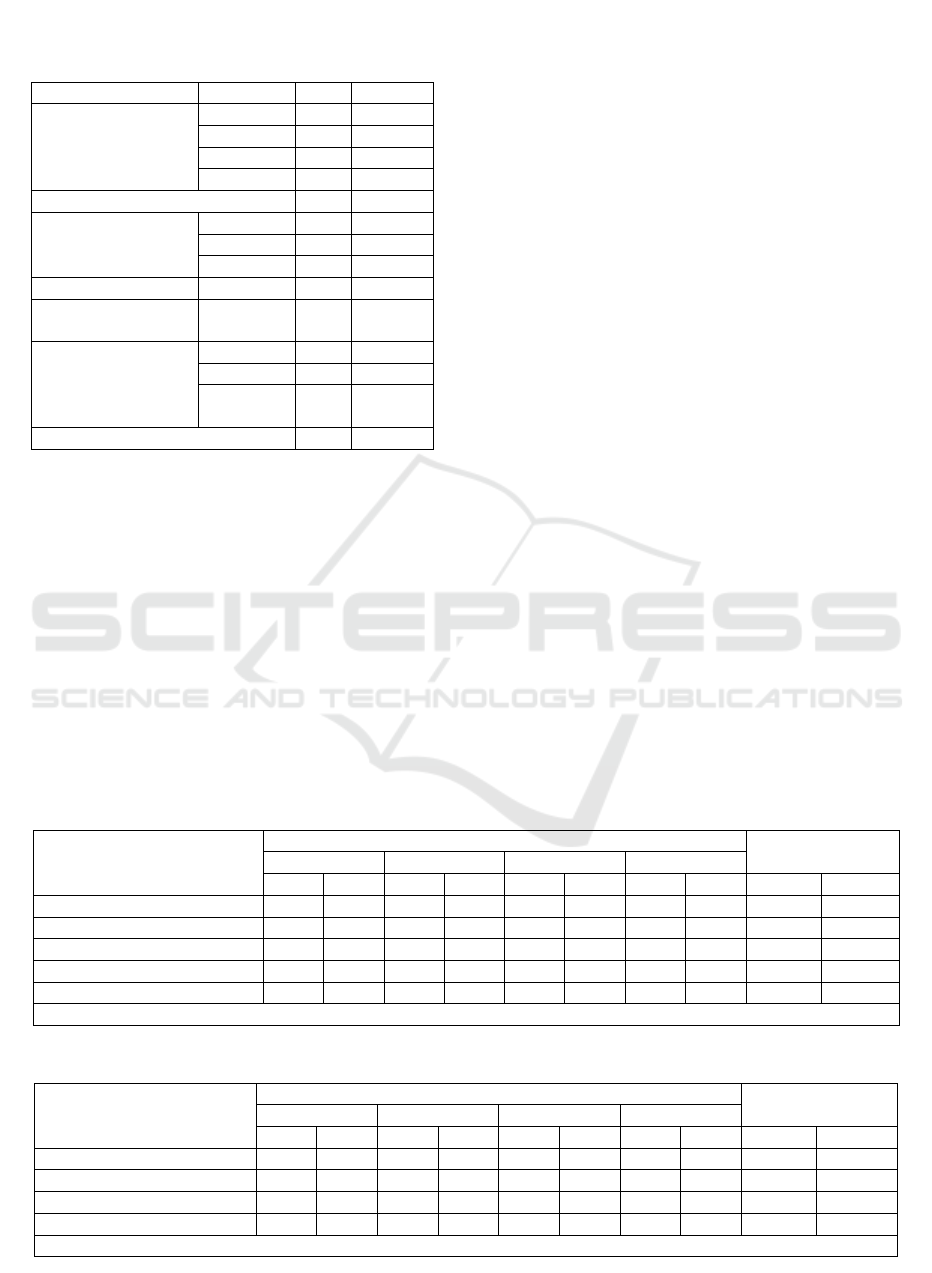
Table 2 shows that most families of TB patients
have sufficient knowledge about TB (as many as 68
people or 61.8%. Family attitudes to TB patients are
mostly good (as many as 70 people or 63.6%). For
medication adherence in patients with lung TB, there
are 73 respondents or 66.4%.
Table 3 shows that ‘much less’ family
knowledge in correlation with less medication
adherence equate to two respondents or 1.8%.
‘Enough’ family knowledge correlates with good
medication adherence at 50 respondents or 45.5%.
The Spearman Rank test showed p = 0.000 with
contingency α < 0.05.
Table 4 shows that ‘enough’ family attitude
correlates with ‘enough’ medication adherence with
30 respondents or 27.3%. A ‘good’ family attitude
correlated with ‘very good’ medication adherence
with just one respondent or 0.9%. The Spearman
Rank test shows p = 0.000 with contingency α <
0.05, at 0.926.
4 DISCUSSION
Family knowledge of pulmonary TB patients at
Perak Timur Health Center is largely adequate. The
compliance of treatment of pulmonary TB patients at
Perak Timur Health Center is good. Sufficient
family knowledge has good medication adherence.
The results of statistical tests show that family
knowledge has a strong relationship with the need
for taking medication in patients with pulmonary TB
at in Perak Timur Health Center.
Family attitudes towards of pulmonary TB
patients at the Perak Timur Health Center is mostly
good. The compliance of patients taking medicine at
Perak Timur Health Center attitudes of patients with
pulmonary TB makes the TB medication adherence
good. Good family attitudes are related to
medication adherence in patients with pulmonary
TB in East Perak Surabaya Public Health.
The success of pulmonary TB lung treatment is
not only the responsibility of the patient, but other
factors that influence family support and family
Table 2: Family knowledge about tuberculosis, family
attitude to TB patients, medication adherence in
patients with lung tuberculosis.
Variable Cate
g
or
y
f %
K
nowledge Much less 2 1.8
Less 16 14.5
Enough 68 61.8
Goo
d
24 21.8
Total 110 100
Attitude Less 6 5.5
Enough 34 30.9
Goo
d
70 63.6
Total 110 100
Medication
Adherence
Less 6 5.5
Enough 30 27.3
Goo
d
73 66.4
Very
goo
d
1 0.9
Total 110 100
Table 3: Relationship of family knowledge with medication adherence in pulmonary tuberculosis patients.
Family Knowledge Medication Adherence Total
Less Enou
g
hGoo
d
Ver
y
g
oo
d
f % F % F % f % f %
Much less 2 1.8000000 2 1.8
Less 4 3.61210.90000 16 14.5
Enough 0 0 18 16.4 50 45.5 0 0 68 61.8
Goo
d
0 0 0 0 23 20.9 1 0.9 24 21.8
Total 6 5.5 30 27.3 73 66.4 1 0.9 110 100
S
p
earman Rank Test
p
=0.000, contin
g
enc
y
coefficient
(
C
)
= 0.655
Table 4: Relationship of family attitude with medication adherence in pulmonary TB patients.
Family Attitude Medication Adherence Total
Less Enou
g
hGoo
d
Ver
y
g
oo
d
f % F % f % f % f %
Less 6 5.5 000000 6 5.5
Enough 0 0 30 27.3 4 3.6 0 0 34 30.9
Goo
d
0 0 0 0 69 62.7 1 0.9 70 63.6
Total 6 5.5 30 27.3 73 66.4 1 0.9 110 100
S
p
earman Rank Test
p
= 0.000, contin
g
enc
y
coefficient
(
C
)
= 0.926
Family Knowledge and Attitudes to Improve Medication Adherence in Patients with Pulmonary Tuberculosis
31

behavior during treatment must be considered.
Families with good knowledge encourage patients to
be obedient during treatment because they know the
consequences of non-compliance. Family knowledge
support is essential for the healing and recovery of
patients.
Family knowledge affects medication adherence
of patients with pulmonary TB because with good
knowledge a family can supervise medicine taking
to ensure the schedule and doses the patient is
drinking are appropriate. Good family knowledge
can also prevent transmission to other family
members and avoid drug withdrawal.
The results are in accordance with factors of
medication adherence in TB patients, such as lost
access to essential financial and practical support
over time, often because relatives and friends are
financially and socially exhausted by supporting
them (Sagbakken et al., 2008). Other research states,
that non-adherence in medication patients in
Pakistan was associated with stigma, experience of
direct observation, social support received from the
family, and reasons for stopping treatment early
(Khan et al., 2005). Personal situations, including
related factors to medication adherence, are
accommodation, unemployment, and nutritional
requirements; knowledge about tuberculosis
comprises of causes, treatment, and prevention,
which are crucial for adherence to treatment (Akeju
et al., 2017).
5 CONCLUSIONS
Most family members who regulate patients with
tuberculosis are women. This is because women are
more conscientious and more attentive to family
members. The age of family members who treat
patients with TB is a productive age, so the ability to
care for family members has more leverage. Most of
the educational levels of family members who care
for TB patients are elementary and high school. This
indicates the level of knowledge of family members.
There is a relationship between family
knowledge and medication adherence in patients
with pulmonary TB at East Surabaya Perak Health
Center. Family members who have a high level of
education improve patient compliance with TB
medication because family members understand the
impact if the patient does not fully take the medicine
and the risks of recurrence, transmission, and drug
resistance OAT will be higher.
There is a relationship between family attitudes
and medication adherence in patients with
pulmonary TB at East Surabaya Perak Health
Center. Family members who have a positive
attitude will provide support to patients with
tuberculosis regarding treatment. Family members
will accompany p in treatment and provide
motivation to TB patients.
REFERENCES
Akeju, O.O., Wright, S.C.D. & Maja, T.M., 2017. Lived
experience of patients on tuberculosis treatment in
Tshwane, Gauteng province. Health SA Gesondheid,
22, pp.259–267. Available at:
http://dx.doi.org/10.1016/j.hsag.2017.03.001.
Depkes RI, 2016. InfoDatin. Tuberkulosis temukan obati
sampai sembuh, pp.2–10.
Ii, B.A.B. & Urin, A.K., 2007. Pengaruh Teknik
Relaksasi...,Bayu Purnomo Aji,Fakultas Ilmu
Kesehatan UMP,2017. , pp.8–19.
Khan, M.A. et al., 2005. Tuberculosis patient adherence to
direct observation: Results of a social study in
Pakistan. Health Policy and Planning, 20(6), pp.354–
365.
Lei, X. et al., 2016. Are tuberculosis patients adherent to
prescribed treatments in China? Results of a
prospective cohort study. Infectious Diseases of
Poverty, 5(1), p.38. Available at:
http://idpjournal.biomedcentral.com/articles/10.1186/s
40249-016-0134-9.
Sagbakken, M., Frich, J.C. & Bjune, G., 2008. Barriers
and enablers in the management of tuberculosis
treatment in Addis Ababa, Ethiopia: A qualitative
study. BMC Public Health, 8, pp.1–11.
de Souza, K.M.J. et al., 2010. Tuberculosis treatment drop
out and relations of bonding to the family health team.
Revista da Escola de Enfermagem da U S P, 44(4),
pp.904–911. Available at:
http://www.ncbi.nlm.nih.gov/pubmed/21337770.
TB Care I & United States Agency for International
Development, 2014. International Standards for
Tuberculosis Care. TB Care I & USAID, p.92.
Available at: http://www.tbcare1.org/publications.
WHO, 2017. Global Tuberculosis Report 2017: Leave no
one behind - Unite to end TB, Available at:
http://www.who.int/tb/publications/global_report/gtbr
2017_main_text.pdf?ua=1.
Xu, W. et al., 2009. Adherence to anti-tuberculosis
treatment among pulmonary tuberculosis patients: A
qualitative and quantitative study. BMC Health
Services Research, 9, pp.1–8.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
32
